
Page 1 of 44
Medicare & Mental Health Coverage
MLN1986542 July 2024
CPT codes, descriptions, and other data only are copyright 2023 American Medical Association. All Rights Reserved.
Applicable FARS/HHSARS apply. Fee schedules, relative value units, conversion factors and/or related components are not
assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly
practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.

Medicare & Mental Health Coverage MLN Booklet
Page 2 of 44 MLN1986542 July 2024
Table of Contents
What’s Changed? ................................................................................................................................ 4
Medicare-Covered Services................................................................................................................ 5
Non-Covered Services
........................................................................................................................ 9
Prescription Drug Coverage ............................................................................................................... 9
Medicare Advantage Organizations ................................................................................................... 9
Eligible Professionals ....................................................................................................................... 10
Provider Information ..........................................................................................................................11
Physician ......................................................................................................................................... 11
Clinical Psychologist (CP) .............................................................................................................. 12
Clinical Social Worker (CSW) ........................................................................................................ 13
Clinical Nurse Specialist (CNS)...................................................................................................... 14
Nurse Practitioner (NP)
.................................................................................................................. 15
Physician Assistant (PA) ................................................................................................................ 16
Certied Nurse-Midwife (CNM) ...................................................................................................... 18
Independently Practicing Psychologist (IPP) ................................................................................. 19
Certied Registered Nurse Anesthetist (CRNA)............................................................................. 20
Marriage & Family Therapist (MFT)
............................................................................................... 21
Mental Health Counselor (MHC) .................................................................................................... 22
Incident to Provision ......................................................................................................................... 23
Commonly Used CPT Codes ............................................................................................................ 24
National Correct Coding Initiative .................................................................................................... 29

Medicare & Mental Health Coverage MLN Booklet
Page 3 of 44 MLN1986542 July 2024
Outpatient Psychiatric Hospital Services ....................................................................................... 29
Telehealth ....................................................................................................................................... 30
Partial Hospitalization Program (PHP) ........................................................................................... 32
Intensive Outpatient Program (IOP) ............................................................................................... 33
Community Mental Health Centers ................................................................................................ 34
Behavioral Health Integration (BHI) Services................................................................................. 34
Medical Records Checklist: Outpatient Psychiatric Services
....................................................... 35
Acute Care Hospital .......................................................................................................................... 38
Inpatient Psychiatric Facility Services ............................................................................................ 38
Medical Records Requirements ..................................................................................................... 38
Medical Records Checklist: Inpatient Psychiatric Services .......................................................... 39
Coverage Period ............................................................................................................................ 43
Same Day Billing Guidelines ............................................................................................................ 43
Resources .......................................................................................................................................... 44

Medicare & Mental Health Coverage MLN Booklet
Page 4 of 44 MLN1986542 July 2024
What’s Changed?
●
Added billing and payment information about marriage and family therapist and mental health
counselor services (pages 21–22)
●
Added more commonly used mental health-related codes (pages 25–28)
●
Added more information about intensive outpatient program services (pages 33–34)
Substantive content changes are in dark red.

Medicare & Mental Health Coverage MLN Booklet
Page 5 of 44 MLN1986542 July 2024
Medicare-covered behavioral health services, typically known as mental health and substance use
services, can aect a patient’s overall well-being. It’s important to understand Medicare’s covered
services and who can provide them.
Anyone experiencing a mental health crisis, including substance use crisis or thoughts of suicide,
can get condential support 24/7 by calling 988 or visiting 988lifeline.org. Visit the Substance
Abuse and Mental Health Administration 988 Partner Toolkit for information and resources.
Medicare-Covered Services
We may cover these behavioral health and wellness services:
●
Alcohol misuse screening and counseling for adults who use alcohol but aren’t dependent; if you
detect misuse, we cover up to 4 brief, face-to-face counseling sessions per year if the patient is
competent and alert during counseling
●
Alcohol treatment, detoxication, outpatient hospital treatment, and rehabilitative services,
including inpatient hospital stays
●
Annual wellness visit (AWV) to develop or update a personalized prevention plan, including health
risk assessment and depression screening
●
If you detect cognitive impairment at an AWV or other routine visit, you may perform a more
detailed cognitive assessment and develop a care plan during a separate visit
●
As of 2024, we cover a Social Determinants of Health (SDOH) risk assessment at no cost to
the patient when it’s provided as an optional AWV element (as part of the same visit with the
same date of service as the AWV)
●
The AWV can be a community health integration (CHI) or principal illness navigation (PIN)
initiating visit when the practitioner identies an unmet SDOH need that prevents the patient
from carrying out the recommended personalized prevention plan
●
Advance care planning (ACP) to discuss a patient’s health care wishes if they can’t make decisions
about their care, as part of the AWV or a separate Part B service, including an advance directive
●
Behavioral health integration (BHI) by clinical sta to assess, monitor, and plan care
●
Biofeedback therapy, where patients learn non-drug treatments to control bodily responses, like
heart rate and muscle tension

Medicare & Mental Health Coverage MLN Booklet
Page 6 of 44 MLN1986542 July 2024
●
Bundled substance use disorder (SUD) payments (see HCPCS G2086, G2087, and G2088 billing
codes) for:
●
SUD management and counseling
●
SUD services provided in an oce setting, including:
▪
Overall management
▪
Care coordination
▪
Individual and group psychotherapy
▪
Substance use counseling
Opioid Treatment Programs
We now pay certied Opioid Treatment Programs (OTPs) through bundled opioid use disorder
(OUD) Medicare Part B treatment services payments. Covered services include FDA-approved
opioid agonist and antagonist medication (including methadone, buprenorphine, and naltrexone)
and their administration (if applicable), substance use counseling, individual and group therapy,
toxicology testing, intake activities, periodic assessments, take-home supplies of naloxone, and
intensive outpatient program services.
Opioid Treatment Program Directory and OTPs Billing & Payment have more information.
●
Caregiver-focused behavioral health risk assessment of their own behavior and health risks, which
benets the patient
●
Caregiver training services when a physician, non-physician practitioner (NPP), or therapist
provides them as part of the patient’s individualized treatment plan or therapy plan of care
●
Chemical and electrical aversion therapy to condition a person to avoid undesirable behavior by
pairing the behavior with unwanted stimuli
●
CHI services to help patients who have unmet social needs that aect the diagnosis and treatment
of their medical problems identify and connect with appropriate clinical and social support resources
●
Practitioners may provide CHI services monthly, as medically necessary, following an initiating
Evaluation and Management (E/M) visit (CHI initiating visit) where the practitioner identies
the presence of SDOH needs that signicantly limit their ability to diagnose or treat the patient
problems addressed in the visit
●
Community health workers, care navigators, peer support specialists, and other auxiliary
personnel may be employed by community-based organizations (CBOs) if the billing practitioner
provides the required supervision for these services, similar to other care management services
●
Cognitive assessment and care planning, a comprehensive evaluation of a new or existing patient
who exhibits cognitive impairment signs and symptoms, required to establish or conrm a diagnosis,
etiology, and condition severity

Medicare & Mental Health Coverage MLN Booklet
Page 7 of 44 MLN1986542 July 2024
●
Chronic care management (CCM) and complex CCM for patients with multiple chronic conditions
placing them at high risk
●
Chronic pain management (CPM) for patients with chronic pain
●
Depression screening, up to 15 minutes annually, when sta-assisted depression care supports
can assure accurate diagnosis, eective treatment, and follow-up; screening by clinical sta in a
primary care setting who can advise the physician of results and coordinate treatment referrals
●
Diagnostic psychological and neuropsychological tests
●
Drug therapy or pharmacological management using medications to treat a disease
●
Drug withdrawal treatment to monitor signs and symptoms after changes in regular drug dose
●
Electroconvulsive therapy (ECT), which involves passing small electric currents through the brain,
intentionally triggering a seizure, to treat depression and other mental illness
●
Family psychotherapy with or without the patient present, as medically reasonable and necessary,
with patient treatment as the primary purpose
●
Health and behavioral assessment and intervention that identies or treats psychological, behavioral,
emotional, cognitive, and social factors important to prevent, treat, or manage physical health issues
●
Hypnotherapy
●
Individual and group psychotherapy; individual therapy with 1 or more therapists or more than 1
person in a therapy session with 1 or more therapists
●
Individual activity therapy that’s part of a partial hospitalization program (PHP), which may be cognitive,
physical, social, and spiritual but not recreational or diversionary
●
PHP, a structured, intensive, outpatient psychiatric services program, is an alternative to inpatient
psychiatric care provided during the day (doesn’t require an overnight stay) through a hospital
outpatient department or community mental health center (CMHC)
●
Initial preventive physical exam (IPPE) to review medical and social health history and provide
preventive services education, counseling, and referral, as appropriate
●
Intensive outpatient program (IOP) services
●
Interactive psychotherapy
●
Interactive telecommunications, including 2-way, interactive audio-only technology, to diagnose,
evaluate, or treat certain mental health or SUDs using telehealth services if the patient is in their home
●
Hospital clinical sta must have the capability to provide 2-way, interactive, audio-video technology
services but may use audio-only technology given an individual patient’s technological limitations,
abilities, or preferences
●
You can provide telehealth using 2-way, interactive, audio-only technology through
December 31, 2024
●
Telehealth services provided to people in their homes will be paid at the non-facility Medicare
Physician Fee Schedule (PFS) rate through December 31, 2024
●
Marriage and family therapist (MFT) services (also available through an acceptable telehealth
mental health disorder service site)

