Update of Canada’s Low-Risk
Alcohol Drinking Guidelines:
Final Report for Public
Consultation
This document was published by the Canadian Centre on Substance Use and Addiction
(CCSA).
Suggested citation: Paradis, C., Butt, P., Shield, K., Poole, N., Wells, S., Naimi, T., Sherk, A., &
the Low-Risk Alcohol Drinking Guidelines Scientific Expert Panels. (2022). Update of Canada’s
Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation. Ottawa, Ont.:
Canadian Centre on Substance Use and Addiction.
© Canadian Centre on Substance Use and Addiction, 2022.
CCSA, 500–75 Albert Street
Ottawa, ON K1P 5E7
613-235-4048
Production of this document has been made possible through a financial contribution from
Health Canada. The views expressed herein do not necessarily represent the views of Health
Canada.
This document can also be downloaded as a PDF at www.ccsa.ca
Ce document est également disponible en français sous le titre :
Le projet d’actualisation des Directives de consommation d’alcool à faible risque du Canada :
rapport final pour consultation publique
ISBN 978-1-77178-994-3

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances
Table of Contents
Public Summary .......................................................................................................... 1
Technical Summary ..................................................................................................... 2
Aim and Approach 2
Risk Associated with Various Levels of Alcohol Use 3
Risk Associated with Each Occasion of Alcohol Use 4
Risk for Men 4
Risk for Women 4
Risk for Women Who Are Pregnant or Breastfeeding ....................................... 4
Risk for Men and Women 5
Reasons for the New Guidance on Alcohol and Health 5
Alcohol and Cancer .......................................................................................... 5
Alcohol and Heart Disease ................................................................................ 5
Alcohol and Violence ....................................................................................... 5
Policy Implications 6
Technical Report ......................................................................................................... 7
Introduction 7
Awareness and Adherence to the 2011 LRDGs of People Living in Canada 7
Time to Update 8
Aim and Scope of This Report 9
Part 1: Development of Experts’ Recommendations ................................................... 9
1.1 Defining Research Questions 10
1.2 Estimating the Lifetime Risk of Alcohol-Related Death and Disability in the
Canadian Population 10
1.3 The Evidence Base for Updating the Guidelines 11
Part 2: Evidence Used to Construct the Recommendations ....................................... 13
2.1 Global Evidence Review on the Effects of Alcohol on Health 13
2.1.1. Methods ................................................................................................ 13
2.1.2 Results .................................................................................................... 15
2.1.3 Implications ............................................................................................ 16

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances
2.2 Mathematical Modelling of the Lifetime Risk of Death for Various Levels of
Average Alcohol Consumption 16
2.2.1 Methodological Principles ..................................................................... 17
2.2.2 Results and Implications ......................................................................... 18
2.3 Alcohol Use per Occasion 23
2.4 Rapid Reviews 24
2.4.1 Association Between Alcohol Use, Aggression and Violence ................. 24
2.4.2 Association Between Alcohol Use and Mental Health ............................. 27
2.5 Women’s Health and Alcohol 28
2.5.1 What Are Some Sex-Related Factors? .................................................... 28
2.5.2 What Are Some Gender-Related Factors? .............................................. 28
2.5.3 How Do Sex and Gender Interact and Intersect with Other Factors? ...... 29
2.5.4 How Does Alcohol Affect Reproduction? ................................................ 29
2.5.5 Discussion .............................................................................................. 29
2.5.6 What Are the Key Messages for Women? ............................................... 30
2.6 Views, Preferences and Expectations About Guidelines of People Living in
Canada 30
2.6.1 Summary of Evidence on Understanding and Response to Alcohol
Guidelines ...................................................................................................... 30
2.6.2 Public Consultation on Alcohol Guidelines ............................................ 31
2.6.3 Interviews with Stakeholders ................................................................. 32
2.6.4 Focused Consultations with Indigenous People ..................................... 34
Part 3: Experts’ Recommendations ........................................................................... 36
3.1 Canada’s Guidance on Alcohol and Health 36
3.2 Moving Forward 39
3.2 Conclusion 40
References ................................................................................................................ 41
Appendix 1 ............................................................................................................... 50
Lifetime Risk of Alcohol-Attributable Death and Disability: Shadow Analysis 50
Purpose .......................................................................................................... 50
Method ........................................................................................................... 50
Summary of the Comparison of Findings ........................................................ 50
Appendix 2 ............................................................................................................... 53
Appendix 3 ............................................................................................................... 57

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances
Acknowledgements
The Canadian Centre on Substance Use and Addiction (CCSA) would like to extend its appreciation
and gratitude to members of the Low-Risk Alcohol Drinking Guidelines Scientific Expert Panels for
their expertise, guidance and other invaluable contributions (in alphabetical order):
Co-chairs for the project:
• Catherine Paradis, Canadian Centre on Substance Use and Addiction
• Peter Butt, College of Medicine, University of Saskatchewan
Members:
• Mark Asbridge, Dalhousie Medical School
• Danielle Buell, University of Toronto
• Samantha Cukier, Health Canada
• Francois Damphousse, Health Canada
• Jennifer Heatley, Public Health at Government of Nova Scotia
• Erin Hobin, Public Health Ontario
• Harold R. Johnson, Lawyer and Author
1
• Ryan McCarthy, Canadian Centre on Substance Use and Addiction (co-chair for the Knowledge
Mobilization Scientific Expert Panel)
• Kate Morissette, Public Health Agency of Canada
• Chris Mushquash, Lakehead University
• Daniel Myran, Ottawa Hospital Research Institute
• Tim Naimi, Canadian Institute for Substance Use Research, University of Victoria
• Nancy Poole, Centre of Excellence for Women's Health
• Justin Presseau, Ottawa Hospital Research Institute
• Adam Sherk, Canadian Institute for Substance Use Research, University of Victoria
• Kevin D. Shield, Institute for Mental Health Policy Research, Centre for Addiction and Mental Health
• Tim Stockwell, Canadian Institute for Substance Use Research, University of Victoria
• Sharon Straus, University of Toronto
• Kara Thompson, St. Francis Xavier University
• Samantha Wells, Institute for Mental Health Policy Research, Centre for Addiction and Mental Health
1
Harold R. Johnson passed away during the development of this report. We greatly appreciate his important contributions to this process,
and we extend our sincere condolences to his family and friends.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances
• Matthew Young, Gambling Research Exchange Ontario, Carleton University, and the Canadian
Centre on Substance Use and Addiction
The following members and their colleagues also led the production of reports and reviews that
informed the update of the 2011 LRDGs (in alphabetical order):
• Sam Churchill, Adam Sherk and Tim Naimi: Lifetime Risk of Alcohol-Attributable Death and
Disability: Shadow analysis
• Tim Naimi. Per occasion alcohol use
• Nancy Poole and Lorraine Greaves: Sex, Gender and Alcohol: What Matters for Women in Low-
Risk Drinking Guidelines?
• Nancy Poole and Lorraine Greaves: Specific messages for girls and women to supplement the
Guidance on Alcohol and Health
• Kevin Shield: Lifetime Risk of Alcohol-Attributable Death and Disability
• Kathryn Graham, Bryan Tanner, Jesus Chavarria, Tavleen Dhinsa, Jean Francois Crépault and
Samantha Wells: Association Between Alcohol Use and Aggression and Violence: A Rapid
Overview of Reviews to Inform Canada’s Low-Risk Alcohol Drinking Guidelines
The project has also benefited from the efforts and contributions of the following organizations and
individuals (in alphabetical order):
• Autrement Dit: Plain language summary of the Guidance on Alcohol and Health
• Cochrane Canada: Update of a Systematic Review of the Effect of Alcohol Consumption on the
Development of Depression, Anxiety and Suicidal Ideation
• Cochrane Canada: Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Summary of
Evidence on Understanding and Response to Alcohol Consumption Guidelines
• Christine Levesque, Nitika Sanger and Hanie Hadelati: Assistance in all aspects of the evidence
review portion of this project
• Jennifer Reynolds for her assistance in overseeing the first public consultation and the
stakeholder’s consultations
• Lauren Levett, Scott Hannant, Christina Davies, Wendy Schlachta, Manon Blouin, Patricia-Anne
Croteau, John Thurston, Virginia St-Denis, Ahmer Gulzar, Lili Yan and Victoria Lewis: Assistance
with project management, communications, editing, translation and other support throughout
the project
In addition, CCSA would like to thank members of the Low-Risk Alcohol Drinking Guidelines Executive
Committee who generously contributed their time and expertise throughout this project (in
alphabetical order):
Co-chairs:
• Shannon Nix, Health Canada
• Rita Notarandrea, Canadian Centre on Substance Use and Addiction

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances
Members:
• Ally Butler, Substance use and Strategic Initiatives, Government of British Columbia
• Ian Culbert, Canadian Public Health Association
• Scott Hannant, Canadian Centre on Substance Use and Addiction
• Carol Hopkins, Thunderbird Partnership Foundation
• Jennifer Saxe, Health Canada
• Candice St-Aubin, Public Health Agency of Canada
• Robert Strang, Council of Chief Medical Officers of Canada
• Sam Weiss, Canadian Institute of Health Research
Conflict of Interest
The list of potential conflicts of interest is available on CCSA’s website: Disclosure of Affiliations and
Interests.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances
About this Document
This report contains three documents produced for three different target groups.
Public Summary
The Public Summary is a one-page summary intended for the general public.
Technical Summary
The Technical Summary is intended for health organizations, health professionals (e.g., physicians,
nurses, counsellors) and people who would like to learn about the update of the Low-Risk Alcohol
Drinking Guidelines, its key takeaways, the risks associated with alcohol and the implications.
Technical Report
The Technical Report is intended for alcohol scientists, policy makers and healthcare professionals
who are interested in understanding the detailed process followed, the types of evidence and the
way they were used to update the Low-Risk Alcohol Drinking Guidelines.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 1
Public Summary

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 2
Technical Summary
Alcohol is a legal psychoactive substance used by about three-quarters of people living in Canada.
For some, alcohol use is intertwined with their lifestyle. It is often used in connection with social
events or to mark special occasions. However, alcohol can cause harm to the person who drinks and
sometimes to others around them. Few people recognize that alcohol is a leading preventable cause
of death and disability, injuries, accidents and social problems. In 2017, alcohol contributed to
18,000 deaths in Canada. That same year, the costs associated with alcohol use in Canada were
$16.6 billion, with $5.4 billion of that sum spent on health care.
Aim and Approach
Canada’s Guidance on Alcohol and Health is informed by a public health perspective. It is intended
to replace Canada’s Low-Risk Alcohol Drinking Guidelines. Its stated focus is to provide people living
in Canada with accurate and current information about the risks and harms associated with the use
of alcohol. The guidance should help people to make well-informed and responsible decisions about
their alcohol consumption.
A fundamental idea underlying this project is that people living in Canada have a right to know.
The Guidance on Alcohol and Health is also intended to form the evidence base for future alcohol
policy and prevention resources, with a view to changing Canada’s drinking culture and curbing the
normalization of harmful alcohol use in society.
The production of the new guidance followed a rigorous and transparent approach to assess the
impact of various levels of alcohol use on deaths and disabilities. The analyses were based on the
Canada’s Guidance on Alcohol and Health
Canada’s Guidance on Alcohol and Health consists of seven key takeaways:
1. All levels of alcohol consumption are associated with some risk, so drinking less is better for
everyone.
2. Among healthy individuals, there is a continuum of risk for alcohol-related harms where the
risk is:
• Negligible to low for individuals who consume two standard drinks or less per week;
• Moderate for those who consume between three and six standard drinks per week; and
• Increasingly high for those who consume more than six standard drinks per week.
3. On any occasion, any level of consumption has risks, and with more than two standard drinks,
most individuals will have an increased risk of injuries or other problems.
4. Disproportionately more injuries, violence and deaths result from men’s drinking.
5. Above low levels of alcohol consumption, the health risks increase more steeply for women
than for men.
6. It is safest not to drink while pregnant and during the pre-conception period.
7. For women who are breastfeeding, it is safest not to use alcohol.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 3
most recent data and methods, which have evolved since the Low-Risk Alcohol Drinking Guidelines
were released over a decade ago.
Risk Associated with Various Levels of Alcohol Use
Throughout the life course, there are established thresholds of mortality risk that people are willing
to accept. For involuntary risks such as air pollution, a 1 in 1,000,000 lifetime mortality risk has
been used as a gold standard. That is, people are willing to accept a 1 in 1,000,000 risk of death
when exposed to these risks. For risks associated with activities that people undertake deliberately
and from choice, such as unprotected sexual practices, smoking and so on, people may accept risks
about 1,000 times greater. Hence, advice and recommendations made to people about voluntary
activities use a 1 death in 1,000 lifetimes cut point. However, for drinking alcohol, it is not unusual
for guidelines to be based on a risk threshold 10 times greater, which is a 1 in 100 mortality risk.
Hence, there is a continuum of risk whereby the risk for those who consume two standard drinks or
less per week is negligible to low; it is moderate for those who consume between three and six
standard drinks per week; and it is high for those who consume above six standard drinks per week,
with increasingly higher levels of risk with every additional drink.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 4
Risk Associated with Each Occasion of Alcohol Use
On any drinking occasion, the risk of acute outcomes such as unintentional injuries and violence is
strongly associated with consuming larger amounts of alcohol and a reduced ability to think clearly
or perform certain activities (i.e., is caused by alcohol impairment). The risk of negative outcomes
begins to increase with any consumption, and with more than two standard drinks, most
individuals will have an increased risk of injuries or other problems.
Binge drinking, usually defined as consuming five standard drinks or more for men, or four standard
drinks or more for women in one setting, is a pattern of consumption that results in legal impairment
for most people. It is a well-established risk factor for death from any cause, including unintentional
injuries, violence, heart disease and high blood pressure, inflammation of the gastrointestinal
system, and the development of an alcohol use disorder (i.e., alcohol dependence).
Many of the complications arising from acute impairment and binge drinking involve second-hand
effects that affect someone other than the person who drinks alcohol (e.g., violence, child abuse and
neglect).
Risk for Men
Men drink more alcohol than women do and are more likely to drink in excess. As a consequence,
they are more likely to be involved in alcohol-impaired driving collisions, to be treated in hospitals
and hospitalized for alcohol-related medical emergencies and health problems, to be diagnosed with
an alcohol use disorder, and to die from alcohol-related causes. Alcohol is also more strongly
associated with perpetration of violence for men than for women.
Men are also more likely than women to take other risks (e.g., use other substances, drive under the
influence) that when combined with alcohol further increase their likelihood of experiencing and
causing alcohol-related harms. Overall, disproportionately more injuries, violence and deaths
result from men’s drinking.
Risk for Women
The physiological differences between women and men have only a small impact on lifetime risk of
death. However, it is unequivocal that above low levels of consumption, lifetime risk of health
harms increases more steeply for women than for men. Enzymes, genes, body weight and size,
organ function and metabolism are important in processing alcohol and are affected by sex-related
factors. These biological factors enhance the impact of alcohol on females, causing faster
intoxication, more risk for disease (including breast cancer), and more long-term harm (such as liver
damage and injury) on lesser amounts.
Risk for Women Who Are Pregnant or Breastfeeding
Reproductive health is compromised by alcohol use. In general, there is mixed evidence on the
impact of alcohol on pregnancy and delivery outcomes, with possible increases in miscarriage,
hypertensive disorders of pregnancy and placental abnormalities.
Alcohol is a teratogen or agent that can cause malformation of the fetus. It can lead to learning,
health and social effects with lifelong impacts, including brain injury, birth defects, behavioural
problems, learning disabilities and other health problems. These adverse effects are also observed
at relatively low levels of exposure or short-term exposure to high levels of consumption. For this
reason, it is safest to not to drink at all while pregnant and during the pre-conception period.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 5
Alcohol consumption can also negatively impact breastfeeding by causing a decrease in milk
production, early cessation of breastfeeding and effects on infant sleep patterns. Moreover, alcohol
enters breast milk through passive diffusion meaning that breastfeeding infants, who are unable to
metabolize alcohol, can be exposed to it. Therefore, for women who are breastfeeding, no alcohol
use is safest for the baby.
Risk for Men and Women
Alcohol use is influenced by many gender-related factors, including alcohol marketing tactics, gender
roles, attitudes and expectations. As a consequence, many harms from alcohol use are gender-
related, including stigma, sexual assault and intimate partner violence.
Reasons for the New Guidance on Alcohol and Health
Alcohol and Cancer
Cancer is the leading cause of death in Canada. However, the fact that alcohol is a carcinogen that
can cause at least seven types of cancer is often unknown or overlooked. The most recent
available data show that the use of alcohol causes nearly 7,000 cases of cancer deaths each year in
Canada, with most cases being breast or colon cancer, followed by cancers of the rectum, mouth
and throat, liver, esophagus and larynx. According to the Cancer Society of Canada, drinking less
alcohol is among the top 10 healthy habits to prevent cancer.
Alcohol and Heart Disease
Heart disease is the second leading cause of death in Canada and alcohol is not good for the heart.
For many years, the commonly held belief that drinking in moderation offered protection against
heart disease has been widely publicized. Research in the last decade is more nuanced with the
most recent and highest quality systematic reviews showing that drinking a little alcohol neither
decreases nor increases the risk of heart disease. At higher levels of use, alcohol is a risk factor
for most types of cardiovascular disease, including coronary artery disease and heart attacks, heart
failure, high blood pressure, atrial fibrillation and stroke.
Alcohol and Violence
Alcohol is frequently associated with violent and aggressive behaviour, including intimate partner
violence, male-to-female sexual violence, and aggression and violence between adults. Alcohol can
also increase the severity of violent incidents. No exact dose–response relationship can be
established but consuming alcohol increases the risk of perpetrating alcohol-related violence. Thus.
it is reasonable to infer that individuals can reduce their risk of perpetrating aggressive or violent
acts by limiting their alcohol use. Based on consistent evidence, it is highly likely that avoiding
drinking to intoxication will reduce individuals’ risk of perpetrating alcohol-related violence.
Taken together, overwhelming evidence confirms that when it comes to
drinking alcohol: Less is better.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 6
Policy Implications
To support people living in Canada who will want to drink less, governments —working in close
collaboration with employers, healthcare providers and community stakeholders —need to
implement policies that promote public health. This includes strengthening regulations of alcohol
advertising and marketing, restrictions on the physical availability of alcohol and the adoption of
minimum prices for alcohol.
As a priority, people living in Canada need consistent, easy-to-use information at the point of pour to
track their alcohol use in terms of standard drinks. They also have a right to clear and accessible
information about the health and safety of the products they buy. A direct consequence of the
current project is a recommendation for Health Canada to require, through regulation, the
mandatory labelling of all alcoholic beverages to list the number of standard drinks in a
container, the Guidance on Alcohol and Health, health warnings and nutrition information.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 7
Technical Report
Introduction
Canada’s first Low-Risk Alcohol Drinking Guidelines (LRDGs) were originally published by the
Canadian Centre on Substance Use and Addiction (CCSA) in November 2011 (Butt et al., 2011). The
guidelines were developed by an independent expert working group, with members drawn from
Canadian addiction research agencies. The 2011 LRDGs provided people living in Canada with
advice on how to minimize relative long-term risk of serious diseases caused by the consumption of
alcohol over a number of years (e.g., liver disease, some cancers) and relative short-term risk of
injury or acute illness due to the overconsumption of alcohol on a single occasion (Stockwell et al.,
2012). In addition, specific recommendations were provided for situations and individual
circumstances that are particularly hazardous and for which abstinence or only occasional light
intake was advised (e.g., just before or during pregnancy, teenagers, people on medication). The
guidelines also included tips for safer drinking and the definition of a standard drink. The 2011
LRDGs were a significant step to providing consistent information and messaging for minimizing the
risk associated with drinking alcohol. They have provided the cornerstone for undertaking a variety of
health promotion, prevention and education initiatives across the country (Paradis, 2016).
Still, there were important limitations with the research evidence used developing the 2011 LRDGs.
In the LRDG technical report (Butt et al., 2011), the working group noted the under-reporting of
personal alcohol use in self-reported surveys, the failure to take account of heavy drinking episodes
in many epidemiological studies, the misclassification of former and occasional drinkers as lifetime
abstainers, and the failure to control for confounding effects of personality and lifestyle factors
independent of alcohol. In its quality appraisal, using the AGREE II instrument, the Public Health
Agency of Canada (PHAC) further noted limitations, particularly with respect to the rigour of
development and editorial independence, two domains that did not receive the minimum acceptable
score of 60%. Consequently, the 2011 LRDGs received an overall assessment of 60.7% and so did
not meet the criteria for high quality guidelines. They were recommended for use with modifications,
and since then, it has been known that careful consideration would need to be paid to these
limitations when developing alcohol guidelines.
Awareness and Adherence to the 2011 LRDGs of People
Living in Canada
Since their publication, the 2011 LRDGs have been promoted at varying degrees across the country
and adopted differently by key demographics. In 2012, just a few months after the release of the
guidelines, a national survey indicated that a quarter (26%) of people living in Canada had seen or
heard of the LRDGs. Since then, a few provincial studies have recorded people’s awareness of the
LRDGs. In 2017, Public Health Ontario surveyed 2,000 adults in Ontario aged 19 and older who
consume alcohol and found that less than a fifth (17%) were aware of the 2011 LRDGs (Public
Health Ontario, 2017a). In 2019–2020, the new Canadian Postsecondary Education Alcohol and
Drug Use Survey (CPADS) surveyed students in colleges and universities in Canada about their
knowledge of the 2011 LRDGs (Health Canada, 2021). Not surprisingly, within this young group,
awareness was negligible with only 16% reporting to have heard about the guidelines and less than
a third of those (28%), being able to accurately report what the guidelines were.
A study conducted by Institut national de santé publique du Québec found that 55% of Quebecers
thought the 2011 LRDGs were adequate, while 37% believed they were too high, that is,