Medicare & Mental Health Coverage MLN Booklet
Page 8 of 44 MLN1986542 July 2024
●
Medication for Opioid Use Disorder (MOUD) management when a patient agrees to a medication
trial period treatment option and its eectiveness is monitored
●
Medication-Assisted Treatment (MAT), which uses medications with counseling and behavioral
therapy to treat SUDs, including OUDs; when a certied opioid treatment program (OTP) provider
treats OUDs, we pay for certain medications and services
●
Mental health counselor (MHC) services (also available through an acceptable telehealth mental
health disorder service site)
●
Addiction counselors or alcohol and drug counselors who meet the applicable MHC requirements
can enroll in Medicare as MHCs
●
Narcosynthesis, a form of narcoanalysis when a patient recalls repressed memories under hypnosis
●
PIN services, which help patients who are diagnosed with high-risk conditions (for example, mental
health conditions, SUD, and cancer) identify and connect with appropriate clinical and social
support resources
●
PIN services can be performed after a psychiatric evaluation, which can serve as the initiating visit
●
Principal illness navigation-peer support (PIN-PS) services, which are similar to PIN services except
they have more focus on services performed by peer support specialists under general supervision
●
Psychiatric collaborative care services using BHI to enhance primary care services and include a
psychiatric consultant
●
Psychoanalysis that treats mental disorders by investigating the interaction of conscious and
unconscious elements
●
Psychiatric evaluation that systematically evaluates a psychiatric disorder’s causes, symptoms,
course, and consequences
●
Screening, brief intervention, and referral to treatment (SBIRT) services that are early
interventions for people with non-dependent substance use to help them prevent more extensive
or specialized treatment
●
SDOH risk assessment when you have reason to believe there are unmet SDOH needs interfering
with the practitioner’s diagnosis and treatment of a patient’s condition or illness or will inuence
the patient’s choice of treatment plan or plan of care
●
You may provide an SDOH risk assessment with an E/M visit, AWV, or behavioral health oce
visit, like psychiatric diagnostic evaluation and health behavior assessment and intervention
●
SUD treatment in a patient’s home (an acceptable telehealth substance use treatment or a
co-occurring mental health disorder service site)
●
Tobacco use cessation counseling
●
Therapeutic activities that can improve the patient’s condition, like occupational therapy, recreational
therapy, and milieu therapies

Medicare & Mental Health Coverage MLN Booklet
Page 9 of 44 MLN1986542 July 2024
●
Transitional care management, within 30 days of an inpatient hospital setting discharge, interactive
contact, certain non-face-to-face services, and face-to-face visits
●
Urgent care to treat sudden illness or injury that doesn’t need emergency medical attention to
prevent disability or death
Your patients can nd more information in the Roadmap to Behavioral Health guide to understand
how to use their health coverage to improve their mental and physical health.
Non-Covered Services
We don’t cover these mental health services:
●
Environmental intervention or modications
●
Adult day health programs, like structured therapeutic health services and supervised activities
●
Biofeedback training (any modality)
●
Pastoral counseling
●
Preparing reports
●
Interpreting or explaining results or data
●
Hemodialysis specically for treating schizophrenia (experimental)
●
Transportation or outpatient meals
●
Phone apps
Prescription Drug Coverage
Medicare Part A and Part B generally don’t cover drugs, but Part B covers some medications patients
can’t self-administer. For other prescription coverage, patients must enroll in a separate Medicare
drug plan.
Drug plans cover certain protected mental health treatment drug classes, including antipsychotics,
antidepressants, and anticonvulsants. Drug plans must cover most medications in these drug classes,
with some exceptions.
Medicare Advantage Organizations
Medicare Advantage (MA) enrollees can get Part A, Part B, and Part D benets under a single
plan. MA Plans provide Part B-covered mental health services and may oer certain (for example,
telehealth) benets beyond what Part B pays. They may also provide supplemental benets Parts
A or B don’t cover. For example, supplemental mental health benets may address coping with life
changes, conict resolution, or grief counseling, all oered as individual or group sessions.

Medicare & Mental Health Coverage MLN Booklet
Page 10 of 44 MLN1986542 July 2024
Eligible Professionals
The sections below list the required qualications, coverage requirements, and the Medicare PFS
payment amount that physicians and these practitioners are eligible to bill and be paid under the
Medicare Part B Program:
●
Physicians (Medical Doctors (MDs) and Doctors of Osteopathy (DOs)), particularly Psychiatrists
●
Clinical Psychologists (CPs)
●
Clinical Social Workers (CSWs)
●
Clinical Nurse Specialists (CNSs)
●
Nurse Practitioners (NPs)
●
Physician Assistants (PAs)
●
Certied Nurse-Midwives (CNMs)
●
Independently Practicing Psychologists (IPPs)
●
Certied Registered Nurse Anesthetists (CRNAs) (supervision of diagnostic psychological and
neuropsychological tests)
●
Marriage and Family Therapists (MFTs)
●
Mental Health Counselors (MHCs)

Medicare & Mental Health Coverage MLN Booklet
Page 11 of 44 MLN1986542 July 2024
Provider Information
These sections list individual provider-type required qualications, coverage, and payment criteria. Each
provider type must meet all qualications and coverage requirements. See the Commonly Used CPT Codes
section for specic billing codes.
Physician
Required Qualications
●
MD or DO
●
Legally authorized to practice medicine in the state
where you provide services
●
Act within the scope of your license
Coverage Requirements
●
We don’t statutorily preclude the services, and they’re
reasonable and necessary
●
Generally, in addition to performing tests, you may also
supervise the performance of diagnostic psychological and
neuropsychological tests
●
You may have services and supplies provided incident to your personal professional services
Payment
Paid at 100% under the Medicare PFS

Medicare & Mental Health Coverage MLN Booklet
Page 12 of 44 MLN1986542 July 2024
Clinical Psychologist (CP)
Required Qualications
●
Psychology doctoral degree
●
Licensed or certied in the state where you practice at
the independent level and directly provide diagnostic,
assessment, preventive, and therapeutic patient services
Coverage Requirements
●
Legally authorized to practice psychology in the state
where you provide services
●
We don’t statutorily preclude the services, and they’re
reasonable and necessary
●
If the patient consents, attempt to consult their attending or
primary care physician about provided services and either:
●
Document the date the patient consented or declined the
consultation and the consultation dates in the patient’s medical record
●
Document in the patient’s medical record if consultations are unsuccessful with the date and
the physician notication method (doesn’t apply if the physician referred the patient to a CP)
●
Generally, in addition to personally performing diagnostic psychological and neuropsychological
tests, you may supervise the performance of diagnostic psychological and neuropsychological tests
●
You may have services and supplies provided incident to your personal professional services
Payment
●
We pay only on assignment
●
Paid at 100% of assigned services under the Medicare PFS

Medicare & Mental Health Coverage MLN Booklet
Page 13 of 44 MLN1986542 July 2024
Clinical Social Worker (CSW)
Required Qualications
●
Social work master’s or doctoral degree
●
At least 2 years of supervised clinical social work
●
Licensed or certied CSW by the state where you
provide services
●
If you practice in a state that doesn’t have licensure or
certication and you completed at least 2 years or 3,000
hours of post-master’s degree clinical supervised
experience in social work practice in an appropriate setting
(for example, a hospital, skilled nursing facility (SNF), or clinic)
Coverage Requirements
●
Legally authorized to practice clinical social work in the state where you provide services
●
We don’t statutorily preclude the services, and they’re reasonable and necessary
●
You provide mental health services for diagnosing and treating a mental illness and you’re legally
authorized to perform them under state law
●
We cover CSW hospital outpatient services and pay for CSW services under the CSW benet
category when hospitals bill under the CSW’s NPI
●
We don’t pay CSWs under the CSW benet category for their hospital inpatient services
●
We don’t pay under the CSW benet category for CSW services to patients under a PHP or an
IOP by a hospital outpatient department or CMHC
●
We don’t pay under the CSW benet category for CSW services to SNF inpatients and patients
in Medicare-participating ESRD facilities if the services are under the respective provider’s
participation requirements
●
We may cover ancillary CSW services when provided as auxiliary personnel incident to the
personal professional services of a physician, CP, CNS, NP, PA, or CNM
●
We don’t cover services provided incident to your personal professional services
Payment
●
We pay only on assignment
●
Paid at 80% of the lesser of the actual charge for the service or 75% of the CP’s Medicare PFS