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 8
corresponding to larger amounts of alcohol than what they consider to be low-risk drinking (Bergeron
et al., 2020).
According to the most recent data from the
Canadian Alcohol and Drugs Survey Health
Canada, 2019), a majority of people living in
Canada indicated drinking within the 2011
LRDGs. In 2019, 83% of the people aged 15 years
and older who consumed alcohol in the past year
reported to drink within the guidelines for short-
term risk and 77% within those for long-term risk.
While more females than males reported to drink
alcohol within the guidelines for short-term risk
(85% vs 81%), the percentages were similar for
the long-term risk guideline (76% for males vs
78% for females). Young adults between the ages
of 20–24 were less likely than other age groups to
drink within the guidelines. In 2019, three-
quarters (74%) followed the guideline for short-
term risk of injury and harm while 69% reported to
follow the guidelines for long-term health risk.
While the percentages seem to indicate general adhesion to the 2011 LRDGs, the reality may be
otherwise. The CADS estimates are based on the alcohol consumption in the previous seven days,
meaning that people who consumed alcohol in the past year but did not have a drink in the week
preceding the survey are automatically considered as not exceeding the 2011 LRDGs. This seems
very unlikely given Canada’s time out culture where people drink to mark special occasions rather
than on a regular daily basis. In fact, a study conducted in 2015 explored adherence to the LRDGs
while attempting to adjust for the under-reporting of alcohol consumption (Zhao et al., 2015). It was
found that 73% of people living in Canada over the age of 15 followed the weekly limits while 61%
followed the daily limits recommended by the LRDGs. In Ontario, the Public Health Ontario survey
found that 39% of people who used alcohol in the Ontario sample regularly exceeded the LRDG daily
limits and 27% the weekly limits (Public Health Ontario, 2017a). According to CPADS , a majority
(88%) of students who use alcohol reported following the guidelines for long-term risk, but only 36%
indicated drinking within the recommendations for short-term risk (Health Canada, 2021). Zhao and
colleagues (2015) also found that, after adjustment for under-reporting, more than 80% of all drinks
consumed in Canada were consumed in a fashion inconsistent with the LRDGs.
Time to Update
There are no set criteria for updating health guidelines to ensure they remain current and evidence
based, but an update is typically recommended when new evidence is identified that is relevant and
important or could alter current guidelines (Vernooij et al., 2014). Over the last decade, several
reasons that justify an update of the 2011 LRDGs have been identified.
First, knowledge on and estimates of relations between different dimensions of alcohol use and
particular diseases, disorders or injuries have been evolving since 2011. Research now confirms the
importance of alcohol use as a risk factor for an increasing number of diseases including at least
seven types of cancers, dementia and sexually transmitted diseases (International Agency for
Research on Cancer, 2012; Lu et al., 2017; Rehm et al., 2017). Second, more than 50% of alcohol-
attributable cancer deaths in Canada are among former alcohol users and people using alcohol
Canada’s 2011 LRDGs
The 2011 LRDGs recommended to reduce:
• Long-term health risk by drinking no
more than 10 standard drinks a week for
women, with no more than two drinks a
day most days, or 15 standard drinks a
week for men, with no more than two
drinks a day most days.
• Short-term risk of injury and harm by
drinking no more than three standard
drinks for women or four standard drinks
for men on any single occasion.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 9
within the 2011 LRDGs for long-term risks (Sherk et al., 2020). People living in Canada who use
alcohol within the LRDG’s weekly limits also account for 65% of hospital stays due to unintentional
injuries and a substantial percentage of deaths due to digestive conditions (18%) and injuries (40%),
suggesting that reducing the burden of disease requires revising the 2011 LRDGs (Sherk et al.,
2020). Third, countries like the United Kingdom, France, Denmark, Holland and Australia recently
reviewed new evidence on alcohol and health and released updated guidelines with limits
significantly different from the 2011 LRDGs, with weekly limits ranging from the equivalent of 5.2 to
8.3 Canadian standard drinks for women and men alike.
2
Finally, given recent reports on the extent
to which alcohol use causes social problems for individuals other than the drinkers themselves
(Laslett et al., 2019), there has been curiosity as to what alcohol guidelines would be if, in addition
to diseases, disorders and injuries, social and mental health harms were also included.
The Canadian 2011 LRDGs did not include an expiration date but given the limitations and in light of
the new evidence, in early 2019, CCSA, Health Canada, PHAC and members of the Canadian 2011
LRDGs working group engaged in discussions to update the guidelines. In July 2020, Health Canada
confirmed funding to CCSA to update Canada’s LRDGs and make recommendations for knowledge
mobilization to maximize dissemination and application of the updated guidelines. The mandate
specified building on the guidelines from the United Kingdom (U.K. Chief Medical Officers, 2016) and
Australia (National Health and Medical Research Council, 2020), which had provided access to the
underlying evidence base supporting their alcohol guidelines. It was further agreed that CCSA would
be responsible for overseeing and facilitating the updating process. Health Canada would provide
advice, support and guidance through membership on the project’s various committees, plus
administrative support. PHAC would provide methodological advice and support.
Aim and Scope of This Report
In the interests of transparency and because the development of best practices for defining alcohol
drinking guidelines remains a work in progress (Holmes et al., 2019), this report will describe the
updating process, so that others can learn from the Canadian experience. The report is divided into
three main parts:
1. The construction of experts’ recommendations;
2. The evidence used by the experts; and
3. The experts’ recommendations for updated alcohol guidelines in Canada.
Part 1: Development of Experts’ Recommendations
To update the 2011 LRDGs, four committees were convened. An executive committee with members
from federal, provincial and territorial governments, and national organizations was established to
provide project oversight and advice. Three scientific expert panels were established to review the
evidence for updating the guidelines and making recommendations on how best to effectively
mobilize this new knowledge. One panel focused on the impacts of alcohol consumption on physical
health, a second one on the social and mental health effects, and a third on knowledge mobilization.
2
Around the world, what constitutes a standard drink ranges from 8 to 20 g of pure alcohol. In Canada, it is defined as 13.45 grams
(Paula et al., 2020). Some say that Canada’s particular standard drink was chosen because it corresponds to the measure of whisky
traditionally available in Canadian bars (Miller et al., 1991). A more probable reason is that it corresponds to the amount of pure alcohol
contained in 341 ml bottles of 5% beer, which has traditionally been the alcoholic beverage of choice in Canada.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 10
To provide scientific support to members of scientific expert panels (hereafter referred to as the
experts), CCSA further established an internal Evidence Review Working Group responsible for
evaluating and summarizing evidence, leading consultations and conducting new research as
needed.
Members of the executive committee and the experts were required to disclose affiliations and
interest, as per (Schünemann et al., 2013). The list of potential conflicts of interest was published on
CCSA’s website in Disclosure of Affiliations and Interests.
1.1 Defining Research Questions
The general research question underlying the 2011 LRDGs update is: To minimize the risk of
developing alcohol-related physical and mental health disorders and social problems, which level or
pattern of use should be recommended to people living in Canada?
For this question to lead to evidence-based guidelines, three more specific questions were
developed, each one specifying a particular target population, the level of exposure to alcohol and
the type of outcomes being considered. (For more information, see Update of Canada’s Low Risk
Alcohol Drinking Guidelines: Development of Research Questions.) It is these three specific research
questions that have guided this project’s evidence collection, analyses and conclusions:
1. What are the short-term risks and benefits (physical and mental health, and social impact)
associated with varying levels of alcohol consumption (including no alcohol use), in different
contexts, associated with a single episode of drinking in the general population?
2. What are the long-term risks and benefits (physical and mental health, and social impact)
associated with varying levels and patterns of alcohol consumption (including no alcohol
consumption) in the general population?
3. What are the risks and benefits (physical and mental health, and social impact) associated with
varying levels and patterns of alcohol consumption (including no alcohol consumption) during
pregnancy or breastfeeding, for fetal, infant and child development?
The specific questions were formulated to encompass all effects, so that studies focusing on both
positive and negative effects could be identified.
1.2 Estimating the Lifetime Risk of Alcohol-Related Death
and Disability in the Canadian Population
From the outset of this project, there was a common understanding among experts that to update
the 2011 LRDGs, the specific research questions would be answered through mathematical
modelling. Modelling had previously been used to establish the 2011 LRDGs as well as alcohol
guidelines in Australia (National Health and Medical Research Council, 2020), the U.K. (U.K. Chief
Medical Officers, 2016) and France (Santé publique France & Institut national du cancer, 2017).
Moreover, since 2016, the European Union Joint Action on Reducing Alcohol-Related Harm has
recommended the use of cumulative lifetime risk of death from alcohol-related disease or injury as a
common metric for assessing the risks from alcohol at the country level; the metric should also
inform discussions by experts to establish alcohol guidelines (Broholm et al., 2016).
Modelling requires alcohol mortality risk functions for all disease or injury categories causally related
to alcohol consumption. These risk functions can be found in meta-analyses that assess the dose–
response relationship between alcohol and the risk of disease mortality. The quality of modelling
depends upon the quality of the risk functions and therefore on the identification of the highest

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 11
quality meta-analyses. Such identification is a complex and lengthy process that could have gone
over the 21 months allocated to update the 2011 LRDGs. However, the project’s mandate stipulated
that the update should be informed by the 2016 alcohol guidelines from the U.K. (U.K. Chief Medical
Officers, 2016) and the 2020 Australian guidelines to reduce health risks (National Health and
Medical Research Council, 2020). Therefore, a quality assessment of these alcohol guidelines was
performed. (For more information, see
Updating Canada's Low-Risk Alcohol Drinking Guidelines:
Evaluation of Selected Guidelines.) With regards to its methodology for identifying and selecting
evidence on the risks and benefits associated with alcohol consumption, the Australian guidelines
received top ratings.
Hence, to update Canada’s LRDGs, the global evidence review did not start from scratch, but rather
built upon the rigorous and systematic work previously done by the Australian Alcohol Working
Committee (AAWC), which covered the January 2017 to February 2021 period. (The overall process
is explained in section 2.1.). Besides ensuring the quality of the modelling, the global evidence
review on the risks and benefits associated with alcohol consumption identified areas where high
quality systematic reviews were missing; for these areas, the experts agreed to commission
additional reviews to formulate the updated guidelines for Canada.
1.3 The Evidence Base for Updating the Guidelines
A range of inputs was considered in updating the 2011 LRDGs:
• Global evidence review on the effects of alcohol on health
• Mathematical modelling of the lifetime risk of death and disability for various levels of average
alcohol consumption
• Rapid review on alcohol and mental health
• Rapid review on alcohol and violence
• Comprehensive multi-part review of recent literature on women’s health and alcohol
This project’s mandate also required recommendations for knowledge mobilization of the updated
alcohol guidelines. To this end, a series of activities were undertaken to better understand people’s
views, preferences and expectations on alcohol guidelines. Discussions on formulation and
presentation of the finalized guidelines were further informed by the following activities:
• Summary Evidence on Understanding and Response to Alcohol Consumption Guidelines;
• Public consultation to hear what alcohol, health and well-being issues matter most and what is
most useful to people in Canada;
• Interviews with representatives from different health-related organizations that have an interest
in alcohol-related issues; and
• Focused consultations with Indigenous People.
The overall process by which the recommendations were developed is illustrated in Figure 1.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 12
Figure 1: Process for updating Canada’s LRDGs
Note. For a PDF of this image, visit https://ccsa.ca/sites/default/files/2022-08/CCSA-LRDG-Lower-Risk-
Drinking-Guidelines-Process-and-Documentation-2022-en.pdf.
Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 13
Part 2: Evidence Used to Construct the
Recommendations
The studies and evidence reviews informing the update to the 2011 LRDGs are available on the
CCSA webpage dedicated to this project. Those interested in understanding in detail the types of
evidence and the way they were used to update the guidelines are encouraged to visit the webpage
to access the full reports. The following sections provide summaries of each report, to give readers
an overview of the material reviewed by the experts to reach their conclusions.
2.1 Global Evidence Review on the Effects of Alcohol on
Health
Several studies have quantified the risk relationships between alcohol use and the occurrence of
and mortality from all disease or injury categories causally related to alcohol consumption. However,
the quality of these studies vary greatly. To provide an answer to this project’s three research
questions and estimate the impact of alcohol consumption on individuals, a systematic search and
review was performed of meta-analyses that reported alcohol dose–response curves between
different average levels of alcohol use, disease and injuries. The aim was to identify the highest
quality systematic reviews and meta-analyses using a standard set of quality criteria. (For the full
report, see Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Evidence Review Technical
Report.)
2.1.1. Methods
A systematic electronic search was performed using PubMed, PsycNET, Embase, Cochrane Library,
Database of Abstracts of Reviews of Effects, Health Technology Assessment Database, International
Health Technology Assessment Database, Joanna Briggs Institute, Database of Systematic Reviews
of Effects, and Epistemonikos. The search was limited to articles published from Jan. 6, 2017, to
Feb. 17, 2021. It provided an update to the AAWC systematic review for 2007 to 2017. All articles
included in the Australian’s systematic review were also included in this review (National Health and
Medical Research Council, 2020).
An information specialist screened the search results and removed duplicates and any articles that
were clearly outside of the scope of the project based on titles and abstracts. Two independent
investigators assessed articles for title and abstract, and subsequently for full-text eligibility against:
• The study design and the Population, Exposure, Comparator and Outcome (PECO) criteria;
• Methodological quality criteria selected from A MeaSurement Tool to Assess systematic Reviews
(AMSTAR 2; Shea et al., 2017) and Risk of Bias in Systematic Reviews (ROBIS; Whiting et al.,
2013) tools;
• Methods of analyses criteria; and
• Mathematical modelling criteria.
If a particular disease or injury category was considered by more than one systematic review or
meta-analysis, priority was given to the article that met the most methodological quality criteria. In
the event that the same number of criteria were met, the most recent article was given priority.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 14
Finally, the quality of each eligible systematic review and meta-analysis was assessed by two
independent investigators using two international standard tools: A MeaSurement Tool to Assess
systematic Reviews (AMSTAR 2; Shea et al., 2017), and the Grading of Recommendations,
Assessment, Development and Evaluations system (GRADE; Schünemann et al., 2013). Studies were
also evaluated for the inclusion of sex- and gender-based analysis (Brabete et al., 2020).
Figure 2. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram
Records identified from:
• Databases (n = 5884)
• Grey literature (n = 31)
• Australian search (n=38)
Records removed by information
specialist:
• Duplicate records removed (n = 325)
• Records outside of the scope of the
project removed (n = 4848)
Records screened
(n = 780)
Records excluded
(n = 541)
Reports sought for full-text retrieval
(n = 239)
Reports not retrieved
(n = 0)
Reports assessed for inclusion eligibility
(n = 239)
Reports excluded:
• Did not met the PEO/study type
criteria (n = 146)
• Methods of analysis insufficient
(n = 11)
• Newer review identified and/or met
more criteria (n = 20)
• No ICD-10 code available (n = 4)
• No dose-response (n = 6)
• No causal relationship with alcohol
consumption (n = 26)
• Reverse causality with alcohol
consumption (n = 1)
• Not a fatal disease (n = 4)
• Alcohol consumption while
pregnant (n = 5)
Reports included in the mathematical
modelling (n = 16)
Identification of studies via databases and registers
Identification
Screening
Included

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 15
2.1.2 Results
In addition to the 38 systematic reviews already identified by the AAWC, a total of 5,915 systematic
reviews were initially retrieved from the updated search. The PRISMA (Preferred Reporting Items
for Systematic Reviews and Meta-Analyses) flow diagram presented in Figure 2 illustrates that after
removing duplicates and any articles that were outside of the scope of the project, a subset of 780
systematic reviews were screened for title and abstract and a total of 239 systematic reviews
(37 identified by the AAWC and 202 identified by this update) were subsequently screened for
full-text eligibility.
The 31 reports identified by the search of the grey literature were excluded as PECO and study
design criteria were not met. Most of the grey literature items were found to be informative
brochures, reports, fact sheets and books.
In the end, a total of 16 systematic reviews fulfilled all the inclusion criteria for this project for all
three research questions and were selected for inclusion in the mathematical modelling.
Research Question 1: Short-Term Risks and Benefits
Twenty-nine systematic reviews on the short-term risks and benefits of alcohol were evaluated. Two
systematic reviews were selected for inclusion in the mathematical modelling. One selected
review focused on road injury (Taylor & Rehm, 2012) and the other on intentional and unintentional
injuries (Taylor et al., 2010).
Research Question 2: Long-Term Risks and Benefits
A total of 154 systematic reviews across eight categories of diseases associated with the long-term
health risks and benefits of alcohol were evaluated. Fourteen reviews were selected for inclusion
in the mathematical modelling. The selected reviews assessed the relationship between alcohol
use and liver cirrhosis (Roerecke et al., 2019), ischæmic heart disease (Zhao et al., 2017),
hypertensive heart disease (Liu et al., 2020), breast cancer (Sun et al., 2020), liver cancer (World
Cancer Research Fund International, 2018), pancreatitis (Samokhvalov et al., 2015), lower
respiratory infections (Samokhvalov et al., 2010a;), epilepsy (Samokhvalov et al., 2010b) ischemic
stroke (Larsson et al., 2016), intracerebral hemorrhage (Larsson et al., 2016),subarachnoid
hemorrhage (Larsson et al., 2016), atrial fibrillation (Larsson et al., 2014), colon and rectum cancers
(Vieira et al., 2017), diabetes mellitus (Knott et al., 2015), larynx cancer (Bagnardi et al., 2015),
mouth and oropharynx cancers (Bagnardi et al., 2015), esophagus cancer (Bagnardi et al., 2015)
and tuberculosis (Imtiaz et al., 2017).
Research Question 3: Pregnancy and Child Development Risks and
Benefits
Twenty-five systematic reviews focusing on the risks and benefits associated with alcohol
consumption during pregnancy or breastfeeding for fetal, infant and child development were
evaluated. None were selected for inclusion in the modelling because none met the mathematical
modelling criteria. The studies focused on alcohol-attributable mortality and morbidity to others
rather than the person who consumes alcohol.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 16
2.1.3 Implications
The global evidence review identified the most recent and highest quality systematic reviews and
meta-analyses available to examine the relationship between alcohol consumption and the various
outcomes covered by this project’s research questions. The methodology used to select these
systematic reviews is based on the Australian guidelines, which received a top score according to a
previous evaluation, further strengthening our certainty that our results are based on the highest
quality evidence. (For more information, see Update of Canada's Low-Risk Alcohol Drinking
Guidelines: Evaluation of Selected Guidelines.)
Through this work, we identified areas where high quality systematic reviews are currently missing
(e.g., mental health, violence) and for which the experts agreed to commission additional reviews to
complete the LRDG update (see section 2.4). A decision was also taken to commission a report on
women’s health and alcohol that would address, among other things, the issues of pregnancy.
2.2 Mathematical Modelling of the Lifetime Risk of Death
for Various Levels of Average Alcohol Consumption
To establish alcohol guidelines, modelling the lifetime risk of death for various levels of average
alcohol consumption has been recommended (Broholm et al., 2016; Rehm et al., 2014) and applied
(e.g., in Australia, the U.K., France and Canada). Modelling allows for the estimation of the “excess
risk” of mortality and disability associated with various levels of average consumption and the
specification of the level of risk from negligible to high associated with each level of consumption.
The aim of modelling is not to set a “threshold” of consumption below which there is no risk, but to
provide “benchmarks” based on which recommendations can be formulated.
For this project, the lifetime risk approach was adopted to estimate the lifetime risk of death,
premature death (< 75 years of age), years of life lost (YLLs) and disability-adjusted life years (DALYs)
lost. A full report presenting all analyses is available in Lifetime Risk of Alcohol-Attributable Death
and Disability. Every estimation and result presented in the report was subsequently the object of a
shadow analysis that confirmed the accuracy of the primary analyses (Appendix 1).
Discussions among experts led to a decision to use risk thresholds associated with YLLs. Compared
to using lifetime risk of death or premature death, YLLs allows researchers to consider the deaths of
older individuals and, more importantly, factors the unequal health loss caused by death among
people relatively younger in age. While DALYs can be an optimal outcome for the measurement of
health loss attributable to alcohol, there is limited data on the DALYs alcohol cause and this project’s
analyses resulted in identical risk thresholds whether they were based on YLLs or DALYs.
3
Since
DALYs is conceptually more difficult to understand than YLLs, the experts fixed their choice on YLLs
estimations. Results are presented and discussed below, after a review of methodological principles.
3
For example, there is evidence that DALYs can be influenced by mental disorders such as depression but because the evidence search
did not identify high-quality systematic reviews assessing the relationship between alcohol use and mental health, it is likely that the
current project underestimates alcohol-related DALYs.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 17
2.2.1 Methodological Principles
Calculating Alcohol-Attributable Deaths
In epidemiology, the concept of an attributable fraction makes it possible to express the proportion
of risk for a particular health event (in this case death), due to exposure to a particular cause (in this
case alcohol consumption). An attributable fraction is classically calculated from the number of
deaths that could be avoided if the exposure was eliminated.
The proportion depends on the risk of death according to sex and age but also on the “trajectory” of
exposure, which is the history of alcohol consumption before the subject’s death. Establishing
alcohol-attributable deaths in the population requires access to the population’s mortality rate and
knowledge of the individuals’ lifetime exposure to alcohol in standardized terms, such as average
grams of alcohol per day. With this data, alcohol-attributable deaths can be calculated for various
levels of consumption, provided that it is considered identical among individuals and constant over
time for each of them until death. In this model, lifetime abstainers are the reference group in relation
to which the risks associated with different average levels of alcohol consumption are calculated.
By varying the average level of consumption in such a scenario, it becomes possible to summarize
the relationship between the risk due to alcohol and different levels of consumption. In return, this
informs the benchmarks for different levels of risk.
Diseases and Injuries Included in the Modelling
A total of 34 cause categories for alcohol-related diseases, conditions and injuries and more than
200 three-digit International Classification of Disease, version 10 (ICD-10-CA) codes were included in
the modelling of alcohol-attributable deaths. To be included, there were three criteria:
1. The disease or injury had to be causally related to alcohol use;
2. A dose–response risk function needed to be available for the risk relationship between alcohol
consumption (measured in grams per day) and the disease or injury of interest that also passed
the GRADE criteria; and
3. Either death or disability needed to be measured specifically for the disease or injury causally
related to alcohol use.
What Evidence Has Changed Since the Release of the 2011 LRDGs?
•
Animal, mechanistic and epidemiological evidence published since the publication of the
Canadian LRDGs in 2011 has led to changes in the diseases that are known to be causally
related to alcohol use.
• Alcohol has been found to causally increase the risk of lower respiratory infections
(Samokhvalov et al., 2010a).
• Systematic reviews on the risk relationship between alcohol use and the diagnosis of and
death from cancer have observed no lower risk threshold (Bagnardi et al., 2015; Sun et al.,
2020; Vieira et al., 2017; World Cancer Research Fund, 2018).
• The risk relationship between alcohol use and hypertensive heart disease has been observed
to have no lower risk threshold (Liu et al., 2020).