Medicare & Mental Health Coverage MLN Booklet
Page 14 of 44 MLN1986542 July 2024
Clinical Nurse Specialist (CNS)
Required Qualications
●
Be a registered nurse (RN) currently licensed in the state
where you practice and authorized to provide CNS services
according to state law
●
Doctor of Nursing Practice or master’s degree in a dened
clinical nursing area from an accredited educational
institution
●
Certied as a CNS by a recognized national certifying body
with established CNS standards
Coverage Requirements
●
Legally authorized to practice medicine in the state where you provide services
●
We don’t statutorily preclude the services, and they’re reasonable and necessary
●
We consider the services physicians’ services if they’re provided by an MD or a DO
●
You provide the services while working in collaboration with a physician
●
We may cover assistant-at-surgery services you provide
●
You may personally perform diagnostic psychological and neuropsychological tests to the extent
authorized by state law to perform tests in collaboration with a physician as required under the
CNS benet; we authorize CNSs to supervise the performance of diagnostic tests according to
state law and scope of practice
●
You may have services and supplies provided incident to your personal professional services
Payment
●
We pay only on assignment
●
If you provide services on assignment, you can’t charge a patient more than the amounts
permitted under 42 CFR 424.55
●
If a patient paid for a service over these limits, refund their payment
●
We pay for services at 80% of the lesser of the actual charge or 85% of the amount a physician
gets under the Medicare PFS
●
We pay for assistant-at-surgery services directly at 85% of 16% of the amount a physician gets
under the Medicare PFS

Medicare & Mental Health Coverage MLN Booklet
Page 15 of 44 MLN1986542 July 2024
Nurse Practitioner (NP)
Required Qualications
●
Be an RN licensed and authorized by the state where you
provide NP services according to state law
●
Be a registered professional nurse who’s authorized by the
state where you provide services to practice as an NP by
December 31, 2000
●
Got Medicare NP billing privileges for the rst time since
January 1, 2003, and:
●
NP certied by a recognized national certifying body with established NP standards
●
Master’s degree in nursing or a Doctor of Nursing Practice doctoral degree
●
Got Medicare NP billing privileges for the rst time before January 1, 2003, and meet
certication requirements
●
Got Medicare NP billing privileges for the rst time before January 1, 2001
Coverage Requirements
●
Legally authorized to practice medicine in the state where you provide services
●
We don’t statutorily preclude the services, and they’re reasonable and necessary
●
We consider the services physicians’ services if they’re provided by an MD or a DO
●
You provide the services while working in collaboration with a physician
●
We may cover assistant-at-surgery services you provide
●
You may personally perform diagnostic psychological and neuropsychological tests to the extent
authorized by state law to perform tests in collaboration with a physician as required under the NP
benet; we authorize NPs to supervise the performance of diagnostic tests according to state law
and scope of practice
●
You may have services and supplies provided incident to your personal professional services
Payment
●
We pay only on assignment
●
If you provide services on assignment, you can’t charge a patient more than the amounts permitted
under 42 CFR 424.55
●
If a patient paid for a service over these limits, refund their payment
●
We pay for services at 80% of the lesser of the actual charge or 85% of the amount a physician
gets under the Medicare PFS
●
We pay for assistant-at-surgery services directly at 85% of 16% of the amount a physician gets
under the Medicare PFS

Medicare & Mental Health Coverage MLN Booklet
Page 16 of 44 MLN1986542 July 2024
Physician Assistant (PA)
Required Qualications
●
Licensed by the state where you practice and 1 of these
criteria apply:
●
Graduated from a PA educational program accredited
by the Accreditation Review Commission on Education
for the Physician Assistant (or its predecessor agencies,
the Commission on Accreditation of Allied Health
Education Programs and the Committee on Allied
Health Education and Accreditation)
●
Passed a national certication exam administered
by the National Commission on Certication of
Physician Assistants
Coverage Requirements
●
Legally authorized to practice medicine in the state where you provide services
●
We don’t statutorily preclude the services, and they’re reasonable and necessary
●
We consider the services physicians’ services if provided by an MD or a DO
●
Someone who meets all PA qualications provides the services
●
You provide services under an MD or a DO’s supervision
●
We may cover assistant-at-surgery services you provide
●
You may personally perform diagnostic psychological and neuropsychological tests under physician
supervision as required under the PA benet category and as authorized by state law; we authorize
PAs to supervise the performance of diagnostic tests according to state law and scope of practice
●
You may have services and supplies provided incident to your personal professional services
Payment
●
We pay only on assignment
●
If you provide services on assignment, you can’t charge a patient more than the amounts
permitted under 42 CFR 424.55
●
If a patient paid for a service over these limits, refund their payment
●
We pay for your professional services, including services and supplies provided incident to
your services
●
We pay for your professional services provided in all rural and non-rural settings and areas
●
We pay only if no facility or other provider charges or we didn’t pay any other service amount
they provided

Medicare & Mental Health Coverage MLN Booklet
Page 17 of 44 MLN1986542 July 2024
●
We pay for services at 80% of the lesser of the actual charge or at 85% of the amount a physician
gets under the Medicare PFS
●
We pay for your assistant-at-surgery services directly at 85% of 16% of the amount a physician
gets under the Medicare PFS
●
We pay for services provided incident to a PA outside a hospital at 85% of the amount a physician
gets under the Medicare PFS
●
When you bill a hospital inpatient and outpatient service directly, we unbundle the payment and
pay you directly
●
You can bill Medicare and we pay for your services directly like we do NPs and CNSs
●
You may reassign your service payment rights and incorporate as a group of practitioners only in
your specialty and bill Medicare like NPs and CNSs
●
Bill under your NPI

Medicare & Mental Health Coverage MLN Booklet
Page 18 of 44 MLN1986542 July 2024
Certied Nurse-Midwife (CNM)
Required Qualications
●
RN legally authorized to practice as a nurse-midwife in the
state where you provide services
●
Successfully completed a nurse-midwives program of study
and got clinical experience accredited by an accrediting
body the U.S. Department of Education approves
●
Certied as a Nurse-Midwife by the American College of
Nurse-Midwives or the American College of Nurse-Midwives
Certication Council
Coverage Requirements
●
Legally authorized to practice medicine in the state where
you provide services
●
We don’t statutorily preclude the services, and they’re
reasonable and necessary
●
We consider the services physicians’ services if they’re
provided by an MD or a DO
●
You provide the services without physician supervision and without association with a physician or
other health care provider, unless otherwise required under state law
●
You may personally perform diagnostic psychological and neuropsychological tests without
physician supervision or oversight as required under the CNM benet category and as authorized
under state law; we authorize CNMs to supervise diagnostic tests performed according to state
law and scope of practice
●
You may have services and supplies provided incident to your personal professional services
Payment
●
We pay only on assignment
●
If you provide services on assignment, you can’t charge a patient more than the amounts
permitted under 42 CFR 424.55
●
If a patient paid for a service over these limits, refund their payment
●
We pay for services at 80% of the lesser of the actual charge, or 100% of the amount a physician
gets under the Medicare PFS

Medicare & Mental Health Coverage MLN Booklet
Page 19 of 44 MLN1986542 July 2024
Independently Practicing Psychologist (IPP)
Required Qualications
●
Psychologist who isn’t a CP
●
Meets 1 of these criteria:
●
Practices independent of an institution, agency, or
physician’s oce and is licensed or certied to practice
psychology in the state or jurisdiction where you
provide the services
●
Practicing psychologist who provides services in a
jurisdiction that doesn’t issue licenses
Coverage Requirements
●
We don’t statutorily preclude the services, and they’re reasonable and necessary
●
Provide services on your own responsibility, free of administrative and professional control of an
employer (for example, physician, institution, or agency)
●
You treat your own patients
●
When you practice in an oce in an institution:
●
The oce is conned to a separately identied part of the facility used solely as an oce and
not confused as extending throughout the entire institution
●
You operate a private practice (patients outside an institution and non-institutional patients)
●
You may perform diagnostic psychological and neuropsychological tests when a physician or
certain NPPs order them
●
You can bill directly and collect and retain service fees
Payment
●
We don’t subject diagnostic psychological and neuropsychological tests to assignment; however,
on the claim, include the name and address of the physician or NPP who orders the tests
●
Paid at 100% of Medicare PFS for diagnostic tests

Medicare & Mental Health Coverage MLN Booklet
Page 20 of 44 MLN1986542 July 2024
Certied Registered Nurse
Anesthetist (CRNA)
Required Qualications
●
Licensed as a registered professional nurse by the state
where you practice
●
Meet any licensure requirements the state imposes on
non-physician anesthetists
●
Graduated from a nurse anesthesia educational program
that meets standards of the Council on Accreditation of
Nurse Anesthesia Educational Programs (COA) or other
accreditation organization the HHS Secretary designates
●
Passed a National Board of Certication & Recertication
for Nurse Anesthetists (NBCRNA) certication exam
●
Graduated from a nurse anesthesia educational program that meets the COA Educational Program’s
standards and, within 24 months of graduation, passed a certication exam from NBCRNA or
another certication organization the HHS Secretary designates
Coverage Requirements
●
Legally authorized to practice medicine in the state where you provide services
●
We don’t statutorily preclude the services, and they’re reasonable and necessary
●
You may personally perform diagnostic psychological and neuropsychological tests under physician
supervision as required under the CRNA benet category and as authorized by state law; we
authorize CRNAs to supervise the performance of diagnostic tests according to state law and
scope of practice
●
You can bill directly and collect and retain service fees
Payment
●
Paid at 100% under the Medicare PFS as determined by the level of required supervision
●
You may bill your services directly to Medicare, get paid directly, or have payment made to any
person or entity (for example, hospital, critical access hospital (CAH), physician, group practice,
or ambulatory surgical center) if you have an employment or contractor relationship that’s paying
you or them

Medicare & Mental Health Coverage MLN Booklet
Page 21 of 44 MLN1986542 July 2024
Marriage & Family Therapist (MFT)
Required Qualications
●
Master’s or doctor’s degree that qualies for licensure or
certication as an MFT according to the state law where you
provide services
●
Licensed or certied as an MFT in the state where you
provide services
●
After getting your degree, you complete at least 2 years
or 3,000 hours of post-master’s degree clinical supervised
experience in marriage and family therapy in an appropriate
setting (for example, a hospital, SNF, or clinic)
Coverage Requirements
●
Legally authorized to practice as an MFT in the state where you provide services
●
You may enroll in Medicare and bill Medicare independently beginning January 1, 2024
●
You may also still provide services and supplies as auxiliary personnel incident to a physician’s or
certain NPP’s personal professional service
Payment
●
We pay only on assignment
●
We pay for services at 80% of the lesser of the actual charge or 75% of the amount a CP gets
under the Medicare PFS
●
We don’t pay under the MFT benet category for MFT services to patients under a PHP or an IOP
by a hospital outpatient department or CMHC
●
We exclude MFT services provided to SNF residents on or after January 1, 2024, from
consolidated billing
●
Include the SNF’s Medicare provider number when you bill for these Part B services
Medicare & Mental Health Coverage MLN Booklet
Page 22 of 44 MLN1986542 July 2024
Mental Health Counselor (MHC)
Required Qualications
●
Master’s or doctor’s degree that qualies for licensure or
certication as an MHC according to the state law where you
provide MHC services
●
Licensed or certied as an MHC; a clinical professional
counselor; an addiction, alcohol, or drug counselor; or a
professional counselor in the state where you provide services
●
After getting your degree and you complete at least 2 years
or 3,000 hours of clinical supervised experience in mental
health counseling
Coverage Requirements
●
Legally authorized to practice as an MHC in the state where you provide services
●
You may enroll in Medicare and bill Medicare independently beginning January 1, 2024
●
You may also still provide services and supplies as auxiliary personnel incident to a physician’s or
certain NPP’s personal professional service
Payment
●
We pay only on assignment
●
We pay for services at 80% of the lesser of the actual charge or 75% of the amount a CP gets
under the Medicare PFS
●
We don’t pay under the MHC benet category for MHC services to patients under a PHP or an
IOP by a hospital outpatient department or CMHC
●
We exclude MHC services provided to SNF residents on or after January 1, 2024, from
consolidated billing
●
Include the SNF’s Medicare provider number when you bill for these Part B services

Medicare & Mental Health Coverage MLN Booklet
Page 23 of 44 MLN1986542 July 2024
Incident to Provision
Physicians and certain NPPs have a provision under their benet category that authorizes them to
have ancillary services and supplies provided by auxiliary personnel “incident to” their own personal
professional services.
Physicians and specically CPs, NPs, CNSs, CNMs, and PAs can bill and be paid for these integral,
although incidental, services and supplies provided by auxiliary personnel as if they furnished the
services themselves if all the incident to requirements are met. However, under the Medicare PFS,
Medicare doesn’t pay physicians or NPPs for incident to services in an institutional setting (hospital
or SNF).
●
Services and supplies are integral to the patient’s normal treatment course, and the physician or
other listed NPP personally furnished an initial service to which the auxiliary personnel’s services
are incidental. The physician or NPP must remain actively involved in treating the patient.
●
The auxiliary personnel provide services and supplies without charge (included in the physician’s
or other listed NPP’s bill).
●
Services and supplies are an expense to the physician or other listed NPP.
●
Services and supplies are commonly oered in the physician’s or other listed NPP’s oce or clinic.
●
Typically, the incident to regulations require the physician or other listed NPP to furnish direct
supervision; they’re present in the oce suite and immediately available if needed.
We oer an exception to the direct supervision requirement for incident to behavioral health services
provided by auxiliary personnel. In other words, incident to behavioral health services can be provided
under the general supervision of a physician or an NPP instead of direct supervision. Under general
supervision, the physician or NPP may be contacted by phone, if necessary, as the physician’s or
NPP’s presence isn’t required during a procedure.
We don’t dene behavioral health services by HCPCS codes; however, we generally understand a
behavioral health service to be any service a provider furnishes for the diagnosis, evaluation, or
treatment of a mental health disorder, including an SUD.
Physicians, NPPs, and practitioners can also serve as auxiliary personnel and provide services
and supplies incident to the personal professional services of another physician or NPP. Appropriate
payment can be made to the other supervising physician, or NPP in this case, if you meet all the
incident to requirements.
42 CFR 410.26 and 42 CFR 410.27 have more information.