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 18
• Risks for hemorrhagic stroke have been investigated further, with the risk functions for
intracerebral hemorrhage showing protective at lower levels of alcohol use but for subarachnoid
hemorrhage, detrimental effects at lower levels of alcohol use (Larsson et al., 2016)
• Alcohol’s protective impact on ischemic heart disease at lower levels of alcohol use is more
uncertain than previously estimated. The risk is modified by binge drinking (Roerecke & Rehm,
2010; Sundell et al., 2008) and genetics (Chikritzhs et al., 2015; Larsson et al., 2020) .
Data Sources
Several data sources were used to make the necessary calculations:
• Data on death and disability for 2017 to 2019 were obtained from Statistics Canada and the
Institute for Health Metrics and Evaluation’s Global Burden of Disease study (Institute for Health
Metrics and Evaluation, 2018).
• Alcohol exposure data were obtained from the Canadian Alcohol and Drug Use Monitoring Survey
and the Canadian Tobacco, Alcohol and Drugs Survey. Survey data were corrected for total
consumption in Canada (adult per capita consumption) using data from Statistics Canada and
the World Health Organization’s Global Information System on Alcohol and Health (World Health
Organization, 2021).
• Relative risk estimates for diseases and injuries were obtained following the evidence review
(see previous section) that enabled us to identify the highest quality meta-analyses.
The calculations for this project are based on the health harms cause by ethanol in alcoholic
beverages. They do not distinguish between harms caused by beer, wine, spirits and other
alcoholic beverages. Harms caused by beer, wine, spirits and other alcoholic beverages are based
mainly on ethanol content, regardless of the form in which ethanol is consumed. Alcohol
poisonings, which are caused predominately by the consumption of spirits, are the one exception
where the type of alcoholic beverage makes a difference (Rehm, Gmel Sr, et al., 2017)
2.2.2 Results and Implications
The relative risk estimates by cause of disease and average alcohol consumption are outlined in
Table 1 for females and Table 2 for males. For most diseases and injuries alcohol had a net negative
impact on health at all levels of alcohol use, with net impacts being defined by confidence intervals
not crossing a zero effect. However, for diabetes mellitus (females only), ischemic heart disease,
ischemic stroke, intracerebral hemorrhage and pancreatitis (females only), alcohol was neither
associated with a negative nor protective net effect at lower alcohol use amounts. (Confidence
intervals associated with increased risk of diseases and injuries are presented in Appendix 2.)
Furthermore, the leading causes of death among those causes related to alcohol were ischemic
heart disease, followed by colorectal cancer and unintentional injuries (excluding road injuries) for
males, and breast cancer and unintentional injuries (excluding road injuries) for females.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 19
Table 1. Increased risk of diseases and injuries for females based on average daily alcohol use
Disease or injury
Deaths
per
100,000
people per
year
Premature
deaths
per
100,000
people
per year
Average alcohol intake (g/day)
5
10
15
20
25
30
35
40
45
50
Ischemic heart disease 72.1 16.7 -5.0% -5.0% -5.0% -5.0% 4.0% 4.0% 4.0% 4.0% 7.0% 7.0%
Breast cancer 28.3 17.3
4.7%
9.5%
14.7%
20.0%
25.6%
31.5%
37.6%
44.0%
50.7%
57.7%
Other unintentional injuries 22.6 4.3
4.0%
8.1%
12.4%
16.8%
21.4%
26.3%
31.3%
36.5%
41.9%
47.5%
Lower respiratory infections 22.3 3.7 2.4%
4.9%
7.4%
10.0%
12.7%
15.4%
18.2%
21.0%
23.9%
26.9%
Colorectal cancer 21.0 9.2
3.4%
7.0%
10.7%
14.5%
18.4%
22.5%
26.7%
31.1%
35.6%
40.3%
Diabetes Mellitus 12.6 4.7 -21.6% -26.9% -30.0% -31.9% -33.2% -34.0% -34.4% -34.6% -34.6% -34.4%
Hypertension 11.3 1.9 3.0%
6.0%
8.9%
11.8%
14.9%
18.0%
21.4%
24.8%
28.4%
32.0%
Atrial fibrillation and flutter 10.4 0.6
3.3%
6.6%
10.1%
13.7%
17.4%
21.2%
25.2%
29.2%
33.5%
37.8%
Intracerebral hemorrhage 8.6 2.4 -8.0% -8.0% -1.0% -1.0% 25.0% 25.0% 25.0% 25.0% 25.0%
67.0%
Liver cirrhosis 6.9 5.5
109.5%
182.1%
254.9%
330.8%
411.2%
496.7%
588.0%
685.5%
789.6%
900.9%
Ischemic stroke 6.5 1.1 -10.0% -10.0% -8.0% -8.0%
8.0%
8.0%
8.0%
8.0%
8.0%
14.0%
Liver cancer 6.0 3.2
2.0%
4.0%
6.1%
8.2%
10.3%
12.5%
14.7%
17.0%
19.3%
21.7%
Intentional injuries 5.8 5.9
13.3%
28.3%
45.4%
64.7%
86.6%
111.4%
139.4%
171.2%
207.3%
248.1%
Road injuries 2.8 2.5
4.9%
10.1%
15.5%
21.2%
27.1%
33.4%
39.9%
46.8%
54.0%
61.6%
Esophagus cancer 2.6 1.5
6.8%
14.1%
21.9%
30.2%
39.0%
48.4%
58.5%
69.1%
80.5%
92.5%
Subarachnoid hemorrhage 2.4 1.7 21.0% 21.0% 11.0% 11.0% 39.0% 39.0% 39.0% 39.0% 39.0% 82.0%
Oral cavity and pharynx cancer 2.2 1.2
13.1%
27.6%
43.6%
61.4%
81.0%
102.6%
126.3%
152.3%
180.8%
211.7%
Pancreatitis 1.2 0.5 -12.7% -22.7% -28.3% -28.4% -23.9% -15.0% -2.0% 14.8% 34.9% 58.4%
Epilepsy 0.7 0.4
7.0%
13.8%
21.0%
28.6%
36.8%
45.5%
54.7%
64.5%
74.9%
86.0%
Larynx cancer 0.3 0.2
7.5%
15.5%
24.0%
32.9%
42.3%
52.3%
62.8%
73.8%
85.4%
97.6%
Tuberculosis 0.2 0.1
9.4%
19.7%
30.9%
43.2%
56.7%
71.4%
87.6%
105.2%
124.5%
145.6%
Dark red > 50%; light red 20% to 50%; yellow 10% to < 20%; green < 10%
Bolded percentages indicate significant estimates

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 20
Table 2. Increased risk of diseases and injuries for males based on average daily alcohol use
Disease or injury
Deaths
per
100,000
people
per year
Premature
deaths
per
100,000
people
per year
Average alcohol intake (g/day)
5
10
15
20
25
30
35
40
45
50
Ischemic heart disease 104.1 47.5 -5.0% -5.0% -5.0% -5.0% 4.0% 4.0% 4.0% 4.0% 7.0% 7.0%
Colorectal cancer 25.6 13.9
3.4%
7.0%
10.7%
14.5%
18.4%
22.5%
26.7%
31.1%
35.6%
40.3%
Other unintentional injuries 23.2 9.8
4.0%
8.1%
12.4%
16.8%
21.4%
26.3%
31.3%
36.5%
41.9%
47.5%
Lower respiratory infections 19.3 5.1
2.4%
4.9%
7.4%
10.0%
12.7%
15.4%
18.2%
21.0%
23.9%
26.9%
Intentional injuries 18.0 17.9
13.3%
28.3%
45.4%
64.7%
86.6%
111.4%
139.4%
171.2%
207.3%
248.1%
Diabetes Mellitus 16.8 9.0 0.0% 0.2% 0.4% 0.6% 1.0% 1.4% 1.9% 2.4% 3.0% 3.6%
Liver cirrhosis 12.2 10.3
15.5%
32.9%
52.8%
75.7%
102.0%
132.3%
167.1%
207.1%
253.2%
306.1%
Liver cancer 11.1 7.5
2.0%
4.0%
6.1%
8.2%
10.3%
12.5%
14.7%
17.0%
19.3%
21.7%
Esophagus cancer 9.0 6.2
6.8%
14.1%
21.9%
30.2%
39.0%
48.4%
58.5%
69.1%
80.5%
92.5%
Hypertension 8.4 3.4
7.2%
15.0%
19.0%
23.2%
27.5%
32.0%
34.0%
35.9%
38.0%
40.0%
Intracerebral hemorrhage 8.2 3.3 -8.0% -8.0% -1.0% -1.0% 25.0% 25.0% 25.0% 25.0% 25.0%
67.0%
Atrial fibrillation and flutter 6.6 1.0
3.3%
6.6%
10.1%
13.7%
17.4%
21.2%
25.2%
29.2%
33.5%
37.8%
Road injuries 6.0 5.6
7.6%
15.9%
24.7%
34.2%
44.5%
55.5%
67.4%
80.2%
93.9%
108.7%
Ischemic stroke 5.7 1.9 -8.0% -8.0% -8.0% -8.0%
8.0%
8.0%
8.0%
8.0%
8.0%
14.0%
Oral cavity and pharynx cancer 5.2 3.6
13.1%
27.6%
43.6%
61.4%
81.0%
102.6%
126.3%
152.3%
180.8%
211.7%
Larynx cancer 1.8 1.1
7.5%
15.5%
24.0%
32.9%
42.3%
52.3%
62.8%
73.8%
85.4%
97.6%
Subarachnoid hemorrhage 1.6 1.2 21.0% 21.0% 11.0% 11.0% 39.0% 39.0% 39.0% 39.0% 39.0% 82.0%
Pancreatitis 1.5 0.9
9.1%
18.9%
29.7%
41.5%
54.3%
68.3%
83.5%
100.1%
118.3%
138.0%
Epilepsy 0.7 0.6
7.0%
13.8%
21.0%
28.6%
36.8%
45.5%
54.7%
64.5%
74.9%
86.0%
Tuberculosis 0.3 0.2
9.4%
19.7%
30.9%
43.2%
56.7%
71.4%
87.6%
105.2%
124.5%
145.6%
Dark red > 50%; light red 20% to 50%; yellow 10% to < 20%; green < 10
Bolded percentages indicate significant estimates

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 21
Lifetime Risk of Alcohol-Attributable Disability-Adjusted Years of
Life Lost by Sex
Figure 3 presents lifetime risk of a YLL because of alcohol use, for both males and females, for
average levels of alcohol intake varying from 0 to 40 grams of alcohol per day. In Canada, where a
standard drink is 13.45 grams of pure alcohol, this corresponds to consuming zero to three (2.97)
standard drinks per day in an average per week.
The modelling reveals that the number of YLLs increases as alcohol use increases among both
males and females. Among males and females, a protective association was observed for those
consuming 2 to 3 g/day (less than a fifth of a standard drink per day on average) when compared to
people who engaged in lifetime abstention. In all cases, the 95% uncertainty intervals (UIs) crossed
the null hypothesis threshold, which means there is not enough evidence to confirm the protective
effect.
The risk threshold based on 17.5 YLL in 1,000 lifetimes would be:
• 4 (95% UI: <1, 16) g/day for females
• 4 (95% UI: <1, 10) g/day for males
The risk threshold based on 17.5 YLL in 100 lifetimes would be:
• 11 (95% UI: 1, 22) g/day for females
• 11 (95% UI: 1, 19) g/day for males
Reported on a weekly basis, this means that for both females and males, the risk threshold based on
17.5 YLL in 1,000 lifetimes would be 28 g/week or two (exactly 2.08) standard drinks per week,
while based on 17.5 YLL in 100 lifetimes, it would be 77 g/week or six (exactly 5.7) standard drinks
per week.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 22
Figure 3. Lifetime risk of a year of life lost (YLL) attributable to alcohol use at varying levels of average alcohol intake
Based on the systematic review of the published literature on the risk relationships between alcohol
use and disease and injury occurrence, this study estimated that for people who live in Canada, the
lifetime risk of death and disability attributable to alcohol use increases as the amount of
alcohol use increases. The selected model did neither demonstrate a significant negative nor
protective net effect at lower levels of alcohol use and, therefore, alcohol should not be promoted or
used as a product to improve health.
As the lifetime risk of mortality and morbidity is similar for males and females, one guideline for
alcohol consumption can be used for Canada. According to established definitions of acceptable
risks and based on the risk thresholds of 17.5 YLL attributable to alcohol per 1,000 and 100
lifetimes, risk thresholds for alcohol use should be set at either two or six standard drinks per
week (four or 11 g/day) respectively, for both females and males in Canada.
Canada’s 2011 LRDGs pose higher risks in light of current evidence
To reduce the risk of long-term harm, Canada’s 2011 LRDGs recommended consuming no more
than 15 drinks a week among males (~29 g/day) and 10 drinks a week for females (~19 g/day).
Based on today’s data sources and the life course approach to estimate the risk of an alcohol-
attributable death, the 2011 recommendations would be associated with the following risk thresholds:
• Consumption by males of 29 g/day would result in
757 YLL per 1,000 lifetimes
• Consumption by females of 19 g/day would result in
336 YLL per 1,000 lifetimes
Put differently, the 2011 LRDGs would be associated with a risk for males that is between 76 and
757 higher than established definitions of acceptable risk, and with a risk for females that would
be between 34 and 336 higher than those definitions.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 23
2.3 Alcohol Use per Occasion
The risks from alcohol use for most health outcomes (e.g., death, certain cancers, heart disease,
injuries) are usually based on how much alcohol is consumed on average or the total amount
consumed over the past week or month (see tables 1 and 2). That is why the mathematical
modelling led to results expressed in an average number of standard drinks per week, that is,
between two and six standard drinks per week, depending on which level of risk is considered.
However, most people do not drink their average amount every day: on days they use alcohol there is
considerable variability in how much they use on different drinking “occasions.” For this reason,
many people who drink relatively low weekly or monthly amounts of alcohol may in fact drink large
quantities on a single occasion, which may put them at risk for harm (Naimi et al., 2003). In the
context of personal well-being, the experts discussed the latest evidence on alcohol use per drinking
occasion to be able to advise people living in Canada on this particular issue.
With alcohol use during any drinking occasion, each drink increases one’s blood alcohol concentration
(BAC). An increased BAC is what leads to alcohol impairment (a reduced ability to think clearly or
perform certain activities) and intoxication (which is the appearance or sensation of being drunk). The
risk begins to increase with any use of alcohol, and with more than two standard drinks, most
individuals will have a demonstrably increased risk of “acute” problems. For example, compared to no
alcohol use, studies of injuries in emergency departments show increasing risk for each drink
consumed for both men and women.(Cherpitel et al., 2015; Vinson et al., 2003) Similarly, studies of
motor vehicle crash fatalities demonstrate increasing risk above a BAC of 0.02%,(Blomberg et al.,
2009; Compton & Berning, 2015; Voas et al., 2012), which corresponds to about one drink. After
about two standard drinks consumed within an hour, one’s BACs may be approximately 0.05% (the
level will differ on the basis of body mass and other factors). Above this level, risk gets progressively
and substantially higher the more one drinks on any occasion and the higher one’s BAC. It is important
to recognize that people typically exhibit behaviour changes or become impaired starting at BAC levels
below those at which they feel “drunk” or appear intoxicated (Midanik, 1999).
Binge drinking, usually defined as consuming five standard drinks or more for men, or four standard
drinks or more for women, in one setting (National Institute of Alcohol Abuse & Alcoholism, 2004;
Wechsler & Austin, 1998) is a common yet dangerous pattern of consumption that results in legal
impairment (i.e., a BAC > 0.08%) for most persons, and is significantly associated with a range of
alcohol-related health and social problems (Centers for Disease Control and Prevention, 2022; Fillmore
& Jude, 2011).
4
Specifically, binge drinking and resulting BAC levels are well-established risk factors
for death from any cause, including unintentional injuries (car crashes, drownings, falls), physical and
sexual violence, cardiovascular disease (hypertension, myocardial infarction, stroke), inflammation of
the gastrointestinal system (gastritis, acute pancreatitis), and the development of an alcohol use
disorder (Alpert et al., 2022; Brewer & Swahn, 2005; Dawson et al., 2005; Devries et al., 2014; Dietary
Guidelines Advisory Committee, 2020; Mukamal et al., 2005; Roerecke & Rehm, 2014).
Many of the complications arising from acute impairment and binge drinking involve second-hand
effects that affect someone other than the person who drinks (e.g., domestic violence, child abuse
and neglect). Because binge drinking is common and involves large volumes of use, binge drinking
occasions account for a substantial proportion of all alcohol consumed in the population. As such,
binge drinking is also an important contributor to long-term health problems like liver disease and
4
Some scientists have questioned this criteria and suggested that a lowered standard defining impairment should be used for women
(Canadian Centre on Substance use and Addiction, 2014; Thomas et al., 2014). Patterns of alcohol use among women of childbearing
years in Canada: Implications for FASD prevention Public Health 2014, Toronto, On.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 24
certain cancers (Llerena et al., 2015). Fortunately, effective alcohol control policies can reduce rates
of binge drinking and related problems (Naimi et al., 2014; Wagenaar et al., 2009; Wagenaar et al.,
2010). Although most persons who engage in binge drinking do not meet criteria for an alcohol use
disorder, virtually all persons with an alcohol use disorder engage in binge drinking.
In sum, the evidence is clear and consistent: in terms of health, fewer standard drinks per drinking
occasion means less risk of harms to the person consuming the alcohol and reduced risk of second-
hand effects to those other than that person. Although some risk begins at one drink and increases
more substantially, with more than two standard drinks, risks are higher and increase very rapidly at
or above binge drinking levels (five or more standard drinks for men, four or more standard drinks for
women). At all levels of per occasion use, consuming fewer standard drinks is better for health; the
more standard drinks one consumes per occasion, the larger the benefits from reductions in use.
2.4 Rapid Reviews
At the beginning of this project, a public consultation was held to hear what alcohol, health and well-
being issues mattered most and were most useful to people living in Canada. (We will return to this
in section 2.6.) A key finding from the consultation was that from a list of eight topics, the one
respondents asked to be prioritized in the updated guidelines was the impact of drinking alcohol on
mental health. It was followed by the impact of drinking alcohol on physical health and how alcohol
can impact people’s lives via, for example, violence and sexual assaults.
Unfortunately, the updated evidence review on the effects of alcohol on health did not identify high
quality-evidence systematic reviews on alcohol use and mental health nor on alcohol use and social
harms. Not a single review met all the selection criteria. (See section 2.1 and Update of Canada’s
Low-Risk Alcohol Drinking Guidelines: Evidence Review Technical Report. This means that the
modelling presented in the previous section ignores the impact that alcohol may have on mental
health and violence and therefore, on people’s overall risk of death and disability. To overcome this
blind spot, the experts agreed to commission two rapid reviews, one on the effects of alcohol on
violence and another one on the effects of alcohol on mental health.
2.4.1 Association Between Alcohol Use, Aggression and Violence
In the absence of recent high quality systematic reviews or meta-analyses on alcohol and violence
and to inform experts opinion, an overview of recent reviews of the literature on alcohol and
aggression and violence (A/V) was commissioned.
Alcohol is associated with many health and social harms, including various forms of aggression and
violence. Three common forms of A/V that have shown high rates of alcohol involvement and that
experts agreed to consider to update Canada’s 2011 LRDGs are intimate partner A/V (IPV), male-to-
female sexual A/V (SV), and non-intimate and non-sexual A/V between adults or general A/V (GV).
The role of alcohol in both A/V perpetration (being aggressive or violent toward another adult) and
victimization (having an act of aggression or violence done toward them) was considered.
5
Relevant
details about findings related to sex/gender differences are reported where available.
6
5
In the context of this overview, perpetrator refers to the person who was aggressive/violent toward another person or persons.
Perpetration refers to the act of carrying out A/V. Victim refers to the person or persons to whom the aggressive/violent act was done
(commonly referred to in the literature as the victim, target or survivor); that is, the person who was victimized by the perpetrator.
Victimization refers to the process of being victimized. These terms are not meant to label those who experience violence. Use of terms
“victim” or “victimization” is by no means intended to assign blame, imply weakness or guilt, or otherwise stigmatize those who experience
A/V, nor is it meant to imply any particular response or impact of the A/V on the person.
6
We use the term “sex/gender” in this overview because, while some studies restricted their analyses to sex (biological attributes), both
alcohol consumption and A/V are inextricably linked to gender (socially constructed roles, norms, values and behaviours).

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 25
The full report, Update of Canada's Low-Risk Alcohol Drinking Guidelines: Overview of Reviews of the
Association Between Alcohol Use and Aggression and Violence, including references, is available on
CCSA’s LRDG 2022 webpage. A summary of the report is presented in this report.
Method
A comprehensive search was performed of the literature published from the year 2000 to January
2022, including systematic reviews (i.e., meta-analyses and narrative literature reviews), using the
following databases: Medical Literature Analysis and Retrieval System Online (MEDLINE) and
Excerpta Medica Database (Embase) using the OVID platform, PubMed, PsychINFO, PsychNET, Web
of Science, Criminal Justice Abstracts, Cochrane CENTRA and other reviews from our collection.
• The search resulted in 3,826 records.
• After removal of duplicates, 2,744 titles and abstracts were retrieved.
• After screening by two independent screeners, 54 reviews were included (30 IPV, 10 SV and 14
GV). Results are reported separately for IPV, SV and GV, and separately for perpetration and
victimization.
Key Findings
Alcohol and Intimate Partner Violence (IPV) Perpetration
Event-level alcohol consumption (i.e., having consumed alcohol at the time or prior to the A/V
incident) was associated with perpetration of IPV, but the strength of the relationship varied by
sample and sex/gender of perpetrator (larger for male than for female perpetrators). In terms of
usual drinking pattern (e.g., usual number of standard drinks consumed per occasion, frequency of
consumption over a specific time period, a regular pattern of drinking to intoxication), heavy episodic
drinking (or binge drinking) and drinking to intoxication were positively associated with IPV
perpetration, with weaker associations found for drinking frequency. As with event-level drinking, the
relationship between usual drinking pattern and IPV perpetration was stronger for men than for
women. Drinking problems and alcohol use disorders were positively associated with IPV
perpetration, with stronger relationships for male than for female perpetrators (although some
inconsistent findings were also reported). Some evidence suggested that alcohol use was also
associated with more severe IPV perpetration.
Alcohol and IPV Victimization
Event-level drinking was associated with greater risk of being the victim of IPV. Findings were
inconsistent relating to drinking pattern of the victim, but generally suggested that IPV victimization
was associated with a pattern of heavy episodic drinking and intoxication, as well as drinking
problems and alcohol use disorders. However, estimates of associations were usually smaller than
were found for drinking by perpetrators, and some estimates were non-significant.
Alcohol and Male-to-Female Sexual Violence (SV) Perpetration
Small-to-medium effect sizes were found for the relationship between event-level alcohol
consumption and male-to-female SV perpetration, although some experimental paradigms did not
produce a significant effect of alcohol on SV. As well, moderating factors such as personality and
attitudes were noted in the relationship. Associations were found between perpetration of SV and
both drinking patterns and drinking problems, particularly for heavy episodic drinking. However, not

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 26
all studies found significant associations, especially when key variables such as past perpetration
were controlled.
Alcohol and Male-to-Female SV Victimization
Consuming higher amounts of alcohol prior to SV was associated with greater severity of SV
experienced by victims in some, but not all studies. This finding may relate to heavier drinking by the
perpetrator because drinking by perpetrators and victims is highly correlated. Although there is
relatively little research, some evidence suggested that women who engaged in a pattern of heavy
episodic drinking, drinking to intoxication or problem drinking were more likely to be victims of SV.
Alcohol and General Violence (GV) Perpetration
Experimental, laboratory-based and other research indicates that alcohol increases aggressive
behaviour (medium effect sizes), with variability related to how aggression was measured in the
laboratory and sex/gender of aggressors. The research also identified important moderators of the
association. Research suggests positive associations between GV perpetration by individuals and
heavier drinking patterns as well as drinking problems. However, the evidence is less clear for usual
quantity consumed per occasion (i.e., average number of drinks usually consumed) by individuals
and frequency of drinking than for alcohol in the event (i.e., consumption during or prior to an A/V
event), and the reviews in this area have methodological weaknesses.
Alcohol and GV Victimization
A large proportion of homicide victims tested positive for alcohol (larger for women than men), and
many were defined as intoxicated (BAC > .08 or .10), although these studies found large variability in
estimates. Homicide rate was found to be positively correlated with per capita consumption in some
countries but not others. Emergency department studies indicated that patients with violence-related
injuries were significantly more likely to have consumed alcohol than were non-violence-related
injured patients, with some evidence suggesting the relationship was stronger for men than for
women. There were insufficient data on drinking patterns of GV victims to draw conclusions about
the relationship between alcohol consumption and being the victim of GV.
Discussion
Although the exact mechanisms by which alcohol is associated with A/V are unknown, there is
overwhelming evidence that alcohol consumption, especially intoxication, is associated with
perpetration of A/V, and some evidence indicates that alcohol may increase the severity of A/V.
However, there are insufficient data to define the exact dose–response relationship. Thus, although
existing research does not allow the calculation of a risk curve for alcohol and A/V, it is reasonable
to infer that individuals can reduce their risk of perpetrating A/V by limiting their alcohol
consumption. Based on consistent evidence, it is highly likely that avoiding drinking to
intoxication will reduce individuals’ risk of perpetrating alcohol-related violence. Therefore,
efforts to reduce or eliminate alcohol-related A/V need to focus on reducing alcohol use, especially
among those who may be likely to perpetrate A/V or get involved in violent incidents. Because A/V
decreases with age and is perpetrated more by men than women, prevention efforts should focus on
young adults, particularly young men. Overall, people should be encouraged to avoid drinking high
levels of alcohol or avoid drinking altogether to reduce their risk of perpetrating violence. Persons
who have a history of alcohol-related violence should avoid any consumption of alcohol.
The literature on the association between alcohol and A/V victimization is less clear. The findings
suggest there is likely an association, but there are some mixed and null findings, and noteworthy
limitations of this literature. Alcohol’s role in victimization likely reflects many different mechanisms

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 27
that may work in combination, such as alcohol intoxication reducing the ability to avoid or escape
danger, use of alcohol by victims due to trauma, increased exposure to risk in drinking settings,
targeting by perpetrators of people who are intoxicated, and use of substances to control victims.
Attributing A/V victimization to alcohol contributes to beliefs that victims of A/V who had used
alcohol are responsible or blameworthy for being victimized. Moreover, evidence suggests that
interventions that place the burden to avoid risk of victimization on women and girls are ineffective.
While alcohol might be a contributing factor in A/V victimization, we state unequivocally that drinking
alcohol does not make a person responsible for A/V done toward them. Thus, we conclude that lower
risk drinking guidelines should focus on reducing alcohol use by potential perpetrators.
2.4.2 Association Between Alcohol Use and Mental Health
In 2016, when Australia’s National Health and Medical Research Council was asked to revisit their
2009 alcohol guidelines, their systematic review on the health effects of alcohol consumption
revealed there was actually very little synthesized evidence on how different levels of alcohol
consumption influence mental health (National Health and Medical Research Council, 2020).
Because this question was of interest for drafting updated alcohol guideline recommendations, the
Adelaide Health Technology Assessment, University of Adelaide, was contracted to conduct a
systematic literature review on the latest and best scientific evidence on the mental health risks and
benefits of alcohol consumption (Newton et al., 2018). The Newton et al. systematic review, plus six
new systematic reviews on the association between alcohol consumption and mental health and
substance use disorders were evaluated for the current project (See Update of Canada’s Low-Risk
Alcohol Drinking Guidelines: Evidence Review Technical Report). None of the reviews met the criteria
for inclusion.
Given the previously mentioned importance that people living in Canada expressed for the
relationship between alcohol and mental health, the experts decided to commission Cochrane
Canada, McMaster University, to conduct a rapid update of a systematic review of the effect of
alcohol consumption on the development of depression, anxiety and suicidal ideation. The full report,
Effect of Alcohol Consumption on the Development of Depression, Anxiety and Suicidal Ideation:
Update of a Systematic Review, is available on CCSA’s LRDG 2022 webpage.
Limitations of the Rapid Update and Experts’ Decision
With this rapid update, the intention was to be able to pool together results across studies using
statistical analyses. Unfortunately, as with the 2018 review prepared by Newton et al., thresholds
and definitions for alcohol quantity or frequency varied across studies and so a statistical analysis
could not be performed. In addition, studies often failed to report odds ratios with standard errors or
confidence intervals so results could not be easily pooled. The review was also found that many
studies did not report results that could be easily interpreted and even the most recently published
studies provided little data that could be used to make healthcare decisions. Experts highlighted that
just as was the case for many studies on the relationship between alcohol and physical health, many
studies on alcohol and mental health misclassified abstainers. Specifically, to assess the impact of
alcohol on mental health, the reference group against which those who use alcohol were compared
were people who do not consume alcohol, including people who quit using alcohol because of health
problems, such as mental health issues. In addition, the experts noted that the results of the review,
which generally showed a null association between alcohol and mental health, contradicted the most
recent WHO findings. The WHO review from 2019 found a close link between patterns of alcohol use
and depression, between harmful alcohol use and anxiety disorders, and between harmful use of
alcohol or dependence and self-harm or suicidal behaviour (World Health Organization, n.d.).

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 28
For all these reasons, the experts agreed that further work would be required for mental health
outcomes to be considered when making alcohol guidelines recommendations. The experts were
unanimous in opting to make the rapid review publicly available but agreed that it would not inform
their final discussions on formulation and presentation of updated guidelines.
2.5 Women’s Health and Alcohol
The mathematical modelling revealed identical risk thresholds for females and males at low levels of
alcohol consumption. This was not unexpected. When the U.K. and Australia updated their alcohol
guidelines, both made identical recommendations for men and women. Since 2017, France also
recommends the same alcohol limits for both sexes and when Denmark released its new alcohol
guidelines in spring 2022, they recommended the same amount for adult women and men alike,
and no alcohol consumption for those under 18 years old.
The results obtained by our modelling align with the global trend to not differentiate between
females and males when formulating alcohol guidelines. This conclusion is because at low levels of
consumption the physiological differences between women and men have only a small impact on
lifetime risk of death. However, above low risk, lifetime risk increases more steeply for women than
for men.
The experts are mindful of the complexity of this reality and the necessity to describe it well. Proper
understanding of sex-related and gender-related factors on women’s health and reproductive issues
is key to reach and inform audiences in a meaningful way. Updated alcohol guidelines need to be
shared with the appropriate nuances. To this end, a comprehensive multi-part review of the recent
literature on sex, gender, alcohol and health was commissioned.
The full report prepared by Galvanizing Equity, including references, is available here: Sex, Gender
and Alcohol: What Matters for Women in Low-Risk Drinking Guidelines? and a short version is
presented below. This section concludes with evidence-based key messages that health
professionals and policy makers may want to consider in their programs, practices and
communications about alcohol.
2.5.1 What Are Some Sex-Related Factors?
The four main categories of sex-related biological factors that are important to understanding how
alcohol affects male and female bodies are hormones and enzymes, physiology and anatomy,
genetics, and neurobiology. Within these, various sex-related differences, factors or processes exist.
The absorption, distribution and metabolism of alcohol is affected by sex-related factors. For
example, females absorb ethanol faster than males, and reach a higher BAC due to faster absorption
and slower elimination. Significantly, females generally experience more risk of damage or disease,
such as liver disease, at lower levels of alcohol consumption than do males. In general, males are
more likely to develop alcohol use disorders, but females are more likely to develop organ and other
bodily damage from drinking alcohol.
2.5.2 What Are Some Gender-Related Factors?
There are different impacts on women or men or gender and sexual minorities as a result of alcohol.
The four main aspects of gender that account for these impacts are gender roles and norms, gender
relations, gender identity and institutionalized gender. Gender identity matters in that the strength of
adherence to masculinities or femininities affects style and volume of drinking behaviour, with men
and sexual and gender minorities often drinking larger quantities of alcohol and more often than
women as a group. Gendered relations often mean that women are influenced by a partner’s

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 29
drinking and the impacts of alcohol reflect gender inequities such as vulnerability to sexual assault
and violence. Gender roles lead to women using alcohol to cope with stresses of caregiving roles,
trauma and IPV. Institutionalized gender differentially impacts women by applying increased stigma
to women who drink, and barriers to treatment for women and mothers who use alcohol.
2.5.3 How Do Sex and Gender Interact and Intersect with Other
Factors?
All these factors and processes are exacerbated by sex–gender interactions. For example, sex-
related and gender-related factors coincide to create specific and heightened negative impacts of
alcohol during pregnancy on both women’s and fetal health. Pregnancy-related processes affect the
pharmacokinetics of ingesting alcohol, while stigma and social policing are heightened during
pregnancy. Vulnerability to sexual assault is enhanced in the context of being young, female and
intoxicated, amid pervasive gender-based violence. Intersections, such as those with poverty,
racialization, past trauma, or sexual and gender minority status merge to create more harms.
2.5.4 How Does Alcohol Affect Reproduction?
Women’s and children’s reproductive health is compromised by alcohol use, particularly during
pregnancy and breastfeeding. Long-term damage to children can occur after being exposed to
alcohol in the womb, and alcohol use during breastfeeding can reduce milk production. Furthermore,
alcohol passes into breastmilk and therefore exposes the infant to alcohol. During pregnancy,
increased water and blood volume, along with the impact of alcohol on glucose and insulin lipid
metabolism, create complex effects on the body.
There is mixed evidence on the impact of alcohol on pregnancy and delivery outcomes, with possible
increases in miscarriage and placental abnormalities. However, exposure to alcohol in the womb
results in a well-established risk for learning, health and social effects that have a lifelong impact,
including brain injury, birth defects, health problems and diseases. Recent reviews that considered
low levels of exposure have also found some adverse effects, reinforcing the message that it is
safest not to drink during pregnancy. Effects of alcohol consumption on breastfeeding include a
decrease in milk production, early cessation of breastfeeding and effects on infant sleep patterns.
2.5.5 Discussion
Women are particularly susceptible to the negative effects of drinking alcohol. This is due to factors
related to both sex (biological) and gender (social). The female body’s response to alcohol results in
faster intoxication and more damage from lesser amounts of alcohol, and in a shorter time.
Gendered social and cultural factors about alcohol negatively affect girls and women via enhanced
stigma, social pressures, exploitative marketing and increased vulnerability to sexual assault and
IPV. Sex and gender, along with the determinants of health and intersecting factors, such as race,
age, income and education, shape the overall impacts of alcohol, resulting in differential impacts on
women, men and gender and sexual minorities. While all people living in Canada can benefit from
nuanced information and messaging about alcohol use and safe drinking levels, it is especially
important for women and girls.
Alcohol use also presents numerous sex- and gender-specific risks for reproductive processes such
as fertility and conception, pregnancy, breastfeeding and childcare. Males and females experience
differential alcohol-related reproductive risks and effects, at different life stages. Alcohol use during
pregnancy is particularly unsafe, as it heightens the risk of fetal alcohol spectrum disorder (FASD) in
offspring, often with lifelong disabilities and impacts. Gendered social attitudes about alcohol use

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 30
and reproduction mean that pregnant girls and women who use alcohol experience negative,
punitive and stigmatizing attitudes. In some jurisdictions, these manifest as state sanctioned
interventions, barriers to treatment or child apprehension.
2.5.6 What Are the Key Messages for Women?
The collective impact of sex, gender and interactive and intersectional factors on alcohol use has
particular importance for girls and women. It is necessary to transmit this emerging and growing
body of evidence to women, service providers, practitioners and policy makers to improve health
literacy and inform more specific and tailored prevention, treatment and harm reduction efforts.
• Female bodies can be more damaged by drinking, compared to males.
• Sex-related (biological) factors enhance the impact of alcohol, causing more harm and faster
intoxication in girls and women from lesser amounts.
• Gender-related (social) factors contribute to the negative impacts of alcohol in real life,
increasing vulnerability to marketing exploitation, stigma, sexual assault and IPV.
• Sex, gender and factors such as trauma and poverty interact and make dependence on alcohol,
treatment and recovery more difficult for women.
• Practitioners need to recognize both biological and social factors affecting alcohol use that
create differential impacts on and require tailored responses for women, men and gender and
sexual minorities.
2.6 Views, Preferences and Expectations About Guidelines
of People Living in Canada
Throughout this project, there was a commitment to consider the views, preferences and
expectations of people living in Canada about alcohol guidelines to improve the strength of updated
recommendations. Therefore, as evidence was being gathered on alcohol and health, parallel
activities were led to better understand people’s views about guidelines and to obtain insight on
alcohol, health and issues of well-being that matter most and are most useful to people living in
Canada.
Three different types of evidence were collected to inform experts’ deliberations and final decisions
for the updated guidelines: an update of a systematic review, a public consultation, interviews with
stakeholders.
2.6.1 Summary of Evidence on Understanding and Response to Alcohol
Guidelines
To learn about the acceptability and feasibility of the updated guidelines, the systematic review
previously prepared for the behavioural evidence expert group for the U.K. guidelines (Jones & Bellis,
2013) was updated with a focus on understandings and responses to official public health
guidelines. The update was prepared by Cochrane Canada. (See the full report here: Update of
Canada’s Low-Risk Alcohol Drinking Guidelines: Summary of Evidence on Understanding and
Response to Alcohol Consumption Guidelines.) Some of the results have proven to be of great
importance to the experts charged with making judgments about the acceptability and feasibility of
recommendations.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 31
• There appears to be little understanding among the public about what a standard drink is and
most times people overestimated the standard drink size. The public also overestimated the
number of daily and weekly standard drinks recommended in guidelines. Typically, people
indicated that those recommendations were unrealistic and did not want to count standard
drinks.
• Views about the amount of alcohol consumption that was not sensible or that was harmful were
often associated with excessive intake or “problem drinking,” but people often noted that their
own drinking was not a problem.
• Less than half the people who responded to surveys were aware of the harms of alcohol intake,
and there was less awareness in people who drink at high- or very high-risk levels. While some
people were aware of the harms, they still had a positive attitude toward alcohol use, especially
in social situations.
• People suggested that guidelines should include strategies to help apply the low-risk drinking
recommendations, such as refusing drinks when not really wanted or eating while drinking.
• The applicability to their own lives of guidelines generally and guidelines specifically for low-risk
drinking was questioned by the public with many reasons given for why guidelines might not be
applicable. For example, individual tolerance levels and physical reactions to alcohol can differ,
and the effects of different types of alcohol on an individual can also differ.
• While participants in the studies indicated that a health agency should provide
recommendations, they preferred advice rather than strict rules or patronizing messages.
• Overall, the experts considered these findings to indicate that regardless of the scientific quality
of the guidelines, to be credible updated guidelines must meet people where they are at. They
would have to bridge the gap between the way people consume alcohol and the evidence on the
health impacts by providing them with actionable guidance.
2.6.2 Public Consultation on Alcohol Guidelines
In spring 2021, CCSA held an online public consultation in which 4,845 people living in Canada
participated. (See the full report here: Update of Canada’s Low-Risk Alcohol Drinking Guidelines:
Summary of Findings from Public Consultation.) The consultation focused on the experiences of
people living in Canada with the current LRDGs and their needs and expectations for updated
guidelines. The public consultation revealed alcohol-related topics of importance to people living in
Canada that, in return, influenced the topics for which it was decided to conduct rapid reviews (see
previous section). The experts also retained two major lessons in terms of the type of information to
be emphasized and prioritized in the development of resources to promote the new guidelines:
• Among contributors who said they had used the 2011 LRDGs in the past, the most often cited
challenge with using the guidelines was “not wanting to follow the LRDGs.”
• The contributors shared an interest in understanding their risk of experiencing alcohol-related
harms and receiving information about long-term risks and benefits of alcohol use.
Both these results point to the importance of not only informing people about the existence of the
guidelines, but also about the reasons for their existence. Without fully understanding the risks
associated with alcohol use, people are unlikely to understand why they should follow the guidelines.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 32
2.6.3 Interviews with Stakeholders
To explore the familiarity and understanding of the 2011 LRDGs, and to discuss specific knowledge
mobilization recommendations including ideal messaging and communication strategies, Leger was
contracted to assist in the completion of eight virtual focus groups. A total of 48 persons representing
various health-related organizations were interviewed. The summary report, Commissioned Report:
Update on Canada’s Low-Risk Alcohol Drinking Guidelines: Summary of Stakeholder Focus Groups.
is available on CCSA’s LRDG webpage.
Overall, stakeholders were familiar with the LRDGs. They mentioned frequently referencing the
guidelines, which they found to be particularly useful to start a conversation about alcohol use and
drinking patterns. Still, they mentioned that encouraging people to follow alcohol guidelines was
challenging because awareness of the dangers of alcohol was low and people living in Canada
tended to normalize consuming alcohol.
Stakeholders mentioned that the goal of the updated guidelines should be to get people rethinking
their alcohol consumption. They requested a focus on the adverse effects of alcohol on overall
health and wellness, including information on alcohol being a known teratogen and carcinogen, and
its association with mental health and social harms. Messaging for teens and young adults should
focus on the immediate short-term impacts of drinking. Finally, many participants mentioned the
importance for updated guidelines to challenge the alcohol-centred culture and to include messaging
promoting a non-drinking culture. Participants also mentioned keeping the guidelines as simple as
possible and providing standard drink measurements that are easy to follow as the ideal approach to
conveying the guidelines.
In terms of resources, stakeholders said they wanted a variety of different types of information. They
also viewed infographics as important for communicating the updated guidelines. The guidelines
should be kept as simple as possible and providing standard drink measurements that are easy to
follow is viewed as the ideal approach to conveying them. In fact, the interviews further revealed a
firm belief among stakeholders that the public should be provided with information about standard
drink size, nutritional information and potential health risks related to consuming alcohol. Hence,
they expressed support for the addition of mandatory enhanced alcohol container labels with a
health message, drink guidelines, standard drink information and nutrition information.
Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 33
Standard Drink Labelling: A necessary condition for the adoption of the Guidance on Alcohol and
Health by the public
The concept of standard drink is central to understanding the Guidelines on Alcohol and Health.
To adhere to the guidance and reduce the risk of negative consequences due to alcohol,
consumers need consistent, easy-to-use information when serving alcohol to accurately track and
monitor their drinking.
In Canada, a standard drink is 17.05 ml or 13.45 g of pure alcohol, which is equivalent to:
• A bottle of beer (12 oz., 341 ml, 5% alcohol)
• A bottle of cider (12 oz., 341 ml, 5% alcohol)
• A glass of wine (5 oz., 142 ml, 12% alcohol)
• A shot glass of spirits (1.5 oz., 43 ml, 40% alcohol)
In practice, people in Canada have a limited understanding of a standard drink (Osiowy et al.,
2015; Public Health Ontario, 2017b). According to this project’s public consultation (Update of
Canada’s Low-Risk Alcohol Drinking Guidelines: Summary of Findings from Public Consultation),
38% of contributors said they had previously heard of the 2011 LRDGs. Among those who
reported using the guidelines, less than half (43%) said they were extremely familiar with the
concept of standard drink. When asked about challenges associated with using the 2011 LRDGs,
two of the three most popular answers were that it was not clear to them “what a standard drink
is” and that the standard drinks in the guidelines did not represent the types of alcoholic
beverages they typically drink. These results echo those of other studies showing that a lack of
knowledge about standard drinks can preclude people from adhering to guidelines, even if they
are aware of them and motivated to monitor and regulate their alcohol consumption (De Visser &
Birch, 2012; Dowling et al., 2006; Hawks, 1999).
Percent alcohol by volume (%ABV) information is mandated on alcohol beverage containers in
Canada. However, communicating alcohol content on beverage containers using %ABV
information is problematic because alcohol drinking guidelines are expressed in terms of standard
drinks. The inconsistency in messaging causes consumer confusion and creates barriers for
consumers to adhere to alcohol guidance. Standard Drink Labelling (SDL) can help consumers to
accurately monitor their alcohol use in terms of standard drinks (Osiowy et al., 2015; Wettlaufer,
2018). According to a 2022 systematic review of the impacts of alcohol container labels on
consumer outcomes, the evidence consistently suggests that compared to %ABV labels, exposure
to SDL results in more accurate estimates of the amount of alcohol in a standard drink, the
number of standard drinks in an alcohol container, and the number of standard drinks to reach
drink limit guidelines (Hobin et al., 2022). Evidence also indicates that by providing information at
the point of pour, SDL better supports accurately pouring one standard drink of alcohol relative to
%ABV labels (Brunk et al., 2020; Wettlaufer, 2018). In the only real-world experimental study
testing alcohol container labels, results suggest when consumers are exposed to SDL, they are
more likely to use the labels to drink within guidelines and accurately estimate the number of
standard drinks in their preferred drink (Schoueri‐Mychasiw et al., 2021).
Considering that:
• The concept of standard drink is central to understanding and following Canada’s Guidance on
Alcohol and Health;