Medicare & Mental Health Coverage MLN Booklet
Page 24 of 44 MLN1986542 July 2024
Commonly Used CPT Codes
With thousands of CPT codes, using the correct CPT code to show the mental health services you
provide to patients is essential for billing correctly.
Note:
Only certain codes are billable as part of a PHP or an IOP. View Sections 260 and 261 of the
Medicare Claims Processing Manual, Chapter 4 for more information.
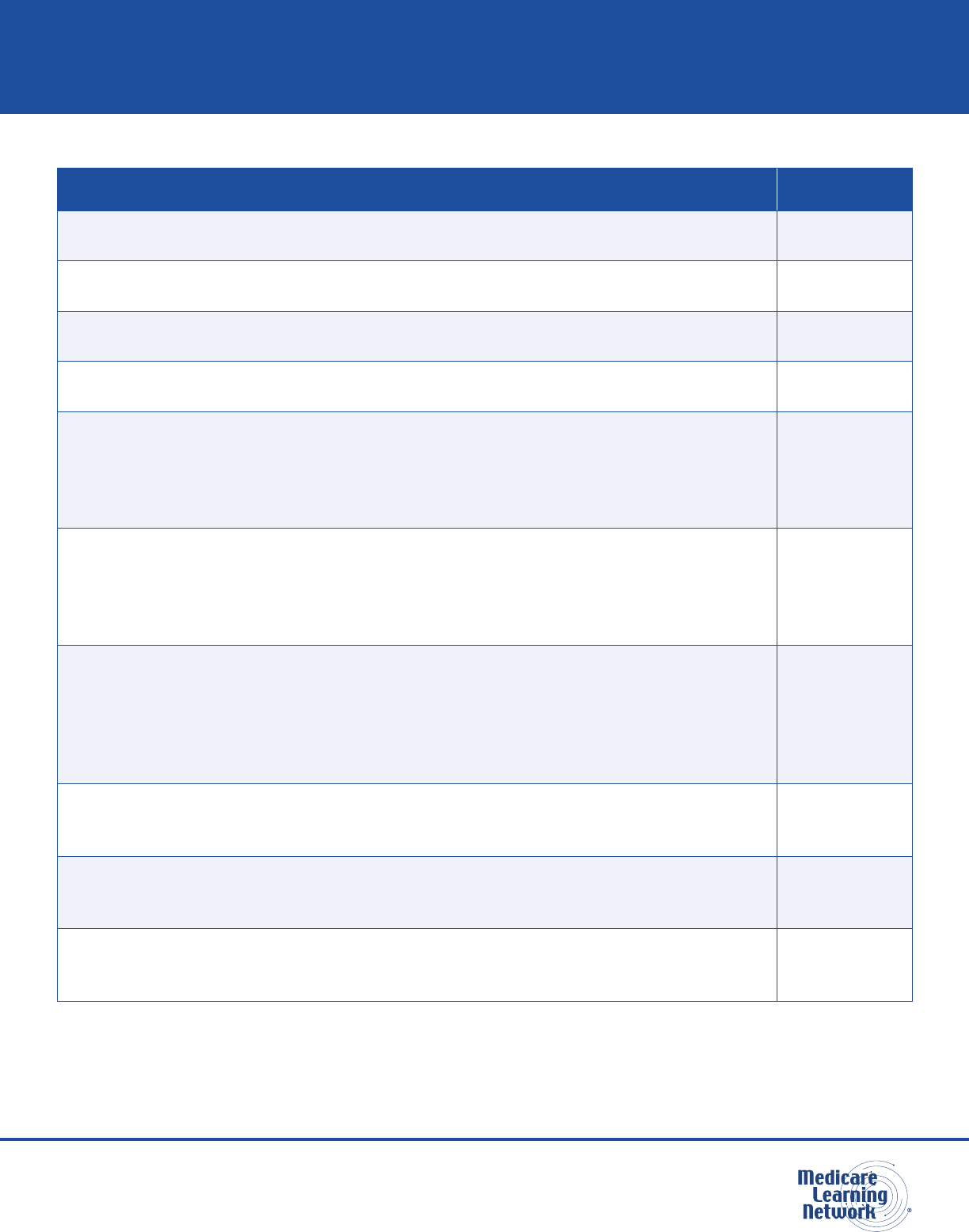
Table 1. Commonly Used Mental Health-Related CPT Codes
Description CPT Code
Interactive complexity (List separately in addition to the code for primary procedure)
(Use 90785 in conjunction with codes for diagnostic psychiatric evaluation [90791,
90792], psychotherapy [90832, 90833, 90834, 90836, 90837, 90838), and group
psychotherapy [90853])
(Use 90785 in conjunction with 90853 for the specied patient when group
psychotherapy includes interactive complexity)
90785
Psychiatric diagnostic evaluation 90791
Psychiatric diagnostic evaluation with medical services
(Use 90785 in conjunction with 90791, 90792 when the diagnostic evaluation
includes interactive complexity services)
90792
Psychotherapy, 30 minutes with patient 90832
Psychotherapy, 30 minutes with patient when performed with an evaluation and
management service (List separately in addition to the code for primary procedure)
90833
Psychotherapy, 45 minutes with patient 90834
Psychotherapy, 45 minutes with patient when performed with an evaluation and
management service (List separately in addition to the code for primary procedure)
90836
Psychotherapy, 60 minutes with patient 90837
Psychotherapy, 60 minutes with patient when performed with an evaluation and
management service (List separately in addition to the code for primary procedure)
90838
Psychotherapy for crisis; rst 60 minutes 90839
Psychotherapy for crisis; each additional 30 minutes (List separately in addition to
code for primary service)
90840
Psychoanalysis 90845
Family psychotherapy (without the patient present), 50 minutes 90846
Family psychotherapy (conjoint psychotherapy) (with patient present), 50 minutes 90847
Multiple-family group psychotherapy 90849
Group psychotherapy (other than of a multiple-family group) 90853
CPT only copyright 2023 American Medical Association. All rights reserved.

Medicare & Mental Health Coverage MLN Booklet
Page 25 of 44 MLN1986542 July 2024
Table 1. Commonly Used Mental Health-Related CPT Codes (cont.)
Description CPT Code
Electroconvulsive therapy (includes necessary monitoring) 90870
Hypnotherapy 90880
Preparation of report of patient’s psychiatric status, history, treatment, or progress
(other than for legal or consultative purposes) for other individuals, agencies, or
insurance carriers
90889
Assessment of aphasia (includes assessment of expressive and receptive speech
and language function, language comprehension, speech production ability,
reading, spelling, writing, eg, by Boston Diagnostic Aphasia Examination) with
interpretation and report, per hour
96105
Developmental test administration (including assessment of ne and/or gross
motor, language, cognitive level, social, memory and/or executive functions by
standardized developmental instruments when performed), by physician or other
qualied health care professional, with interpretation and report; rst hour
96112
Developmental test administration (including assessment of ne and/or gross
motor, language, cognitive level, social, memory and/or executive functions by
standardized developmental instruments when performed), by physician or other
qualied health care professional, with interpretation and report; each additional 30
minutes (List separately in addition to code for primary procedure)
96113
Neurobehavioral status exam (clinical assessment of thinking, reasoning and
judgment, [eg, acquired knowledge, attention, language, memory, planning and
problem solving, and visual spatial abilities]), by physician or other qualied health
care professional, both face-to-face time with the patient and time interpreting test
results and preparing the report; rst hour
96116
Neurobehavioral status exam (clinical assessment of thinking, reasoning and judgment,
[eg, acquired knowledge, attention, language, memory, planning and problem solving,
and visual spatial abilities]), by physician or other qualied health care professional,
both face-to-face time with the patient and time interpreting test results and preparing
the report; each additional hour (List separately in addition to code for primary procedure)
96121
Psychological testing evaluation services by physician or other qualied health care
professional, including integration of patient data, interpretation of standardized test results
and clinical data, clinical decision making, treatment planning and report, and interactive
feedback to the patient, family member(s) or caregiver(s), when performed; rst hour
96130
Psychological testing evaluation services by physician or other qualied health care
professional, including integration of patient data, interpretation of standardized test
results and clinical data, clinical decision making, treatment planning and report, and
interactive feedback to the patient, family member(s) or caregiver(s), when performed;
each additional hour (List separately in addition to code for primary procedure)
96131
CPT only copyright 2023 American Medical Association. All rights reserved.

Medicare & Mental Health Coverage MLN Booklet
Page 26 of 44 MLN1986542 July 2024
Table 1. Commonly Used Mental Health-Related CPT Codes (cont.)
Description CPT Code
Neuropsychological testing evaluation services by physician or other qualied
health care professional, including integration of patient data, interpretation of
standardized test results and clinical data, clinical decision making, treatment
planning and report, and interactive feedback to the patient, family member(s) or
caregiver(s), when performed; rst hour
96132
Neuropsychological testing evaluation services by physician or other qualied health
care professional, including integration of patient data, interpretation of standardized
test results and clinical data, clinical decision making, treatment planning and report,
and interactive feedback to the patient, family member(s) or caregiver(s), when
performed; each additional hour (List separately in addition to code for primary procedure)
96133
Psychological or neuropsychological test administration and scoring by physician or
other qualied health care professional, two or more tests, any method; rst 30 minutes
96136
Psychological or neuropsychological test administration and scoring by physician
or other qualied health care professional, two or more tests, any method; each
additional 30 minutes (List separately in addition to code for primary procedure)
96137
Psychological or neuropsychological test administration and scoring by technician,
two or more tests, any method; rst 30 minutes
96138
Psychological or neuropsychological test administration and scoring by technician,
two or more tests, any method; each additional 30 minutes (List separately in
addition to code for primary procedure)
96139
Psychological or neuropsychological test administration, with single automated,
standardized instrument via electronic platform, with automated result only
96146
Health behavior assessment, or re-assessment (ie, health-focused clinical interview,
behavioral observations, clinical decision making)
96156*
Health behavior intervention, individual, face-to-face; initial 30 minutes 96158*
Health behavior intervention, individual, face-to-face; each additional 15 minutes
(List separately in addition to code for primary service)
96159*
Administration of caregiver-focused health risk assessment instrument (eg,
depression inventory) for the benet of the patient, with scoring and documentation,
per standardized instrument
96161
Health behavior intervention, group (2 or more patients), face-to-face; initial
30 minutes
96164*
Health behavior intervention, group (2 or more patients), face-to-face; each
additional 15 minutes (List separately in addition to code for primary service)
96165*
CPT only copyright 2023 American Medical Association. All rights reserved.
*CPs, CSWs, MFTs, and MHCs can bill these codes.
Medicare & Mental Health Coverage MLN Booklet
Page 27 of 44 MLN1986542 July 2024
Table 1. Commonly Used Mental Health-Related CPT Codes (cont.)
Description CPT Code
Health behavior intervention, family (with the patient present), face-to-face; initial
30 minutes
96167*
Health behavior intervention, family (with the patient present), face-to-face; each
additional 15 minutes (List separately in addition to code for primary service)
96168*
Health behavior intervention, family (without the patient present), face-to-face; initial
30 minutes
96170*
Health behavior intervention, family (without the patient present), face-to-face;
each additional 15 minutes (List separately in addition to code for primary service)
96171*
Multiple-family group behavior management/modication training for parent(s)/
guardian(s)/caregiver(s) of patients with a mental or physical health diagnosis,
administered by physician or other qualied health care professional (without
the patient present), face-to-face with multiple sets of parent(s)/guardian(s)/
caregiver(s); initial 60 minutes
96202
Multiple-family group behavior management/modication training for parent(s)/
guardian(s)/caregiver(s) of patients with a mental or physical health diagnosis,
administered by physician or other qualied health care professional (without the
patient present), face-to-face with multiple sets of parent(s)/guardian(s)/caregiver(s);
each additional 15 minutes (List separately in addition to code for primary service)
96203
Behavior identication assessment, administered by a physician or other qualied
health care professional, each 15 minutes of the physician’s or other qualied health
care professional’s time face-to-face with patient and/or guardian(s)/caregivers(s)
administering assessments and discussing ndings and recommendations, and
non face-to-face analyzing past data, scoring/interpreting the assessment, and
preparing the report/treatment plan
97151
Behavior identication-supporting assessment, administered by one technician
under the direction of a physician or other qualied health care professional,
face-to-face with the patient, each 15 minutes
97152
Adaptive behavior treatment by protocol, administered by technician under the
direction of a physician or other qualied health care professional, face-to-face with
one patient, each 15 minutes
97153
Group adaptive behavior treatment by protocol, administered by technician
under the direction of a physician or other qualied health care professional,
face-to-face with two or more patients, each 15 minutes
97154
CPT only copyright 2023 American Medical Association. All rights reserved.
*CPs, CSWs, MFTs, and MHCs can bill these codes.