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 34
• SDL can help consumers follow alcohol guidelines by monitoring their personal alcohol use;
and
• A fundamental idea underlying this project is that people living in Canada have a right to clear
information about alcohol;
A corollary of this project is a recommendation for Health Canada to require, through regulation,
the mandatory labelling of all alcoholic beverages on the number of standard drinks in a
container.
2.6.4 Focused Consultations with Indigenous People
Throughout the project, focused consultations were held with Indigenous people serving on the
LRDG Executive Committee or Scientific Expert Panels. These experts included Dr. Carol Hopkins,
Lenape Nation, Chief Executive Officer, Thunderbird Partnership Foundation; the late Harold
Johnson, Nehiyaw lawyer and author; and Dr. Christopher Mushquash, Anishinabek Professor,
Lakehead University, and Canada Research Chair in Indigenous Mental Health and Addiction.
The discussions began very broadly with regards to Indigenous peoples’ historical relationship with
alcohol (Johnson, 2016). The participants reflected on how alcohol has been used as a tool or
weapon of colonization from its first introduction during the fur trade. They recalled that the negative
impacts were so severe that the numbered treaties included a clause to ban alcohol from Indigenous
territory and communities. This prohibition led to the criminalization of alcohol sales, transportation
and consumption that in turn contributed to high levels of incarceration of Indigenous people,
negative stereotyping, racism and stigma. In the frontier context, binge drinking and related harms
like violence, injuries and accidents became pervasive (Ehrlander, 2010). Drinking alcohol became a
coping mechanism for dealing with trauma and grief resulting from the losses of self-government,
cultural practices, ceremonies, language and a viable economy, as well as the apprehension,
isolation and abuse of children in the Indian Residential Schools. Indigenous people’s situation
illustrates that the effects of alcohol are not the same for all people and communities.
In this larger context it is important to recognize the bi-modal drinking pattern amongst Indigenous
people. Compared to other adults in Canada, there are proportionately more First Nations adults who
do not use alcohol (42.6%) or engage in binge drinking (50.5%) (First Nations Information
Governance Centre, 2018). Using alcohol without binge drinking is uncommon (6.9%) and generally
confined to those who are urban, and have more education and greater career responsibilities. In
most communities, tribal councils and Indigenous organizations, the emphasis has been on
abstinence-based treatment programs with a strong cultural content. The latter serves to reinforce
Indigenous identity with the exploration of hope, belonging, meaning and purpose (Assembly of First
Nations et al., 2011; Thunderbird Partnership Foundation, 2015). Nevertheless, pragmatic harm
reduction strategies have also been embraced by Indigenous communities.
Because of the above considerations, the Indigenous experts questioned the relevance of the LRDGs
for Indigenous people, in terms of the enormity of the challenges with alcohol, the inequity in
resources to address alcohol at the community level, and the cultural and historical contexts
regarding alcohol. They emphasized that in most Indigenous communities wellness is more oriented
toward abstinence than low-risk alcohol use (Thunderbird Partnership Foundation, 2015). They
further expressed concern that an Indigenous commentary or takeaway, without the correct context,
would simply reinforce systemic racism, negative stereotyping and stigma. Instead, it was suggested
that broad social determinants of health need to be recognized and linked to policies, like
addressing epistemic racism through ensuring Indigenous culture is the foundation of policy and

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 35
programs, poverty reduction, income security, accessible employment and colonialism diminishment
(Czyzewski, 2011).
On a smaller scale, Indigenous experts agreed that Indigenous peoples should be involved in
developing knowledge mobilization practices for their people and the following initiatives should be
prioritized for development:
• A risk-based approach to increase alcohol literacy, aligned with the culturally congruent focus on
wellness;
• A harm reduction initiative to promote substance use health among those who choose to use
alcohol, focused on how to reduce the harms of alcohol consumption to self, families and
Indigenous communities; and
• Community-based alcohol interventions, framed as community-based alcohol strategies, with
appropriate guidance, knowledge mobilization and resources.
A narrative approach identifying risk factors, resiliency and the success of different communities was
encouraged. Evaluation resources should accompany the development of these initiatives to ensure
they meet their intended goals. Each objective should be funded to ensure that alcohol issues are
explored and addressed in the appropriate historical and cultural context, guided by an evidence-
based, culturally relevant approach, and using enhanced community-based resources.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 36
Part 3: Experts’ Recommendations
Canada’s LRDGs were originally published in November 2011 and the evidence since then on the
association between drinking alcohol and physical, mental and social harms has continuously
evolved. An update of the guidelines was required to take into account these advancements in what
we know about the risks and benefits associated with alcohol. In July 2020, with the support of
Health Canada, CCSA was mandated to update Canada’s LRDGs. The project has been guided by a
public health perspective and its stated focus has been to provide people living in Canada with the
latest evidence-based advice on alcohol to support them in making informed decisions about its use.
When the update of Canada’s LRDGs was initiated, it was anticipated that the new guidelines would
set lower limits for alcohol use. This was, in part, due to several trends that have emerged since the
guidelines were released in 2011: that alcohol use was a risk factor for an increasing number of
diseases; an important proportion of alcohol-attributable deaths in Canada were among people
adhering to the 2011 guidelines; and alcohol guidelines coming from other countries in recent years
had all recommended limits below the 2011 Canadian guidelines. What was not anticipated was
that the evidence review would reveal the extent to which even very small amounts of alcohol can be
harmful to people’s health and well-being. In this context, the experts have agreed to replace
Canada’s LRDGs with Canada’s Guidance on Alcohol and Health.
3.1 Canada’s Guidance on Alcohol and Health
Throughout the life course, there are established thresholds of mortality risk that people are willing
to accept (BMJ Best Practice, n.d.; Starr, 1969). For voluntary activities like unprotected sexual
practices or smoking cigarettes, that level is a 1 in 1,000 mortality risk (i.e., people are willing to
accept a 1 in 1,000 risk of death when participating in these activities). For alcohol, people
appear willing to accept a higher risk of death associated with consumption as compared with
other voluntary activities. It is not uncommon for countries to base their guideline recommendations
on a 1 in 100 mortality risk limit (e.g., Australia, France, U.K.). This project revealed that in Canada,
the limit associated with a 1 in 1,000 chance of premature death related to an alcohol condition is
two standard drinks per week, while the 1 in 100 risk limit is six standard drinks per week.
There is a continuum of risk whereby the risk for those who consume two standard drinks or less per
week is negligible to low; it is moderate for those who consume between three and six standard
drinks per week; and it is increasingly high for those who consume more than six standard drinks per
week.
In light of results obtained through this project’s knowledge mobilization activities and with a view to
meet people where they are at, the experts are unanimous that instead of providing people with
strict rules and recommendations, people living in Canada should be presented with a continuum of
risk associated with various levels of alcohol use. The experts anticipate that a continuum of risk will
allow people to situate themselves where they are on that continuum and understand in which risk
zone their alcohol use places them. It is hoped that this will lead people to develop intentions to
adopt healthier and safer behaviours (i.e., to move toward a less risky drinking zone along that
continuum). Presenting people living in Canada with a continuum is also a direct response to
stakeholders’ wishes for the new guidance to be broadly relatable to all segments of the population,
reflecting the different ways people living in Canada use alcohol and the unique health and social
outcomes associated with those patterns of use.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 37
The weekly number of standard drinks that delineate
the continuum’s risk zones align with weekly
recommendations in the U.K. (8.3 standard drinks),
Australia, Denmark, France
(7.4 standard drinks) and
the Netherlands (5.2 standard drinks). In Canada,
among persons aged 15 and older, about a fifth of
females (23%) and males (21%) do not drink alcohol,
27% of females and 16% of males usually consume
less than two standard drinks per week; 19% of
females and 15% of males consume three to six
standard drinks per week on average and a third of females (32%) and half of males (49%) usually
consume more than six standard drinks per week. These proportions are based on two data sources:
World Health Organization (2021) and Statistics Canada (2018).
The continuum of risk is based on average quantities of alcohol people consume per week and the
impact it has on their physical health. Therefore, the experts looked at other types of evidence to
support people living in Canada who may wonder about the consequences of occasional drinking or
immediate effects that could fall outside the realm of physical health. From that line or inquiry, there
is a second takeaway: On any occasion, the risk of a negative acute outcome begins to increase
with any consumption, and with more than two standard drinks, most individuals will have an
increased risk of injuries or other problems.
It is not lost on the experts that this new Guidance on Alcohol and Health, which puts forward a
continuum of risk, will be surprising and unsettling to large segments of the population, including the
alcohol industry, media and policy makers. However, people living in Canada have a right to know.
Alcohol is a carcinogen related to at least seven types of cancer, including common ones like colon and
breast cancer. Furthermore, in contrast to common perceptions, current evidence shows that
drinking a little alcohol does not decrease the risk of heart disease. In fact, alcohol consumption can
lead to cardiovascular diseases and lower respiratory infections, as well as injuries resulting from
violence and road crashes. Hence, this project has confirmed that less is better when it comes to
drinking alcohol and from this fact, it is necessary to promote the message that it is okay not to
drink alcohol.
An encouraging fact associated with this new evidence is that every standard drink counts and any
reduction in alcohol use is beneficial. Research demonstrates that many harms related to chronic
disease caused by alcohol are reversible. People who decrease their alcohol consumption
experience improvements in liver function, insulin resistance, weight, blood pressure and cancer-
related growth factors (Mehta et al., 2018; Thomes et al., 2021). Reductions in alcohol use further
decrease hypertension (Roerecke et al., 2017) and reduce the risk of cancer, atrial fibrillation,
stroke, diabetes, pancreatitis and liver cirrhosis (Heckley et al., 2011; Lee et al., 2021; Nikkola et al.,
2013; Verrill et al., 2009; Voskoboinik et al., 2020; Wu et al., 2021). In addition, the risk of infectious
diseases, epilepsy and injuries are affected by the acute effects of alcohol and reductions in alcohol
use will immediately decrease the risk of these outcomes (Imtiaz et al., 2017; A. Samokhvalov et al.,
2010a; Samokhvalov et al., 2010b; Taylor et al., 2010). Hence, it is never too late to reduce alcohol
consumption.
Among people living in Canada aged
15 and older, one fifth (20%) do not
drink alcohol, another fifth (21%)
consume less than two standard
drinks per week on average, 17%
consume three to six standard drinks
per week and 40% consume more
than six standard drinks per week.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 38
Another surprising finding of this project is that at low levels of consumption the physiological
differences in the lifetime risk of death due to alcohol between women and men is minimal.
However, the experts are unequivocal in stating that this should not distract from the evidence that
lifetime risk of harm increases more steeply for women than for men when we move above the
lowest risk levels. On the one hand, biological factors enhance the impact of alcohol, causing more
harm and faster intoxication on lesser amounts in girls and women. On the other hand, girls and
women suffer disproportionately from social factors that contribute to the negative impacts of
alcohol in real life, such as increasing vulnerability to marketing exploitations, stigma, sexual assault
and IPV.
On this note, the experts find it imperative to highlight that men’s vulnerability to alcohol should not
be overlooked. The work completed in this project has shown that men are more likely than women
to experience and cause alcohol-related harms. Men drink more alcohol than women do and are
more likely to drink in excess. As a consequence, they are more likely to be involved in alcohol-
impaired driving collisions, to be treated in hospitals and hospitalized for alcohol-related medical
emergencies and health problems, to be diagnosed with an alcohol use disorder, and to die from
alcohol-related causes (Canadian Institute for Health Information, 2022; Canadian Substance Use
Costs and Harms, 2020; Rehm et al., 2006; Statistics Canada, 2021). Alcohol is also more strongly
associated with perpetration of violence for men then for women. Disproportionately more injuries,
violence and deaths result from men’s drinking.
Finally, reproductive health is compromised by alcohol use and people living in Canada need to be
reminded that alcohol is a teratogen that can cause learning, health and social effects that have a
lifelong impact, including brain injury, birth defects, behavioural problems, learning disabilities and
other health problems. These adverse effects are observed at relatively low levels of exposure or
short-term exposure to high levels of consumption, so it is safest not to drink while pregnant and
during the pre-conception period.
Canada’s Guidance on Alcohol and Health, Seven Key Takeaway Messages
1. All levels of alcohol consumption are associated with some risk, so drinking less is better for
everyone.
2. Among healthy individuals, there is a continuum of risk for alcohol-related harms whereby the
risk is:
• Negligible to low for individuals who consume two standard drinks or less per week;
• Moderate for those who consume between three and six standard drinks per week; and
• Increasingly high for those who consume more than six standard drinks per week.
3. On any occasion, any level of consumption has risks, and with more than two standard drinks,
most individuals will have an increased risk of injuries or other problems
4. Disproportionately more injuries, violence and deaths result from men’s drinking.
5. Above low levels of alcohol consumption, the health risks increase more steeply for women
than for men.
6. It is safest not to drink alcohol while pregnant and during the pre-conception period.
7. For women who are breastfeeding, it is safest not to use alcohol.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 39
Alcohol consumption can also negatively impact breastfeeding by causing a decrease in milk
production, early cessation of breastfeeding and effects on infant sleep patterns. Alcohol enters
breast milk through passive diffusion within 30 to 60 minutes following ingestion, so breastfeeding
infants can be exposed to alcohol through breastmilk. However, infants are unable to metabolize
alcohol. Therefore, for women who are breastfeeding, it is safest not to use alcohol.
3.2 Moving Forward
In light of the new Guidance on Alcohol and Health, as well as the fact that alcohol literacy in the
population is low (Canadian Centre on Substance Use and Addiction, 2021), substantial and
sustained efforts will be required to develop messaging that speaks directly to the unique
concerns of people with diverse backgrounds and personal experiences. For example, novel work
developed in parallel to this project has shown that alcohol consumers aged 18 to 30 may be more
receptive to health messaging about the effects of their alcohol use on life expectancy, than to
messages which simply present a guideline (Stockwell et al., 2022). Others may want to direct their
prevention efforts toward young adults, particularly boys and young men since aggression and
violence decreases with age and is perpetrated more by men than women. Recommendations and
suggestions, particularly in relation to sex and gender, have also been prepared in connection with
this project and are available to those who would like to build a campaign around them (Appendix 3).
Furthermore, the involvement of health professionals, family doctors and nurses, who are crucial
allies with immense credibility in explaining the continuum of risks associated with alcohol to patients
and the general public, will also be required. By doing so, they may make a valuable contribution to
health care by reducing direct alcohol-related costs; we will return to this issue below.
People living in Canada should “Learn the facts. Parse the fictions. Act accordingly.”
7
To do so, they
will need more than plain and clear information, no matter how effective newly developed target
campaigns will be. Alcohol, like tobacco or processed foods, has been termed a “sinful good,”
meaning that when people use it, they get the pleasure now and suffer the consequences later. To
make wise decisions about such goods, people need encouragement (Thaler & Sunstein, 2008).
People living in Canada who want to move toward the lower end of the continuum of alcohol-related
risks need an environment that supports healthier and safer decisions. To move away from an
alcogenic culture (Johnston, 2014), there needs to be a cultural shift. Therefore, a corollary to the
current project is the requirement for governments to design a healthier environment that will
help people make difficult decision making about alcohol a little easier.
First and foremost, for people living in Canada to adhere to the Guidance on Alcohol and Health,
evidence shows consumers need consistent, easy-to-use information on alcohol containers to
accurately track and monitor their alcohol use in terms of standard drinks. While beer remains the
alcoholic beverage of choice for people living in Canada, the growing craft movement is resulting in a
variety of alcohol content and sizes of cans and bottles being available for consumption at home.
Now more than ever, to count how many standard drinks they consume, people need information at
the point of pour. While Canada is a world leader in mandating enhanced labels on tobacco and
cannabis packages, alcohol containers are exempt from these requirements. Enhanced alcohol
container labels are an increasingly popular strategy for providing information to consumers, and a
key recommendation by national and international health organizations (Jané-Llopis et al., 2020;
Vallance et al., 2021; World Health Organization, 2022). A direct consequence of the current project
7
The expression comes from an opinion letter entitled Drinking skyrocketed during COVID-19. Why’s it so hard to learn the facts about
alcohol? It was written by Alec Bruce and published in The Globe and Mail on Nov. 12, 2021.
https://www.theglobeandmail.com/opinion/article-drinking-skyrocketed-during-covid-19-whys-it-so-hard-to-learn-the/

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 40
is a recommendation for Health Canada to require, through regulation, the mandatory labelling of
all alcoholic beverages on the number of standard drinks in a container.
Many studies have shown that people are most likely to follow guidance if they know the reasons
why they should (Pettigrew et al., 2021; Wakefield et al., 2018). Our public consultation revealed
that without understanding the risks and benefits associated with alcohol use, people are unlikely to
understand why they should follow the guidelines. Therefore, the requirement for standard drink
labelling should be followed by a requirement to label all alcoholic beverages with health
warnings and nutrition information. Labelling may be an important intervention in a more
comprehensive alcohol strategy (Kokole et al., 2021). Evidence has shown that adding health
warnings to alcohol labels can increase public awareness of the causal link with cancer and reduce
per capita alcohol consumption. They can also strengthen public support for policies that are often
unpopular but known to reduce population-level alcohol-caused harms (Weerasinghe et al., 2020).
To support people living in Canada who want to move toward the less risky end of the continuum,
governments will need to be involved on other policy fronts. Cost-effective policies and feasible
interventions that reduce the overall level of alcohol consumption are well documented at the global,
national and provincial levels (Vallance et al., 2021; World Health Organization, 2022). For example,
work conducted by the Canadian Alcohol Policy Evaluation committee and the National Alcohol
Strategy Advisory Committee has highlighted that measures such as strengthened regulations of
alcohol advertising and marketing, restrictions on the physical availability of alcohol, and the
adoption of a minimum price for alcohol sold are all beneficial to public health. If the new Guidance
on Alcohol and Health were to facilitate policy discussions and initiatives, the effects could be
considerable and extend beyond the public health sphere to include economic benefits.
The Canadian Substance Use Costs and Harms study (Canadian Substance Use Costs and Harms,
2020) has revealed that the annual direct costs of alcohol are $16.7 billion, far more than the direct
costs associated with tobacco ($12.3 billion), opioids ($5.9 billion) or cannabis ($3.2 billion), and far
exceeding the value of the revenue produced by alcohol sales and taxation, which was last estimated
to be $13.5 billion (Statistics Canada, 2021).
Hence, by adopting policies to support healthier and
safer decisions around alcohol use, government may save money and reduce per-person costs
attributable to alcohol use in Canada, most recently estimated at $455 per year (Canadian
Substance Use Costs and Harms, 2020).
3.2 Conclusion
The new Guidance on Alcohol and Health reflects the conclusions drawn from global evidence
reviews, mathematical modelling, consultations with the public and experts, and discussions. It is
hoped that this work will be useful to people living in Canada who are health conscious and want to
know more about the effects of alcohol consumption on their well-being. The Guidance on Alcohol
and Health was developed for them to make informed decisions about their alcohol use.
The Guidance on Alcohol and Health requires a cultural shift that, by and large, can only be
orchestrated by governments through policies and collaboration with employers, healthcare
providers and community stakeholders to make people aware and better at managing their risks.
Hence, the evidence reviewed and presented here should influence provincial and federal
governments to implement alcohol policies focused on reducing alcohol-related harms and
promoting health and wellness. Information and advice are useful and necessary for people in
Canada, but an environment supporting healthier and more informed-behaviour choices around
alcohol is an absolute pre-requisite for a healthy society.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 41
References
Alpert, H. R., Slater, M. E., Yoon, Y. H., Chen, C. M., Winstanley, N., & Esser, M. B. (2022). Alcohol
consumption and 15 causes of fatal injuries: A systematic review and meta-analysis. American
Journal of Preventive Medicine, Article S0749-3797(22)00183-0. Advance online publication.
https://doi.org/10.1016/j.amepre.2022.03.025
Assembly of First Nations, National Native Addictions Partnership Foundation & Health Canada.
(2011). Honouring our strengths: A renewed framework to address substance abuse issues
among First Nations people in Canada. https://thunderbirdpf.org/wp-
content/uploads/2014/02/Honouring-Our-Strengths-2011_Eng1.pdf
Bagnardi, V., Rota, M., Botteri, E., Tramacere, I., Islami, F., Fedirko, V., … La Vecchia, C. (2015).
Alcohol consumption and site-specific cancer risk: A comprehensive dose–response meta-
analysis. British Journal of Cancer, 112(3), 580–593. https://doi.org/10.1038/bjc.2014.579
Bergeron, C. D., Tremblay-Antoine, C. D. B.-C., Morin, R., April, N., & Cloutier, A. (2020). La
consommation d’alcool : qu’en pense la population du Québec?
https://www.inspq.qc.ca/sites/default/files/publications/2772-consommation-alcool-
population-quebec.pdf
Blomberg, R. D., Peck, R. C., Moskowitz, H., Burns, M., & Fiorentino, D. (2009). The Long Beach/Fort
Lauderdale relative risk study. Journal of Safety Research, 40(4), 285–292.
https://doi.org/10.1016/j.jsr.2009.07.002
BMJ Best Practice. (n.d.). Understanding risk. https://bestpractice.bmj.com/info/toolkit/practise-
ebm/understanding-risk/
Brabete, A. C., Greaves, L., Hemsing, N., & Stinson, J. (2020). Sex- and gender-based analysis in
cannabis treatment outcomes: A systematic review. International Journal of Environmental
Research and Public Health, 17(3), Article 872. https://doi.org/10.3390/ijerph17030872
Brewer, R. D., & Swahn, M. H. (2005). Binge drinking and violence. JAMA, 294(5), 616–618.
https://doi.org/10.1001/jama.294.5.616
Broholm, K., Galluzzo, L., Gandin, C., Ghirini, S., Ghiselli, A., Jones, L., … Mäkelä, P. (2016). Good
practice principles for low risk drinking guidelines. Helsinki, Finland: National Institute for Health
and Welfare (THL).
https://www.julkari.fi/bitstream/handle/10024/131322/WP5%20Good%20practice%20low%2
0risk%20guidelines.pdf?sequence=1&isAllowed=y
Brunk, E., Becker, M. W., & Bix, L. (2020). Empirical evaluation of the presence of a label containing
standard drinks on pour accuracy among US college students. PloS one, 15(11), Article
e0241583. https://doi.org/10.1371/journal.pone.0241583
Butt, P., Beirness, D., Gliksman, L., Paradis, C., & Stockwell, T. (2011). Alcohol and health in Canada:
A summary of evidence and guidelines for low-risk drinking. Ottawa, ON: Canadian Centre on
Substance Abuse. https://www.ccsa.ca/sites/default/files/2019-04/2011-Summary-of-
Evidence-and-Guidelines-for-Low-Risk%20Drinking-en.pdf
Canadian Centre on Substance use and Addiction. (2014). Recalculating risky drinking in women.
Ottawa, Ont.,: Author.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 42
Canadian Centre on Substance Use and Addiction. (2021). Update of Canada’s Low-Risk Alcohol
Drinking Guidelines: Summary of findings from public consultation. Ottawa, Ont.: Author.
https://www.ccsa.ca/sites/default/files/2021-09/CCSA-Lower-Risk-Drinking-Guidelines-
Summary-Findings-Public-Consultation-2021-en_0.pdf
Canadian Institute for Health Information. (2022). Hospitalizations entirely caused by alcohol.
https://yourhealthsystem.cihi.ca/hsp/inbrief?lang=en#!/indicators/061/hospitalizations-
entirely-caused-by-alcohol/;mapC1;mapLevel2;/
Canadian Substance Use Costs and Harms Scientific Working Group. (2020). Canadian substance
use costs and harms 2015–2017. (Prepared by the Canadian Institute for Substance Use
Research and the Canadian Centre on Substance Use and Addiction.) Ottawa, Ont.: Canadian
Centre on Substance Use and Addiction. https://csuch.ca/publications/CSUCH-Canadian-
Substance-Use-Costs-Harms-Report-2020-en.pdf
Centers for Disease Control and Prevention. (2022). Binge drinking.
https://www.cdc.gov/alcohol/fact-sheets/binge-drinking.htm
Cherpitel, C. J., Ye, Y., Bond, J., Borges, G., & Monteiro, M. (2015). Relative risk of injury from acute
alcohol consumption: modeling the dose–response relationship in emergency department data
from 18 countries. Addiction, 110(2), 279–288. https://doi.org/10.1111/add.12755
Chikritzhs, T., Stockwell, T., Naimi, T., Andreasson, S., Dangardt, F., & Liang, W. (2015). Has the
leaning tower of presumed health benefits from ‘moderate’ alcohol use finally collapsed?
Addiction, 110(5), 726–727. https://doi.org/10.1111/add.12828
Compton, R. P. & Berning, A. (2015, February). Drug and alcohol crash risk. (Traffic Safety Facts
Research Note. DOT HS 812 117). Washington, DC: National Highway Traffic Safety
Administration. https://www.nhtsa.gov/staticfiles/nti/pdf/812117-
Drug_and_Alcohol_Crash_Risk.pdf
Czyzewski, K. (2011). Colonialism as a broader social determinant of health. The International
Indigenous Policy Journal,2(1) Article 5. https://doi.org/10.18584/iipj.2011.2.1.5
Dawson, D. A., Grant, B. F., & Li, T. K. (2005). Quantifying the risks associated with exceeding
recommended drinking limits. Alcoholism, Clinical and Experimental Research, 29(5), 902–908.
https://doi.org/10.1097/01.alc.0000164544.45746.a7
de Visser, R. O., & Birch, J. D. (2012). My cup runneth over: Young people’s lack of knowledge of low-
risk drinking guidelines. Drug and Alcohol Review, 31(2), 206–212.
https://doi.org/10.1111/j.1465-3362.2011.00371.x
Devries, K. M., Child, J. C., Bacchus, L. J., Mak, J., Falder, G., Graham, K., Watts, C., & Heise, L.
(2014). Intimate partner violence victimization and alcohol consumption in women: A systematic
review and meta-analysis. Addiction, 109(3), 379–391. https://doi.org/10.1111/add.12393
Dietary Guidelines Advisory Committee. (2020). Scientific report of the 2020 Dietary Guidelines
Advisory Committee: Advisory report to the Secretary of Agriculture and the Secretary of Health
and Human Services. Washington, DC: U.S. Department of Agriculture, Agricultural Research
Service. https://doi.org/10.52570/DGAC2020
Dowling, N., Clark, D. & Corney, T. (2006) Responsible drinking knowledge: A comparison of
Australian apprentices and university students. Youth Studies Australia, 25 (3). pp. 42–48

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 43
Ehrlander, M. (2010). The historical roots of a frontier alcohol culture: Alaska and northern Canada.
The Northern Review, 32, 63–103. https://thenorthernreview.ca/index.php/nr/article/view/14
Fillmore, M.T. & Jude, R. (2011), Defining “binge” drinking as five drinks per occasion or drinking to a
.08% BAC: Which is more sensitive to risk?. The American Journal on Addictions, 20, 468–475.
https://doi.org/10.1111/j.1521-0391.2011.00156.x
First Nations Information Governance Centre. (2018). National report of the First Nations Regional
Health Survey, Phase 3: Volume One. Ottawa, Ont.: Author. https://fnigc.ca/wp-
content/uploads/2020/09/713c8fd606a8eeb021debc927332938d_FNIGC-RHS-Phase-III-
Report1-FINAL-VERSION-Dec.2018.pdf
Hawks D. (1999). Not much to ask for, really! The introduction of standard drink labelling in
Australia. Addiction, 94(6), 801–811. https://doi.org/10.1046/j.1360-0443.1999.9468014.x
Health Canada. (2019). Canadian Alcohol and Drugs Survey (CADS): Summary of results for 2019.
https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2019-
summary.html
Health Canada. (2021). Canadian Postsecondary Education Alcohol and Drug Use Survey,
2019/2020. https://health-infobase.canada.ca/alcohol/cpads/
Heckley, G. A., Jarl, J., Asamoah, B. O., & G-Gerdtham, U. (2011). How the risk of liver cancer changes
after alcohol cessation: a review and meta-analysis of the current literature. BMC Cancer, 11,
Article 446. https://doi.org/10.1186/1471-2407-11-446
Hobin, E., Jansen, R., Vanderlee,. L., & Berenbaum, E. (2022). Enhanced alcohol container labels: A
systematic review. Ottawa, Ont.: Canadian Centre on Substance Use and Addiction.
https://www.ccsa.ca/sites/default/files/2022-02/CCSA-Enhanced-Alcohol-Container-Labels-
Systematic-Review-Report-en.pdf
Holmes, J., Angus, C., Meier, P. S., Buykx, P., & Brennan, A. (2019). How should we set consumption
thresholds for low risk drinking guidelines? Achieving objectivity and transparency using
evidence, expert judgement and pragmatism. Addiction, 114(4), 590–600.
https://doi.org/10.1111/add.14381
Imtiaz, S., Shield, K. D., Roerecke, M., Samokhvalov, A. V., Lönnroth, K., & Rehm, J. (2017). Alcohol
consumption as a risk factor for tuberculosis: meta-analyses and burden of disease. European
Respiratory Journal, 50(1), Article 1700216. https://doi.org/10.1183/13993003.00216-2017
Institute for Health Metrics and Evaluation. (2018). Data visualizations: GBD compare. Seattle,
Washington: Author. https://vizhub.healthdata.org/gbd-compare/
International Agency for Research on Cancer. (2012). Personal habits and indoor combustions,
Volume 100 E: A review of human carcinogens. Lyon, France: Author.
https://monographs.iarc.who.int/wp-content/uploads/2018/06/mono100E.pdf
Jané-Llopis, E., Kokole, D., Neufeld, M., Hasan, O. S. M., & Rehm, J. (2020). What is the current
alcohol labelling practice in the WHO European Region and what are barriers and facilitators to
development and implementation of alcohol labelling policy? Copenhagen: WHO Regional Office
for Europe (Health Evidence Network Synthesis Report, No. 68).
https://www.ncbi.nlm.nih.gov/books/NBK558550/
Johnson, H. (2016). Firewater: How alcohol is killing my people (and yours). Regina, Sask.: University
of Regina Press.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 44
Johnston, A. D. (2014). Drink: The intimate relationship between women and alcohol. Harper Collins.
Jones, L., & Bellis, M. A. (2013). CMO alcohol guidelines review: A summary of the evidence on
understanding and response to public health guidelines. Liverpool, England: Centre for Public
Health. https://www.drugsandalcohol.ie/25026/1/LJMU_CMO-Alcohol-Guidelines-Behavioural-
Review.pdf
Knott, C., Bell, S., & Britton, A. (2015). Alcohol consumption and the risk of type 2 diabetes: A
systematic review and dose-response meta-analysis of more than 1.9 million individuals from 38
observational studies. Diabetes Care, 38(9), 1804–1812. https://doi.org/10.2337/dc15-0710
Kokole, D., Anderson, P., & Jané-Llopis, E. (2021). Nature and potential impact of alcohol health
warning labels: A scoping review. Nutrients, 13(9), Article 3065.
https://doi.org/10.3390/nu13093065
Larsson, S. C., Burgess, S., Mason, A. M., & Michaëlsson, K. (2020). Alcohol consumption and
cardiovascular disease: A mendelian randomization study. Circulation: Genomic and Precision
Medicine, 13(3), Article e002814. https://doi.org/10.1161/CIRCGEN.119.002814
Larsson, S. C., Drca, N., & Wolk, A. (2014). Alcohol consumption and risk of atrial fibrillation: a
prospective study and dose-response meta-analysis. Journal of the American College of
Cardiology, 64(3), 281–289. https://doi.org/10.1016/j.jacc.2014.03.048
Larsson, S. C., Wallin, A., Wolk, A., & Markus, H. S. (2016). Differing association of alcohol
consumption with different stroke types: A systematic review and meta-analysis. BMC Medicine,
14, Article 178. https://doi.org/10.1186/s12916-016-0721-4
Laslett, A.-M., Room, R., Waleewong, O., Stanesby, O., & Callinan, S. (2019). Harm to others from
drinking: Patterns in nine societies. World Health Organization.
https://apps.who.int/iris/handle/10665/329393
Lee, S.-R., Choi, E.-K., Jung, J.-H., Han, K.-D., Oh, S., & Lip, G. Y. H. (2021). Lower risk of stroke after
alcohol abstinence in patients with incident atrial fibrillation: A nationwide population-based
cohort study. European Heart Journal, 42(46) 4759–4768.
https://doi.org/10.1093/eurheartj/ehab315
Liu, F., Liu, Y., Sun, X., Yin, Z., Li, H., Deng, K., … Hu, D. (2020). Race- and sex-specific association
between alcohol consumption and hypertension in 22 cohort studies: A systematic review and
meta-analysis. Nutrition, Metabolism and Cardiovascular Diseases, 30(8), 1249–1259.
https://doi.org/10.1016/j.numecd.2020.03.018
Llerena, S., Arias-Loste, M. T., Puente, A., Cabezas, J., Crespo, J., & Fábrega, E. (2015). Binge
drinking: Burden of liver disease and beyond. World Journal of Hepatology, 7(27), 2703–2715.
https://doi.org/10.4254/wjh.v7.i27.2703
Lu, P.-Y., Shu, L., Shen, S.-S., Chen, X.-J., & Zhang, X.-Y. (2017). Dietary patterns and pancreatic
cancer risk: A meta-analysis. Nutrients, 9(1), Article 38. http://dx.doi.org/10.3390/nu9010038
Mehta, G., Macdonald, S., Cronberg, A., Rosselli, M., Khera-Butler, T., Sumpter, C., … Moore, K. P.
(2018). Short-term abstinence from alcohol and changes in cardiovascular risk factors, liver
function tests and cancer-related growth factors: A prospective observational study. BMJ Open,
8(5), Article e020673. https://doi.org/10.1136/bmjopen-2017-020673
Midanik, L. T. (1999). Drunkenness, feeling the effects and 5+ measures. Addiction, 94(6), 887–
897. https://doi.org/10.1046/j.1360-0443.1999.94688711.x