Medicare & Mental Health Coverage MLN Booklet
Page 28 of 44 MLN1986542 July 2024
Table 1. Commonly Used Mental Health-Related CPT Codes (cont.)
Description CPT Code
Adaptive behavior treatment with protocol modication, administered by physician
or other qualied health care professional, which may include simultaneous
direction of technician, face-to-face with one patient, each 15 minutes
97155
Family adaptive behavior treatment guidance, administered by physician or other
qualied health care professional (with or without the patient present), face-to-face
with guardian(s)/caregivers(s), each 15 minutes
97156
Multiple-family group adaptive behavior treatment guidance, administered by
physician or other qualied health care professional (without the patient present),
face-to-face with multiple sets of guardians/caregivers, each 15 minutes
97157
Group adaptive behavior treatment with protocol modication, administered by
physician or other qualied health care professional, face-to-face with multiple
patients, each 15 minutes
97158
Caregiver training in strategies and techniques to facilitate the patient’s functional
performance in the home or community (eg, activities of daily living [ADLs], instrumental
ADLs [iADLs], transfers, mobility, communication, swallowing, feeding, problem solving,
safety practices) (without the patient present), face to face; initial 30 minutes
97550
Caregiver training in strategies and techniques to facilitate the patient’s functional
performance in the home or community (eg, activities of daily living [ADLs], instrumental
ADLs [iADLs], transfers, mobility, communication, swallowing, feeding, problem solving,
safety practices) (without the patient present), face to face, each additional 15 minutes
(List separately in addition to code for primary service)
97551
Group caregiver training in strategies and techniques to facilitate the patient’s
functional performance in the home or community (eg, activities of daily living [ADLs],
instrumental ADLs [iADLs], transfers, mobility, communication, swallowing, feeding,
problem solving, safety practices) (without the patient present), face to face with
multiple sets of caregivers
97552
HCPCS code G0136 (Administration of a standardized, evidence-based social determinants of health
risk assessment tool, 5–15 minutes), not provided more often than every 6 months, can also be
provided
with CPT code 90791 (Psychiatric diagnostic evaluation) and the health behavior
assessment and intervention (HBAI) services, described by CPT codes 96156, 96158, 96159, 96164,
96165, 96167, and 96168. We allow the HBAI services described by the above CPT codes, and any
successor codes, to be billed by CPs, CSWs, MFT s, and MHCs.
CPT only copyright 2023 American Medical Association. All rights reserved.

Medicare & Mental Health Coverage MLN Booklet
Page 29 of 44 MLN1986542 July 2024
National Correct Coding Initiative
The National Correct Coding Initiative (NCCI) promotes national correct coding methods and oers
national guidance on code pair edits preventing billing certain services on the same day.
Outpatient Psychiatric Hospital Services
Outpatient psychiatric hospital services and supplies are:
●
Medically necessary for diagnostic study or if the patient’s condition is reasonably expected to
improve (see the Same Day Billing Guidelines section for more information)
●
Provided under an individualized, written plan of care (POC) that states the:
●
Type, amount, frequency, and services duration
●
Diagnosis
●
Expected goals (except when you only provide a few brief services)
●
Supervised and periodically evaluated by a physician who:
●
Prescribes the services
●
Determines the extent the patient reached treatment goals and if the POC should change
●
Provides supervision and direction to therapists treating the patient
●
Documents their involvement in the patient’s medical record
●
For diagnostic study or, at a minimum, designed to reduce or control a patient’s psychiatric symptoms
to prevent a relapse or hospitalization and improve or maintain their level of functioning
Generally, we cover these outpatient hospital psychiatric treatment services:
●
Medically necessary diagnostic services for patients when extended or direct observation is
necessary to determine functioning and interactions, identify problem areas, and prepare a POC
●
Individual and group psychotherapy with physicians, CPs, CSWs, or other eligible providers
authorized or licensed by the state where they provide services
●
Social workers, psychiatric nurses, and other sta trained to work with psychiatric patients
●
Occupational therapy services, when part of a PHP or an IOP, that:
●
Require qualied occupational therapist skills
●
Are provided by, or under supervision of, a qualied occupational therapist
●
Are included in a patient’s POC
●
Activity therapies, when part of a PHP or an IOP, that:
●
Are individualized and essential for treating a patient’s diagnosed condition and progressing
toward treatment goals
●
Have a POC that clearly supports and shows each therapy’s need (not primarily recreational
or diversionary)

Medicare & Mental Health Coverage MLN Booklet
Page 30 of 44 MLN1986542 July 2024
●
Family counseling services while treating a person’s condition
●
Patient training and education when they’re closely and clearly related to care and treating an
individual’s diagnosed psychiatric condition
●
Therapeutic drugs and biologicals a patient can’t self-administer
●
CCM to patients with multiple chronic conditions (for example, patients with dementia typically have
multiple chronic conditions that could involve physical and behavioral health issues, like depression)
Telehealth
Beginning in 2025, in-person visit requirements will apply for mental health services provided by
telehealth. This includes a required in-person visit within the 6 months before the initial telehealth
treatment as well as the required subsequent in-person visits at least every 12 months.
We’ll continue to dene direct supervision to permit the immediate availability of the supervising
practitioner through real-time audio and visual interactive telecommunications through
December 31, 2024.
The regulations at 42 CFR 410.78(b)(3)(xiv) describe 2 exceptions to the in-person requirements that
take eect on January 1, 2025:
1. Patients who already get telehealth behavioral health services and have circumstances where
in-person care may not be appropriate
2. Groups with limited availability for in-person behavioral health visits have the exibility to arrange for
practitioners to provide in-person and telehealth visits with dierent practitioners, based on availability
The telehealth policies described above also apply to Rural Health Clinics (RHCs) and Federally
Qualied Health Centers (FQHCs).
Beginning January 1, 2024, MHCs and MFTs can provide and bill Medicare telehealth services.
Exceptions to the in-person visit requirement require a clear justication documented in the patient’s
medical record. Hospitals must also document that patients have a regular source of general medical
care and can get any needed point-of-care testing, including vital sign monitoring and lab studies.
We created 3 Outpatient Prospective Payment System (OPPS)-specic HCPCS codes to describe
that the patient must be in their home and that no associated professional service is billed under the
PFS. Hospital sta must be licensed to provide these services consistent with all applicable state
scope of practice laws. We exempt these services from having sta physically located in the hospital
or outpatient department when providing services remotely using communication technology.

Medicare & Mental Health Coverage MLN Booklet
Page 31 of 44 MLN1986542 July 2024
Table 2. Telehealth HCPCS Codes
Description HCPCS Code
Service for diagnosis, evaluation, or treatment of a mental health or substance
use disorder, 15-29 minutes, provided remotely by hospital sta who are licensed
to provide mental health services under applicable state law(s), when the patient
is in their home, and there is no associated professional service
C7900
Service for diagnosis, evaluation, or treatment of a mental health or substance
use disorder, 30-60 minutes, provided remotely by hospital sta who are licensed
to provide mental health services under applicable state law(s), when the patient
is in their home, and there is no associated professional service
C7901
Service for diagnosis, evaluation, or treatment of a mental health or substance
use disorder, each additional 15 minutes, provided remotely by hospital sta who
are licensed to provide mental health services under applicable state law(s), when
the patient is in their home, and there is no associated professional service (list
separately in addition to code for primary service)
C7902
Administration of a standardized, evidence-based social determinants of health
risk assessment tool, 5-15 minutes
G0136
We assigned HCPCS codes C7900 and C7901 to ambulatory payment classications (APCs) based
on the PFS facility payment rates for CPT codes 96158 and 96159. C7902 is an add-on code; the
payment is packaged, and the code isn’t assigned to an APC.
Generally, we don’t cover these outpatient hospital services:
●
Meals and transportation
●
Activity therapies, group activities, or other primarily recreational or diversionary services and programs
●
Outpatient psychosocial programs (we cover outpatient psychosocial components not primarily for
social or recreational purposes)
●
Vocational training related only to specic employment opportunities
CPT only copyright 2023 American Medical Association. All rights reserved.