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 45
Miller, W. R., Heather, N., & Hall, W. (1991). Calculating standard drink units: International
comparisons. British Journal of Addiction, 86(1), 43–47. https://doi.org/10.1111/j.1360-
0443.1991.tb02627.x
Mukamal, K. J., Maclure, M., Muller, J. E., & Mittleman, M. A. (2005). Binge drinking and mortality
after acute myocardial infarction. Circulation, 112(25), 3839–3845.
https://doi.org/10.1161/CIRCULATIONAHA.105.574749
Naimi, T. S., Blanchette, J., Nelson, T. F., Nguyen, T., Oussayef, N., Heeren, T. C., … Xuan, Z. (2014). A
new scale of the U.S. alcohol policy environment and its relationship to binge drinking. American
Journal of Preventive Medicine, 46(1), 10–16. https://doi.org/10.1016/j.amepre.2013.07.015
Naimi, T. S., Brewer, R. D., Mokdad, A., Denny, C., Serdula, M. K., & Marks, J. S. (2003). Binge
drinking among US adults. JAMA, 289(1), 70–75. https://doi.org/10.1001/jama.289.1.70
National Health and Medical Research Council. (2020). Australian guidelines to reduce health risks
from drinking alcohol. Canberra, Australia: Author. https://www.nhmrc.gov.au/about-
us/publications/australian-guidelines-reduce-health-risks-drinking-alcohol
National Institute of Alcohol Abuse & Alcoholism. (2004). NIAAA council approves binge drinking
definition. NIAAA Newsletter, 2004(3), 3.
http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf
Newton, S., Morona, J., Salinger, K., & Merlin, T. (2018). Systematic literature review on the
association between alcohol consumption and mental health disorders. Adelaide, South
Australia: Adelaide Health Technology Assessment.
https://www.nhmrc.gov.au/sites/default/files/documents/attachments/Alcohol/4-tech-report-
systematic-review.pdf
Nikkola, J., Räty, S., Laukkarinen, J., Seppänen, H., Lappalainen-Lehto, R., Järvinen, S., Nordback, I.,
& Sand, J. (2013). Abstinence after first acute alcohol-associated pancreatitis protects against
recurrent pancreatitis and minimizes the risk of pancreatic dysfunction. Alcohol and Alcoholism,
48(4), 483–486. https://doi.org/10.1093/alcalc/agt019
Osiowy, M., Stockwell, T., Zhao, J., Thompson, K., & Moore, S. (2015). How much did you actually
drink last night? An evaluation of standard drink labels as an aid to monitoring personal
consumption. Addiction Research & Theory, 23(2), 163–169.
https://doi.org/10.3109/16066359.2014.955480
Paradis, C. (2016). Canada’s National Alcohol Strategy: It’s time to assess progress. Canadian
Journal of Program Evaluation, 31(2), 232–241.
https://journalhosting.ucalgary.ca/index.php/cjpe/article/view/31045
Paula, T., Chagas, C., Martins, L. B., & Ferri, C. P. (2020). Low-risk drinking guidelines around the
world: An overview of the current situation. Addictive Disorders & Their Treatment, 19(4), 218–
227. https://doi.org/10.1097/ADT.0000000000000225
Pettigrew, S., Booth, L., Jongenelis, M. I., Brennan, E., Chikritzhs, T., Hasking, P., … Wakefield, M.
(2021). A randomized controlled trial of the effectiveness of combinations of ‘why to reduce’ and
‘how to reduce’ alcohol harm-reduction communications. Addictive Behaviors, 121, Article
107004. https://doi.org/10.1016/j.addbeh.2021.107004
Public Health Ontario. (2017a). Alcohol: Awareness and knowledge of Canada’s Low Risk Drinking
Guidelines (LRDG) [Infographic]. https://www.publichealthontario.ca/-
/media/Documents/A/2017/alcohol-lrdg.pdf?sc_lang=en
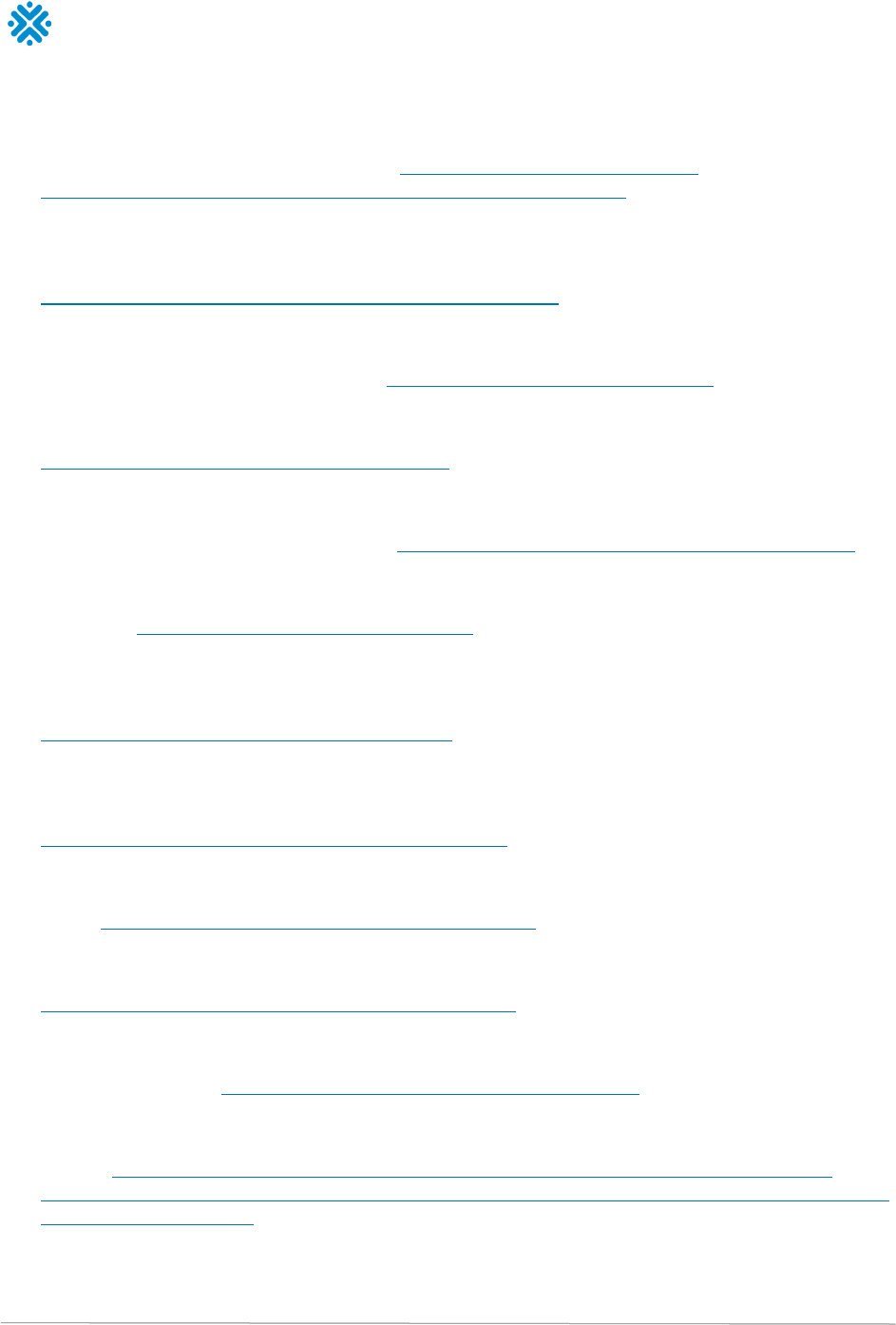
Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 46
Public Health Ontario. (2017b). Alcohol: Awareness of alcohol-related health risks and support for
health and nutrition labels [Infographic].
https://www.publichealthontario.ca/-
/media/Documents/A/2017/alcohol-health-risks-labels.pdf?sc_lang=en .
Rehm, J., Giesbrecht, N., Patra, J., & Roerecke, M. (2006). Estimating chronic disease deaths and
hospitalizations due to alcohol use in Canada in 2002: Implications for policy and prevention
strategies. Preventing Chronic Disease, 3(4), Article A121.
https://www.cdc.gov/pcd/issues/2006/oct/05_0009.htm
Rehm, J., Gmel, G. E., Sr., Gmel, G., Hasan, O. S. M., Imtiaz, S., Popova, S., … Shuper, P. A. (2017)
The relationship between different dimensions of alcohol use and the burden of disease—an
update. Addiction, 112(6), 968–1001. https://doi.org/10.1111/add.13757
Rehm, J., Lachenmeier, D. W., & Room, R. (2014). Why does society accept a higher risk for alcohol
than for other voluntary or involuntary risks? BMC Medicine, 12, Article 189.
https://doi.org/10.1186/s12916-014-0189-z
Roerecke, M., Kaczorowski, J., Tobe, S. W., Gmel, G., Hasan, O., & Rehm, J. (2017). The effect of a
reduction in alcohol consumption on blood pressure: A systematic review and meta-analysis.
Lancet Public health, 2(2), e108–e120. https://doi.org/10.1016/S2468-2667(17)30003-8
Roerecke, M., & Rehm, J. (2010). Irregular heavy drinking occasions and risk of ischemic heart
disease: a systematic review and meta-analysis. American Journal of Epidemiology, 171(6),
633–644. https://doi.org/10.1093/aje/kwp451
Roerecke, M., & Rehm, J. (2014). Alcohol consumption, drinking patterns, and ischemic heart
disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the
impact of heavy drinking occasions on risk for moderate drinkers. BMC Medicine, 12, 182.
https://doi.org/10.1186/s12916-014-0182-6
Roerecke, M., Vafaei, A., Hasan, O. S. M., Chrystoja, B. R., Cruz, M., Lee, R., Neuman, M. G., & Rehm,
J. (2019). Alcohol consumption and risk of liver cirrhosis: A systematic review and meta-Analysis.
American Journal of Gastroenterology, 114(10), 1574–1586.
https://doi.org/10.14309/ajg.0000000000000340
Samokhvalov, A. V., Irving, H. M., & Rehm, J. (2010a). Alcohol consumption as a risk factor for
pneumonia: a systematic review and meta-analysis. Epidemiology and Infection, 138(12), 1789–
1795. https://doi.org/10.1017/S0950268810000774
Samokhvalov, A. V., Irving, H., Mohapatra, S., & Rehm, J. (2010b). Alcohol consumption, unprovoked
seizures, and epilepsy: a systematic review and meta-analysis. Epilepsia, 51(7), 1177–1184.
https://doi.org/10.1111/j.1528-1167.2009.02426.x
Samokhvalov, A. V., Rehm, J., & Roerecke, M. (2015). Alcohol consumption as a risk factor for acute
and chronic pancreatitis: a systematic review and a series of meta-analyses. eBioMedicine,
2(12), 1996–2002. https://doi.org/10.1016/j.ebiom.2015.11.023
Santé publique France & Institut national du cancer. (2017). Avis d’experts relatif à l'évolution du
discours public en matière de consommation d'alcool en France. Saint-Maurice : Santé publique
France. https://www.santepubliquefrance.fr/les-actualites/2017/avis-d-experts-relatif-a-l-
evolution-du-discours-public-en-matiere-de-consommation-d-alcool-en-france-organise-par-sante-
publique-france-et-l-insti
Schoueri-Mychasiw, N., Weerasinghe, A., Stockwell, T., Vallance, K., Hammond, D., Greenfield, T. K.,
McGavock, J., & Hobin, E. (2021). Use as directed: Do standard drink labels on alcohol

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 47
containers help consumers drink (ir)responsibly? Real-world evidence from a quasi-experimental
study in Yukon, Canada. Drug and Alcohol Review, 40(2), 247–257.
https://doi.org/10.1111/dar.13165
Schünemann, H., Brożek, J., Guyatt, G., & Oxman, A. (2013) GRADE handbook for grading quality of
evidence and strength of recommendations.
http://gdt.guidelinedevelopment.org/app/handbook/handbook.html
Shea, B. J., Reeves, B. C., Wells, G., Thuku, M., Hamel, C., Moran, J., … Henry, D. A. (2017).
AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-
randomised studies of healthcare interventions, or both. BMJ, 358.
https://doi.org/10.1136/bmj.j4008
Sherk, A., Thomas, G., Churchill, S., & Stockwell, T. (2020). Does drinking within low-risk guidelines
prevent harm? Implications for high-income countries using the International Model of Alcohol
Harms and Policies. Journal of Studies on Alcohol and Drugs, 81(3), 352–361.
https://doi.org/10.15288/jsad.2020.81.352
Starr, C. (1969). Social benefit versus technological risk: What is our society willing to pay for safety?
Science, 165(3899), 1232–1238. https://doi.org/10.1126/science.165.3899.1232
Statistics Canada. (2021). Table 13-10-0096-11 Heavy drinking, by age group.
https://doi.org/10.25318/1310009601-eng
Stockwell, T., Butt, P., Beirness, D., Gliksman, L., & Paradis, C. (2012). The basis for Canada’s new
low-risk drinking guidelines: A relative risk approach to estimating hazardous levels and patterns
of alcohol use. Drug Alcohol Review, 31(2), 126–134. https://doi.org/10.1111/j.1465-
3362.2011.00342.x
Stockwell, T., Priore, B., Churchill, S., Goulet-Stock, S., Naimi, T., Sherk, A., Shield, K., & Zhao, J.
(2022, May 30 - June 3). Calling time on low-risk drinking guidelines: An evaluation of alternative
methods to communicate risks of alcohol use to consumers. 47th Annual Alcohol Epidemiology
Symposium of the Kettil Bruun Society [KSB 2022], Warsaw, Poland.
Sun, Q., Xie, W., Wang, Y., Chong, F., Song, M., Li, T., Xu, L., & Song, C. (2020). Alcohol consumption
by beverage type and risk of breast cancer: A dose-response meta-analysis of prospective cohort
studies. Alcohol and Alcoholism, 55(3), 246–253. https://doi.org/10.1093/alcalc/agaa012
Sundell, L., Salomaa, V., Vartiainen, E., Poikolainen, K., & Laatikainen, T. (2008). Increased stroke
risk is related to a binge-drinking habit. Stroke, 39(12), 3179–3184.
https://doi.org/10.1161/STROKEAHA.108.520817
Taylor, B., Irving, H. M., Kanteres, F., Room, R., Borges, G., Cherpitel, C., Greenfield, T., & Rehm, J.
(2010). The more you drink, the harder you fall: A systematic review and meta-analysis of how
acute alcohol consumption and injury or collision risk increase together. Drug and Alcohol
Dependence, 110(1-2), 108–116. https://doi.org/10.1016/j.drugalcdep.2010.02.011
Taylor, B., & Rehm, J. (2012). The relationship between alcohol consumption and fatal motor vehicle
injury: high risk at low alcohol levels. Alcoholism, Clinical and Experimental Research, 36(10),
1827–1834. https://doi.org/10.1111/j.1530-0277.2012.01785.x
Thaler, R. H., & Sunstein, C. R. (2008). Nudge: Improving decisions about health, wealth, and
happiness. New Haven, Connecticut: Yale University Press.

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 48
Thomas, G., Poole, N., Greaves, L., Bialystok, L., & Dell, C. (2014, May 26–29). Patterns of alcohol
use among women of childbearing years in Canada: Implications for FASD prevention. Public
Health 2014, Toronto, Ont.
Thomes, P. G., Rasineni, K., Saraswathi, V., Kharbanda, K. K., Clemens, D. L., Sweeney, S. A., …
Casey, C. A. (2021). Natural recovery by the liver and other organs after chronic alcohol use.
Alcohol Research: Current Reviews, 41(1), Article 05. https://doi.org/10.35946/arcr.v41.1.05
Thunderbird Partnership Foundation. (2015). The native wellness assessment. Bothwell, Ont.:
Author. https://thunderbirdpf.org/about-tpf/scope-of-work/native-wellness-assessment/
U.K. Chief Medical Officers. (2016). UK Chief Medical Officers’ Low Risk Drinking Guidelines.
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_dat
a/file/545937/UK_CMOs__report.pdf
Vallance, K., Stockwell, T., Wettlaufer, A., Chow, C., Giesbrecht, N., April, N., … Thompson, K. (2021).
The Canadian Alcohol Policy Evaluation project: Findings from a review of provincial and
territorial alcohol policies. Drug and Alcohol Review, 40(6), 937–945.
https://doi.org/10.1111/dar.13251
Vernooij, R. W. M., Sanabria, A. J., Solà, I., Alonso-Coello, P., & Martínez García, L. (2014). Guidance
for updating clinical practice guidelines: A systematic review of methodological handbooks.
Implementation Science, 9(1), Article 3. https://doi.org/10.1186/1748-5908-9-3
Verrill, C., Markham, H., Templeton, A., Carr, N. J., & Sheron, N. (2009). Alcohol-related cirrhosis—
early abstinence is a key factor in prognosis, even in the most severe cases. Addiction, 104(5),
768–774. https://doi.org/10.1111/j.1360-0443.2009.02521.x
Vieira, A. R., Abar, L., Chan, D., Vingeliene, S., Polemiti, E., Stevens, C., Greenwood, D., & Norat, T.
(2017). Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis
of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project.
Annals of Oncology, 28(8), 1788–1802. https://doi.org/10.1093/annonc/mdx171
Vinson, D. C., Maclure, M., Reidinger, C., & Smith, G. S. (2003). A population-based case-crossover
and case-control study of alcohol and the risk of injury. Journal of Studies on Alcohol, 64(3),
358–366. https://doi.org/10.15288/jsa.2003.64.358
Voas, R. B., Torres, P., Romano, E., & Lacey, J. H. (2012). Alcohol-related risk of driver fatalities: An
update using 2007 data. Journal of Studies on Alcohol and Drugs, 73(3), 341–350.
https://doi.org/10.15288/jsad.2012.73.341
Voskoboinik, A., Kalman, J. M., De Silva, A., Nicholls, T., Costello, B., Nanayakkara, S., … Kistler, P. M.
(2020). Alcohol abstinence in drinkers with atrial fibrillation. New England Journal of Medicine,
382(1), 20–28. https://doi.org/10.1056/NEJMoa1817591
Wagenaar, A. C., Salois, M. J., & Komro, K. A. (2009). Effects of beverage alcohol price and tax levels
on drinking: a meta-analysis of 1003 estimates from 112 studies. Addiction, 104(2), 179–190.
https://doi.org/10.1111/j.1360-0443.2008.02438.x
Wagenaar, A. C., Tobler, A. L., & Komro, K. A. (2010). Effects of alcohol tax and price policies on
morbidity and mortality: a systematic review. American Journal of Public Health 100, 2270–
2278. https://doi.org/10.2105/AJPH.2009.186007
Wakefield, M. A., Brennan, E., Dunstone, K., Durkin, S. J., Dixon, H. G., Pettigrew, S., & Slater, M. D.
(2018). Immediate effects on adult drinkers of exposure to alcohol harm reduction
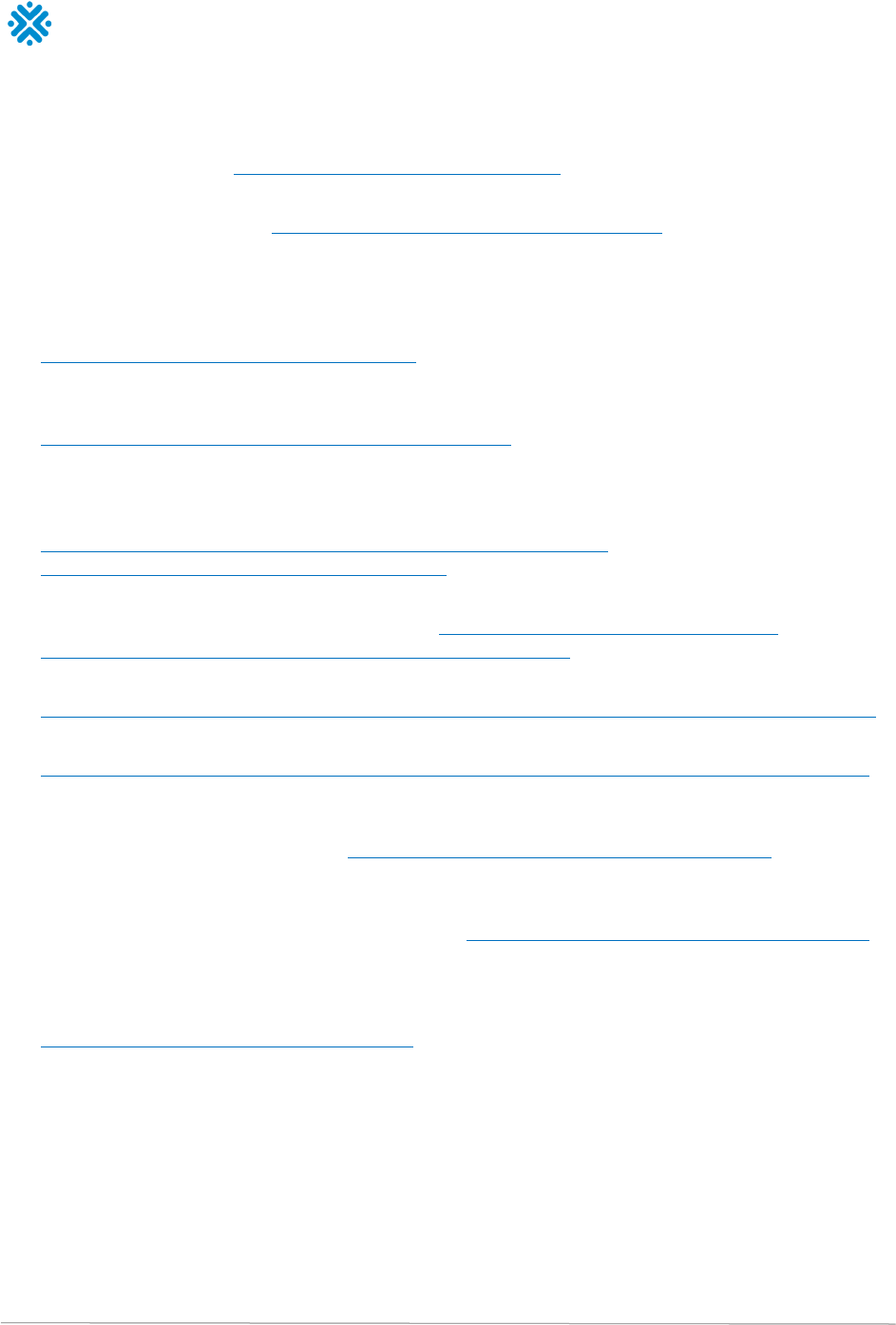
Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 49
advertisements with and without drinking guideline messages: experimental study. Addiction,
113(6), 1019–1029. https://doi.org/10.1111/add.14147
Wechsler, H., & Austin, S. B. (1998). Binge drinking: the five/four measure. Journal of Studies on
Alcohol, 59(1), 122–124. https://doi.org/10.15288/jsa.1998.59.122
Weerasinghe, A., Schoueri-Mychasiw, N., Vallance, K., Stockwell, T., Hammond, D., McGavock, J., …
Hobin, E. (2020). Improving knowledge that alcohol can cause cancer is associated with
consumer support for alcohol policies: Findings from a real-world alcohol labelling study.
International Journal of Environmental Research and Public Health, 17(2), Article 398.
https://doi.org/10.3390/ijerph17020398
Wettlaufer, A. (2018). Can a label help me drink in moderation? A review of the evidence on
standard drink labelling. Substance Use & Misuse, 53(4), 585–595.
https://doi.org/10.1080/10826084.2017.1349798
Whiting, P., Davies, P., Savović, J., Caldwell, D., & Churchill, R. (2013) Evidence to inform the
development of ROBIS, a new tool to assess the risk of bias in systematic reviews. Bristol, United
Kingdom: School of Social and Community Medicine, University of Bristol.
https://www.bristol.ac.uk/media-library/sites/social-community-
medicine/robis/ROBIS%20Report%204_9.pdf
World Cancer Research Fund International. (2018). Diet, nutrition, physical activity and cancer: a
global perspective. London, England: Author. https://www.wcrf.org/diet-activity-and-
cancer/global-cancer-update-programme/table-of-contents/
World Health Organization. (n.d.). Alcohol control policies.
https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/alcohol-control-policies
World Health Organization. (2021). Global information system on alcohol and health.
https://www.who.int/data/gho/data/themes/global-information-system-on-alcohol-and-health
Wu, X., Liu, X., Liao, W., Kang, N., Dong, X., Abdulai, T., … Li, Y. (2021). Prevalence and
characteristics of alcohol consumption and risk of type 2 diabetes mellitus in rural China. BMC
Public Health, 21(1), Article 1644. https://doi.org/10.1186/s12889-021-11681-0
Zhao, J., Stockwell, T., Roemer, A., Naimi, T., & Chikritzhs, T. (2017). Alcohol consumption and
mortality from coronary heart disease: An updated meta-analysis of cohort studies. Journal of
Studies on Alcohol and Drugs, 78(3), 375–386. https://doi.org/10.15288/jsad.2017.78.375
Zhao, J., Stockwell, T., & Thomas, G. (2015). An adaptation of the Yesterday Method to correct for
under-reporting of alcohol consumption and estimate compliance with Canadian low-risk drinking
guidelines. Canadian Journal of Public Health, 106(4), e204–e209.
https://doi.org/10.17269/cjph.106.4753