Medicare & Mental Health Coverage MLN Booklet
Page 32 of 44 MLN1986542 July 2024
Partial Hospitalization Program (PHP)
PHPs are distinct and structured programs that provide intensive outpatient psychiatric care through
active treatment by combining clinically recognized items and services. We cover PHP in hospital
outpatient departments and CMHCs.
Patients may pay a percentage of each doctor’s or other qualied mental health professional’s approved
service amount if they accept assignment. Patients may also pay each day’s PHP services coinsurance
in a hospital outpatient setting or CMHC.
PHPs oer psychiatric treatment less than 24 hours a day to patients:
●
Discharged from an inpatient hospital treatment and a PHP replaces continued inpatient treatment
●
At reasonable inpatient hospitalization risk without partial hospitalization
PHPs must meet these program and patient criteria:
●
Active treatment includes an individual POC with coordinated services designed for the patient’s needs
●
The POC treatment includes a physician-directed multi-disciplinary team care approach certifying
the patient’s need for partial hospitalization therapeutic services a minimum of 20 hours per week,
and this determination must occur no less frequently than monthly
●
Treatment goals should be:
●
Measurable
●
Functional
●
Time framed
●
Medically necessary
●
Directly related to admission reason
●
The patient requires a comprehensive, highly structured, scheduled, and multi-modal individualized
POC requiring medical supervision and coordination because their mental disorder severely
interferes with multiple areas of daily life (social, vocational, ADLs or instrumental ADLs, and
educational functioning)
●
The patient can cognitively and emotionally participate in the active treatment process and tolerate
its intensity
Partial hospitalization services don’t include:
●
Hospital inpatient services
●
Meals, self-administered medications, and transportation
●
Support groups where people talk and socialize (dierent than group psychotherapy, which we cover)
●
Job skills training or testing skills not part of mental health treatment

Medicare & Mental Health Coverage MLN Booklet
Page 33 of 44 MLN1986542 July 2024
Intensive Outpatient Program (IOP)
Intensive outpatient services are provided under an IOP.
Outpatients may get IOP services from their hospital, or through a CAH, a CMHC, an FQHC, or an
RHC, as a distinct and organized intensive ambulatory treatment service, oering less than 24-hour
daily care, in a location other than an individual’s home or inpatient or residential setting.
IOP services may also be provided in OTPs for treating an OUD.
Physicians prescribe an IOP for a person determined (not less frequently than once every other month)
to need these services for a minimum of 9 hours per week. They’re provided under the physician’s
supervision pursuant to an individualized, written treatment plan established and periodically
reviewed by the physician (in consultation with appropriate sta participating in such a program). This
determines the physician’s diagnosis and the type, amount, frequency, and duration of the items and
services provided under the plan and the treatment goals.
Intensive outpatient services include:
●
Individual and group therapy with physicians or psychologists (or other mental health professionals
to the extent authorized under state law)
●
Occupational therapy requiring the skills of a qualied occupational therapist
●
Services of social workers, trained psychiatric nurses, and other sta trained to work with
psychiatric patients
●
Drugs and biologicals provided for therapeutic purposes (which can’t be self-administered)
●
Individualized activity therapies that aren’t primarily recreational or diversionary
●
Family counseling (for the primary purpose of treating the individual’s condition)
●
Patient training and education (to the extent that training and educational activities are closely and
clearly related to the individual’s care and treatment)
●
Diagnostic services
●
Other items and services (excluding meals and transportation) that are reasonable and necessary for
diagnosing or actively treating the individual’s condition, can be reasonably expected to improve or
maintain the individual’s condition and functional level, and help prevent relapse or hospitalization
When a hospital provides non-intensive outpatient program mental health services to an IOP patient,
all intensive outpatient services and non-intensive outpatient mental health services should be reported
on the same hospital claim with condition code 92.
Intensive outpatient services must include a physician certication and POC. However, although PHP
requires the physician to certify that the services are instead of inpatient hospitalization, IOP services
aren’t intended for those who otherwise need an inpatient level of care.
In addition to physicians, the following NPPs may perform the required certication and POC
requirements for IOP services furnished in the OTP setting: NPs, PAs, CPs, CSWs, MHCs, MFTs,

Medicare & Mental Health Coverage MLN Booklet
Page 34 of 44 MLN1986542 July 2024
and any other NPPs dened in Section 1842(b)(18)(C) of the Social Security Act, as permitted by
state law and consistent with scope of practice requirements.
For IOP services, non-excepted o-campus provider-based departments of a hospital are required to
report a PN modier on each claim line for non-excepted items and services.
Eective January 1, 2024, for IOP services, excepted o-campus provider-based departments of a
hospital must continue to report existing modier PO (services, procedures, and surgeries provided at
o-campus provider-based outpatient departments) for all excepted items and services provided.
All hospitals are required to report condition code 92 in form locators 18–28 to indicate the claim is for
IOP services.
Community Mental Health Centers
We cover Part B partial hospitalization services that CMHCs provide, subject to the OPPS.
Medicare-authorized CMHCs must meet these program and patient criteria:
●
Have appropriate state and local CMHC licensing or certication
●
Provide:
●
Outpatient services, including specialized services for children, older adults, chronically
mentally ill patients, and residents of its service area discharged from an inpatient mental
health treatment facility
●
24-hour emergency care services with clinician access and appropriate disposition with follow-up
documentation of the emergency in the patient’s CMHC medical record
●
Day treatment, partial hospitalization services, intensive outpatient services, or psychosocial
rehabilitation services with structured daily treatment plans varying in intensity, frequency, and
duration based on the patient’s needs
●
At least 40% of its services is to patients who are ineligible for Social Security Act, Title XVIII benets
●
Clinically evaluated state mental health facility candidate admissions by clinical personnel and
authorized under state law, except those provided by a 24-hour facility; a CMHC operating in
a state that, by law, prevents it from providing these services may contract with an entity the
HHS Secretary approves
A CMHC is an originating telehealth services site.
Behavioral Health Integration (BHI) Services
Integrating behavioral health and primary care helps improve patient mental and behavioral health condition
outcomes. We separately pay physicians and NPPs providing BHI services over a calendar month.
CPs, CSWs, MFTs, and MHCs can bill the general BHI code HCPCS G0323 when they’re personally
performing services to account for monthly care integration, and those services are the focal point of
care integration. We allow general supervision for G0323.

Medicare & Mental Health Coverage MLN Booklet
Page 35 of 44 MLN1986542 July 2024
Medical Records Checklist: Outpatient Psychiatric Services
This outpatient psychiatric medical records services checklist reminds clinicians and sta of
required documentation.
Community Mental Health Center & Partial Hospitalization Program
Medical Record Content
□
Patient identication data
□
Diagnosis, including intercurrent disease diagnosis and psychiatric diagnosis
□
Indicate signicant illnesses and medical conditions on a problem list
□
Prominently note medication allergies and adverse reactions in the record; note in the record
if the patient has no known allergies or adverse history of reactions

Medicare & Mental Health Coverage MLN Booklet
Page 36 of 44 MLN1986542 July 2024
Standard Initial Evaluation
□
Complete within 24 hours of patient admission
□
Include admitting diagnosis and other diagnoses
□
Referral source
□
Admission reason as stated by the patient or other person signicantly involved
□
Identify the patient’s immediate clinical care needs for their psychiatric diagnosis
□
Current patient prescriptions list, including over-the-counter medications and other substances
they take
□
For PHPs only, an explanation of the patient’s hospitalization risk if a PHP isn’t provided
□
Identify the patient’s appropriate interdisciplinary team members
Standard Comprehensive Assessment
□
Interdisciplinary treatment team completed a timely assessment consistent with the patient’s
needs, but no later than 4 working days after the patient’s admission
□
Identies the patient’s psychiatric illness and ensures the physical, psychological, psychosocial,
emotional, and therapeutic active treatment plan needs are consistent with your ndings
□
Includes the patient’s:
□
Admission reason
□
Psychiatric evaluation containing medical history and symptoms severity
□
Previous and current mental health status information
□
Onset of illness symptoms and admission circumstances
□
Description of attitudes and behaviors aecting their treatment plan
□
Intellectual, memory functioning, and orientation assessment