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 50
Appendix 1
Lifetime Risk of Alcohol-Attributable Death and Disability:
Shadow Analysis
Purpose
To inform decisions regarding the formation of Canadian drinking guidelines, a primary analysis was
performed whose results were a collection of risk relationships that estimated the risk of death and
disability as a function of average daily alcohol use by those who live in Canada.
Toward ensuring accuracy of the primary analysis, this shadow analysis process was designed and
undertaken. The general objective of a shadow analysis is for the main and shadow analysts to come
together and share the desired project input and broad methodology. The two analyses are
conducted independently, in parallel, and results are compared to ensure accuracy of the primary
collection of results.
Method
The primary and shadow researchers met several times to discuss strategy and determine raw input
that would be shared by both analyses. Shared inputs were as follows:
• Relative risk function definitions: Each alcohol-attributable condition considered was assigned a
dose–response relative risk function, and the source and definition of these risk functions was
shared. Relative risk functions were prepared by the primary researcher.
• Prevalence and consumption data: Raw survey data for Canada was transformed into total and
relative population alcohol consumption, where relevant population strata were sex and age.
Prevalence and consumption data were prepared by the primary researcher.
• Deaths, years lived with disability, and incidence in the population, by condition: Raw data were
aggregated and summarized into alcohol-attributable condition categories for each outcome
category. Death data was prepared by the primary researcher and also the shadow researcher.
Years lived with disability and incidence were prepared by the primary researcher.
The two analysts discussed the broad methodologies. The implementation of the lifetime risk
methodology was then performed in R in both the primary and shadow analyses. Researchers wrote
their scripts and/or packages independently. Primary and shadow analysis results were compared
with an eye toward whether differences would have an impact on the quantitative guidelines
endeavour.
Summary of the Comparison of Findings
The shadow analysis is a very near-match with the primary analysis, with differences accounted for
by expected, random differentials in the model-building exercise, the random draws employed
throughout the process and slight differences in methodological choices between analysts. Small
differences between the shadow analyses and the primary analysis are not expected to lead to
differences in interpretations of results for the quantitative guidelines endeavour.
Figures 1 and 2 compares the results of the primary and shadow analyses. Figure 1 displays lifetime
deaths per 1,000 people at each level of consumption up to an average of 100 g ethanol/day.
Figure 2 displays the same statistic on the range of up to an average of 40 g ethanol/day. In each

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 51
figure, the results of the primary analysis (and associated 95% confidence intervals [CIs]) are shown
in red and the shadow analyses in blue. In Figure 2, it is clear that the shadow analysis produced
results that would not lead to substantive differences in interpretation when designing alcohol use
guidelines for people who live in Canada. A high similarity between the shadow and primary analysis
is observed for all levels of average daily alcohol use, and in particular the match is near-perfect at
levels of average daily alcohol use below 50 g ethanol/ day. This behaviour is consistent throughout
the remainder of the shadow results, distributed separately.
Figure 1: Visual comparison between primary results and shadow results in the category of male death, range of
average consumption of from 1 to 100 g ethanol/day
-100
-50
0
50
100
150
200
250
300
350
400
0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90 95 100
Lifetime deaths
per 1000 people
Average alcohol intake (grams /day)
Shadow analysis - Male Deaths
Shadow PE Shadow 95% CI Primary PE Primary 95% CI

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 52
Figure 2: Visual comparison between primary results and shadow results in the category of male death, range of
average consumption of from 1 to 40 g ethanol/day
-60
-40
-20
0
20
40
60
80
100
120
0 5 10 15 20 25 30 35 40
Lifetime deaths
per 1000 people
Average alcohol intake (grams /day)
Shadow analysis - Male Deaths
Shadow PE Shadow 95% CI Primary PE Primary 95% CI
Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 53
Appendix 2
Table 1. Increased risk of diseases and injuries, with 95% confidence intervals, for females, based on average daily alcohol use
Sex / condition or
injury
Alcohol intake (g/day)
5
10
15
20
25
30
35
40
45
50
Tuberculosis
1.09
(1.02, 1.17)
1.20
(1.03, 1.38)
1.31
(1.05, 1.62)
1.43
(1.07, 1.90)
1.57
(1.09, 2.23)
1.71
(1.11, 2.62)
1.88
(1.12, 3.08)
2.05
(1.14, 3.61)
2.24
(1.16, 4.24)
2.46
(1.18, 4.98)
Lower respiratory
infections
1.02
(1.00, 1.04)
1.05
(1.01, 1.09)
1.07
(1.01, 1.13)
1.10
(1.02, 1.18)
1.13
(1.02, 1.23)
1.15
(1.03, 1.28)
1.18
(1.04, 1.33)
1.21
(1.04, 1.39)
1.24
(1.05, 1.45)
1.27
(1.05, 1.51)
Oral cavity and
pharynx cancer
1.13
(1.11, 1.15)
1.28
(1.23, 1.31)
1.44
(1.36, 1.50)
1.61
(1.51, 1.71)
1.81
(1.67, 1.94)
2.03
(1.84, 2.20)
2.26
(2.03, 2.49)
2.52
(2.24, 2.80)
2.81
(2.46, 3.15)
3.12
(2.70, 3.54)
Esophagus cancer
1.07
(1.06, 1.07)
1.14
(1.13, 1.15)
1.22
(1.21, 1.23)
1.30
(1.28, 1.32)
1.39
(1.37, 1.41)
1.48
(1.45, 1.52)
1.58
(1.55, 1.62)
1.69
(1.64, 1.74)
1.80
(1.75, 1.86)
1.93
(1.86, 1.99)
Colorectal cancer
1.03
(1.02, 1.04)
1.07
(1.05, 1.09)
1.11
(1.07, 1.14)
1.14
(1.10, 1.19)
1.18
(1.13, 1.24)
1.23
(1.15, 1.30)
1.27
(1.18, 1.36)
1.31
(1.21, 1.42)
1.36
(1.24, 1.48)
1.40
(1.27, 1.54)
Liver cancer
1.02
(1.01, 1.03)
1.04
(1.02, 1.06)
1.06
(1.03, 1.09)
1.08
(1.04, 1.12)
1.10
(1.05, 1.16)
1.12
(1.06, 1.19)
1.15
(1.07, 1.23)
1.17
(1.08, 1.26)
1.19
(1.09, 1.30)
1.22
(1.10, 1.34)
Breast cancer
1.05
(1.04, 1.06)
1.10
(1.07, 1.12)
1.15
(1.11, 1.19)
1.20
(1.15, 1.25)
1.26
(1.19, 1.33)
1.31
(1.23, 1.40)
1.38
(1.28, 1.49)
1.44
(1.32, 1.57)
1.51
(1.37, 1.66)
1.58
(1.42, 1.76)
Larynx cancer
1.08
(1.06, 1.09)
1.16
(1.11, 1.19)
1.24
(1.18, 1.30)
1.33
(1.24, 1.42)
1.42
(1.31, 1.54)
1.52
(1.38, 1.67)
1.63
(1.46, 1.80)
1.74
(1.54, 1.95)
1.85
(1.62, 2.11)
1.98
(1.70, 2.28)
Pancreatitis
0.87
(0.78, 0.98)
0.77
(0.62, 0.97)
0.72
(0.53, 0.99)
0.72
(0.50, 1.05)
0.76
(0.51, 1.15)
0.85
(0.55, 1.31)
0.98
(0.62, 1.56)
1.15
(0.69, 1.94)
1.35
(0.75, 2.45)
1.58
(0.82, 3.17)
Diabetes Mellitus
0.78
(0.72, 0.85)
0.73
(0.65, 0.82)
0.70
(0.61, 0.80)
0.68
(0.59, 0.79)
0.67
(0.57, 0.79)
0.66
(0.55, 0.78)
0.66
(0.54, 0.79)
0.65
(0.53, 0.80)
0.65
(0.53, 0.81)
0.66
(0.52, 0.81)
Liver cirrhosis
2.09
(1.89, 2.31)
2.82
(2.44, 3.24)
3.55
(2.98, 4.20)
4.31
(3.52, 5.23)
5.11
(4.07, 6.35)
5.97
(4.65, 7.56)
6.88
(5.26, 8.88)
7.85
(5.90, 10.32)
8.90
(6.56, 11.89)
10.01
(7.27, 13.58)
Atrial fibrillation and
flutter
1.03
(1.02, 1.04)
1.07
(1.05, 1.08)
1.10
(1.08, 1.13)
1.14
(1.10, 1.17)
1.17
(1.13, 1.22)
1.21
(1.16, 1.27)
1.25
(1.19, 1.32)
1.29
(1.22, 1.38)
1.33
(1.25, 1.43)
1.38
(1.28, 1.49)
Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 54
Sex / condition or
injury
Alcohol intake (g/day)
5
10
15
20
25
30
35
40
45
50
Hypertension
1.03
(1.00, 1.05)
1.06
(1.01, 1.11)
1.09
(1.03, 1.15)
1.12
(1.05, 1.19)
1.15
(1.06, 1.24)
1.18
(1.07, 1.30)
1.21
(1.10, 1.34)
1.25
(1.12, 1.39)
1.28
(1.14, 1.43)
1.32
(1.16, 1.50)
Ischemic heart
disease
0.95
(0.76, 1.19)
0.95
(0.76, 1.19)
0.95
(0.76, 1.19)
0.95
(0.76, 1.19)
1.04
(0.80, 1.35)
1.04
(0.80, 1.35)
1.04
(0.80, 1.35)
1.04
(0.80, 1.35)
1.07
(0.83, 1.37)
1.07
(0.83, 1.37)
Ischemic stroke
0.90
(0.85, 0.95)
0.90
(0.85, 0.95)
0.92
(0.87, 0.97)
0.92
(0.87, 0.97)
1.08
(1.01, 1.16)
1.08
(1.01, 1.16)
1.08
(1.01, 1.16)
1.08
(1.01, 1.16)
1.08
(1.01, 1.16)
1.14
(1.01, 1.28)
Intracerebral
hemorrhage
0.92
(0.77, 1.10)
0.92
(0.77, 1.10)
0.99
(0.83, 1.19)
0.99
(0.83, 1.19)
1.25
(0.92, 1.69)
1.25
(0.92, 1.69)
1.25
(0.92, 1.69)
1.25
(0.92, 1.69)
1.25
(0.92, 1.69)
1.67
(1.26, 2.25)
Subarachnoid
hemorrhage
1.21
(0.48, 3.06)
1.21
(0.48, 3.06)
1.11
(0.33, 3.90)
1.11
(0.33, 3.90)
1.39
(0.32, 5.94)
1.39
(0.32, 5.94)
1.39
(0.32, 5.94)
1.39
(0.32, 5.94)
1.39
(0.32, 5.94)
1.82
(0.38, 10.12)
Epilepsy
1.07
(1.05, 1.09)
1.14
(1.10, 1.17)
1.21
(1.16, 1.26)
1.29
(1.21, 1.36)
1.37
(1.27, 1.47)
1.45
(1.33, 1.58)
1.55
(1.40, 1.71)
1.64
(1.46, 1.84)
1.75
(1.54, 1.98)
1.86
(1.61, 2.14)
Road injuries
1.05
(1.02, 1.08)
1.10
(1.04, 1.16)
1.15
(1.07, 1.25)
1.21
(1.09, 1.35)
1.27
(1.11, 1.45)
1.33
(1.14, 1.57)
1.40
(1.16, 1.69)
1.47
(1.19, 1.82)
1.54
(1.22, 1.96)
1.62
(1.24, 2.11)
Other unintentional
injuries
1.04
(1.03, 1.05)
1.08
(1.06, 1.10)
1.12
(1.09, 1.16)
1.17
(1.12, 1.22)
1.21
(1.15, 1.28)
1.26
(1.18, 1.35)
1.31
(1.21, 1.42)
1.36
(1.25, 1.49)
1.42
(1.28, 1.56)
1.47
(1.32, 1.64)
Intentional injuries
1.13
(1.10, 1.16)
1.28
(1.21, 1.36)
1.45
(1.34, 1.58)
1.65
(1.47, 1.84)
1.87
(1.62, 2.15)
2.11
(1.79, 2.50)
2.39
(1.97, 2.91)
2.71
(2.17, 3.39)
3.07
(2.39, 3.95)
3.48
(2.63, 4.60)

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 55
Table 2. Increased risk of diseases and injuries, with 95% confidence intervals, for males, based on average daily alcohol use
Sex / condition or
injury
Alcohol intake (g/day)
5
10
15
20
25
30
35
40
45
50
Tuberculosis
1.09
(1.02, 1.18)
1.20
(1.04, 1.38)
1.31
(1.06, 1.63)
1.43
(1.08, 1.91)
1.57
(1.10, 2.25)
1.71
(1.12, 2.64)
1.88
(1.15, 3.11)
2.05
(1.17, 3.66)
2.24
(1.19, 4.30)
2.46
(1.21, 5.05)
Lower respiratory
infections
1.02
(1.01, 1.05)
1.05
(1.01, 1.09)
1.07
(1.02, 1.14)
1.10
(1.02, 1.19)
1.13
(1.03, 1.25)
1.15
(1.03, 1.30)
1.18
(1.04, 1.36)
1.21
(1.04, 1.42)
1.24
(1.05, 1.48)
1.27
(1.05, 1.55)
Oral cavity and
pharynx cancer
1.13
(1.11, 1.15)
1.28
(1.24, 1.32)
1.44
(1.37, 1.51)
1.61
(1.52, 1.72)
1.81
(1.68, 1.95)
2.03
(1.86, 2.22)
2.26
(2.05, 2.51)
2.52
(2.25, 2.83)
2.81
(2.48, 3.18)
3.12
(2.73, 3.58)
Esophagus cancer
1.07
(1.06, 1.07)
1.14
(1.13, 1.15)
1.22
(1.21, 1.23)
1.30
(1.28, 1.32)
1.39
(1.36, 1.42)
1.48
(1.45, 1.52)
1.58
(1.54, 1.63)
1.69
(1.64, 1.74)
1.80
(1.75, 1.87)
1.93
(1.86, 2.00)
Colorectal cancer
1.03
(1.03, 1.04)
1.07
(1.05, 1.09)
1.11
(1.08, 1.14)
1.14
(1.11, 1.19)
1.18
(1.13, 1.24)
1.23
(1.16, 1.30)
1.27
(1.19, 1.35)
1.31
(1.22, 1.41)
1.36
(1.25, 1.48)
1.40
(1.29, 1.54)
Liver cancer
1.02
(1.01, 1.03)
1.04
(1.02, 1.06)
1.06
(1.03, 1.09)
1.08
(1.04, 1.12)
1.10
(1.05, 1.16)
1.12
(1.06, 1.19)
1.15
(1.07, 1.23)
1.17
(1.08, 1.26)
1.19
(1.09, 1.30)
1.22
(1.11, 1.34)
Breast cancer
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
1.00
(1.00, 1.00)
Larynx cancer
1.08
(1.06, 1.09)
1.16
(1.11, 1.20)
1.24
(1.18, 1.30)
1.33
(1.24, 1.42)
1.42
(1.31, 1.54)
1.52
(1.38, 1.67)
1.63
(1.45, 1.82)
1.74
(1.53, 1.97)
1.85
(1.62, 2.13)
1.98
(1.70, 2.29)
Pancreatitis
1.09
(1.05, 1.13)
1.19
(1.10, 1.28)
1.30
(1.16, 1.44)
1.41
(1.21, 1.63)
1.54
(1.27, 1.85)
1.68
(1.34, 2.09)
1.84
(1.40, 2.36)
2.00
(1.47, 2.67)
2.18
(1.54, 3.02)
2.38
(1.62, 3.41)
Diabetes Mellitus
1.00
(1.00, 1.00)
1.00
(1.00, 1.01)
1.00
(0.99, 1.02)
1.01
(0.98, 1.03)
1.01
(0.98, 1.05)
1.01
(0.97, 1.06)
1.02
(0.97, 1.08)
1.02
(0.97, 1.09)
1.03
(0.97, 1.10)
1.04
(0.97, 1.11)
Liver cirrhosis
1.16
(1.13, 1.18)
1.33
(1.28, 1.38)
1.53
(1.45, 1.62)
1.76
(1.63, 1.90)
2.02
(1.84, 2.22)
2.32
(2.08, 2.60)
2.67
(2.35, 3.05)
3.07
(2.66, 3.57)
3.53
(3.00, 4.19)
4.06
(3.39, 4.91)
Atrial fibrillation and
flutter
1.03
(1.02, 1.04)
1.07
(1.05, 1.08)
1.10
(1.08, 1.13)
1.14
(1.10, 1.17)
1.17
(1.13, 1.22)
1.21
(1.16, 1.27)
1.25
(1.19, 1.32)
1.29
(1.21, 1.37)
1.33
(1.24, 1.42)
1.38
(1.27, 1.48)

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 56
Sex / condition or
injury
Alcohol intake (g/day)
5
10
15
20
25
30
35
40
45
50
Hypertension
1.07
(1.04, 1.10)
1.15
(1.09, 1.22)
1.19
(1.13, 1.26)
1.23
(1.16, 1.32)
1.28
(1.20, 1.37)
1.32
(1.23, 1.43)
1.34
(1.25, 1.46)
1.36
(1.27, 1.48)
1.38
(1.28, 1.50)
1.40
(1.30, 1.53)
Ischemic heart
disease
0.95
(0.76, 1.20)
0.95
(0.76, 1.20)
0.95
(0.76, 1.20)
0.95
(0.76, 1.20)
1.04
(0.81, 1.36)
1.04
(0.81, 1.36)
1.04
(0.81, 1.36)
1.04
(0.81, 1.36)
1.07
(0.82, 1.41)
1.07
(0.82, 1.41)
Ischemic stroke
0.92
(0.87, 0.97)
0.92
(0.87, 0.97)
0.92
(0.87, 0.97)
0.92
(0.87, 0.97)
1.08
(1.02, 1.15)
1.08
(1.02, 1.15)
1.08
(1.02, 1.15)
1.08
(1.02, 1.15)
1.08
(1.02, 1.15)
1.14
(1.01, 1.27)
Intracerebral
hemorrhage
0.92
(0.78, 1.11)
0.92
(0.78, 1.11)
0.99
(0.82, 1.19)
0.99
(0.82, 1.19)
1.25
(0.93, 1.68)
1.25
(0.93, 1.68)
1.25
(0.93, 1.68)
1.25
(0.93, 1.68)
1.25
(0.93, 1.68)
1.67
(1.24, 2.22)
Subarachnoid
hemorrhage
1.21
(0.51, 2.81)
1.21
(0.51, 2.81)
1.11
(0.32, 4.00)
1.11
(0.32, 4.00)
1.39
(0.25, 6.42)
1.39
(0.25, 6.42)
1.39
(0.25, 6.42)
1.39
(0.25, 6.42)
1.39
(0.25, 6.42)
1.82
(0.32, 10.36)
Epilepsy
1.07
(1.06, 1.09)
1.14
(1.11, 1.17)
1.21
(1.16, 1.26)
1.29
(1.22, 1.36)
1.37
(1.28, 1.47)
1.45
(1.35, 1.59)
1.55
(1.41, 1.71)
1.64
(1.48, 1.85)
1.75
(1.56, 1.99)
1.86
(1.64, 2.15)
Road injuries
1.08
(1.06, 1.09)
1.16
(1.12, 1.20)
1.25
(1.19, 1.31)
1.34
(1.26, 1.43)
1.44
(1.34, 1.56)
1.56
(1.42, 1.71)
1.67
(1.50, 1.87)
1.80
(1.60, 2.04)
1.94
(1.69, 2.23)
2.09
(1.79, 2.44)
Other unintentional
injuries
1.04
(1.03, 1.05)
1.08
(1.06, 1.10)
1.12
(1.09, 1.16)
1.17
(1.12, 1.22)
1.21
(1.15, 1.28)
1.26
(1.18, 1.35)
1.31
(1.22, 1.42)
1.36
(1.25, 1.49)
1.42
(1.28, 1.56)
1.47
(1.32, 1.64)
Intentional injuries
1.13
(1.10, 1.16)
1.28
(1.21, 1.36)
1.45
(1.33, 1.58)
1.65
(1.47, 1.84)
1.87
(1.62, 2.14)
2.11
(1.78, 2.49)
2.39
(1.96, 2.90)
2.71
(2.16, 3.38)
3.07
(2.38, 3.93)
3.48
(2.62, 4.58)

Update of Canada’s Low-Risk Alcohol Drinking Guidelines: Final Report for Public Consultation
Canadian Centre on Substance Use and Addiction • Centre canadien sur les dépendances et l’usage de substances Page 57
Appendix 3
Specific messages for girls and women to supplement the Guidance on Alcohol and Health
It is important for girls and women to know:
• There are risks of alcohol use for both men and women, but it is not a level playing field, as
alcohol affects women ’s bodies more negatively
• Alcohol is processed by women’s bodies differently, causing more negative health effects, earlier,
after lesser amounts of alcohol
• Women become intoxicated faster after drinking less than men due to smaller bodies and
organs, less body water, hormonal effects, and different enzyme actions that break down alcohol
• Alcohol has more serious health effects on females than males, due to body size, body fat/water
ratio, hormonal effects and differing actions of enzymes that break down alcohol
• Alcohol consumption increases risk of breast cancer, a very common cancer in Canadian women
• Women experience more liver injuries on lower levels of alcohol, compared to men
It is important for girls and women to know:
• Perpetrators of sexual assault often target someone who has been drinking alcohol or is
intoxicatedWomen often use alcohol to cope with the stress of trauma, IPV and caregiving, which
can lead to poorer, not better health
• Girls and women with histories of childhood abuse progress more quickly from starting to drink to
becoming alcohol dependent
And some ideas for the pregnancy-related messages:
• Alcohol use in pregnancy negatively affects both women’s and fetal health
• There is no safe level of alcohol use in pregnancy, so it is safest not to drink at all while pregnant
• The more alcohol consumed, the greater the risk of harm for women’s and fetal health
• Alcohol use in pregnancy especially when combined with poor nutrition and tobacco use can
result in infant death, birth defects, and lifelong behavioural and cognitive problems
• Alcohol use in pregnancy can increase the risk of miscarriage.