Medicare & Mental Health Coverage MLN Booklet
Page 37 of 44 MLN1986542 July 2024
Standard Comprehensive Assessment (cont.)
□
Care planning risk factor complications
□
Functional status, including whether they can participate in their own care and their
strengths and goals
□
Factors aecting their or others’ safety, including suicide risk factors
□
Prescription drug prole, including over-the-counter medications
□
Referral needs and further health care professional evaluation
□
Considered discharge planning factors
□
Current social and health care support systems
□
For pediatric clients, assess social service needs and make needed referrals
□
Make interdisciplinary team updates when the patient’s status or treatment response changes
occur or when they meet goals
□
Upon patient discharge or transfer to another entity, within 2 working days the CMHC must
forward the patient’s:
□
Discharge summary
□
Clinic record, if requested
□
If the patient refuses CMHC services or is non-compliant with the treatment plan, the CMHC
must forward to their primary health care provider:
□
CMHC discharge summary copy
□
Client record, if requested
□
Discharge summary includes the patient’s:
□
Current active treatment plan
□
Most recent physician orders
□
Documentation to help in post-discharge continuity of care

Medicare & Mental Health Coverage MLN Booklet
Page 38 of 44 MLN1986542 July 2024
Acute Care Hospital
When a physician admits a patient to the hospital for inpatient psychiatric facility services, we cover
the services only if the patient needs intensive, appropriate, and active treatment in this type of setting.
The psychiatric facility must be a general hospital with a distinct psychiatric unit or a psychiatric hospital
that cares only for people with mental health conditions.
We certify inpatient psychiatric facilities (IPFs) and distinct psychiatric units in acute care hospitals
and CAHs.
We cover:
●
Semi-private rooms
●
Meals
●
General nursing
●
Drugs (including methadone to treat OUD)
●
Other inpatient hospital treatment services and supplies
Deductible and coinsurance apply. See the Coverage Period section for more information.
If appropriate, physicians can admit patients to a general acute care hospital that doesn’t have a
distinct psychiatric unit to get mental health and SUD services. These inpatient services are covered
like other inpatient services in a general acute care hospital.
Inpatient Psychiatric Facility Services
IPFs include freestanding, certied psychiatric hospitals, and psychiatric units in acute care hospitals or
CAHs, providing routine hospital and psychiatric services to diagnose and treat patients’ mental disorders.
We pay for inpatient psychiatric services under the Inpatient Psychiatric Facility Prospective
Payment System (IPF PPS) when the facility is certied and meets inpatient psychiatric hospital
services regulations.
We require updated hospital inpatient rights and discharge planning conditions of participation for
short-term acute-care, rehabilitation, psychiatric, children’s, cancer, and CAHs.
42 CFR 482.43 outlines current discharge planning conditions of participation requirements.
Medical Records Requirements
IPF medical records must show the physician or NPP treatment level and intensity for each patient
they admit to the hospital, among other requirements detailed at 42 CFR 482.61.
Patients must be able to access their medical records when requested verbally or in writing, and the
hospital must quickly meet the patient’s request, detailed at 42 CFR 482.13.

Medicare & Mental Health Coverage MLN Booklet
Page 39 of 44 MLN1986542 July 2024
Medical Records Checklist: Inpatient Psychiatric Services
This inpatient psychiatric services medical records checklist reminds clinicians and sta of
required documentation.
Medical Record Content
□
Patient identication data, including inpatient legal status
□
Incoming patient history ndings and treatment plan
□
Patient provisional or admitting diagnosis, including intercurrent disease diagnosis and
psychiatric diagnosis
□
Sta or others signicantly involved clearly document inpatient admission reasons
□
Social service records must include:
□
Inpatient, family member, and other interviews
□
Home plans assessment
□
Family attitudes
□
Community resources
□
Contacts
□
Social history
□
If indicated, a completed and recorded neurological exam during the admission physical

Medicare & Mental Health Coverage MLN Booklet
Page 40 of 44 MLN1986542 July 2024
Psychiatric Evaluation
□
Completed within 60 hours of patient admission
□
Medical history
□
Mental status record
□
Admission illness onset and circumstances noted
□
Attitudes and behavior described
□
Estimated intellectual and memory functioning and orientation
□
Inpatient assets inventory, descriptive and not interpretive
Comprehensive Written Treatment Plan
□
Individual plan based on inpatient strengths and disabilities
□
Substantiated diagnosis
□
Short- and long-term goals
□
Specic treatment modalities used
□
Each treatment team member’s responsibilities
□
Adequate documentation justifying diagnosis, treatment, and completed rehabilitation activities
□
All active therapeutic inpatient treatment eorts documented
Recorded Progress
□
All physicians, psychologists, or other licensed independent practitioners record patient progress
□
Others signicantly involved in active treatment modalities, when appropriate
□
Determine the patient’s progress note frequency by condition; less than weekly during the rst
2 months and at least once per month thereafter
□
Progress notes must include treatment plan revision recommendations, when necessary
□
Progress notes must include a precise patient treatment plan progress assessment

Medicare & Mental Health Coverage MLN Booklet
Page 41 of 44 MLN1986542 July 2024
Discharge Plan
□
Discharge summary
□
Patient’s hospital stay recap
□
Recommended patient follow-up and aftercare
□
Patient discharge condition summary
*Discharge Planning Evaluation, Plan, and Summary
□
Does the hospital have a discharge planning process that applies to all hospital patients?
□
Early in the patient’s hospitalization, did you identify if they’re likely to suer adverse health
consequences if discharged without adequate discharge planning?
□
If yes, did you complete a discharge planning evaluation or was it requested by the
patient, their representative, or the physician?
□
Did an RN, a social worker, or another appropriately qualied sta member develop or
supervise the plan?
□
Did the evaluation include the patient’s post-hospital services need and their self-care capacity
or the possibility of returning to their pre-hospital environment?
□
Was the planning evaluation timely to allow appropriate post-hospital arrangements?
□
Does the patient’s medical record document the interaction of relaying discharge planning
evaluation results to them or their representative?
*Identies the newest discharge planning conditions of participation.

Medicare & Mental Health Coverage MLN Booklet
Page 42 of 44 MLN1986542 July 2024
*Standard Discharge Plan
□
Did an RN, a social worker, or another appropriately qualied sta member develop or
supervise discharge plan development if indicated in the evaluation?
□
If the evaluation showed no discharge plan nding, did the patient’s physician request it?
□
Did the hospital re-assess the patient’s discharge plan if factors aecting the patient’s
continuing care needs develop?
□
Did the hospital arrange to implement the patient’s discharge plan?
□
Did the patient, family, and interested persons get counseling to prepare them for
post-hospital care?
□
Did the hospital include a Medicare home health agency (HHA) discharge plan list (HHAs
must request that hospital list when available) and SNFs serving that geographic area where
the patient lives or, in the SNF’s case, in the requested geographic area?
□
Did you present that list to the patient only if they needed home health or post-hospital
extended care services indicated in the discharge planning evaluation?
□
If the patient was enrolled in a managed care organization, did the hospital indicate those
contracted managed care organization services?
□
Did you document in the medical record that you presented the HHA list to the patient?
□
Did the hospital inform the patient and family of their freedom to choose among participating
providers’ post-hospital care services and respect the patient’s and family’s preference (the
hospital must not specify or limit available, qualied providers)?
□
Did the hospital disclose any HHA or SNF nancial interest it may have with them?
*Transfer or Referral
□
If you transferred or referred a patient, did you provide follow-up or ancillary care medical
information to appropriate facilities, agencies, or outpatient services?
*Identies the newest discharge planning conditions of participation.

Medicare & Mental Health Coverage MLN Booklet
Page 43 of 44 MLN1986542 July 2024
Coverage Period
We cover IPF patient services in specialty facilities for 90 days per illness with a 60-day lifetime reserve
and 190 days of care in freestanding psychiatric hospitals (this 190-day limit doesn’t apply to certied
psychiatric units). The patient gets no further benets after using 190 days of psychiatric hospital care.
Under the IPF PPS, federal per diem rates include inpatient operating and capital-related costs
(including routine and ancillary services). We determine them by:
●
Geographic factors
●
Patient characteristics
●
Facility characteristics
IPFs get additional payments for:
●
Patients treated in IPFs with a qualifying emergency department
●
The number of ECT treatments provided
●
Outlier cases (cases with extraordinarily high costs)
The Medicare Benet Policy Manual, Chapter 2 has more information on how Medicare covers IPFs.
Same Day Billing Guidelines
Integrating mental health and SUD services addresses all patients’ needs whether they get care in a
traditional primary care setting or a specialty mental or SUD health care setting. Services include:
●
Mental health care services (we include substance use treatment)
●
Alcohol and substance use (other than tobacco) structured assessment and intervention services
(SBIRT services) billed under HCPCS codes:
●
G2011: Alcohol and/or substance (other than tobacco) misuse structured assessment (e.g.,
audit, dast), and brief intervention, 5-14 minutes
●
G0396: Alcohol and/or substance (other than tobacco) misuse structured assessment (e.g.,
audit, dast), and brief intervention 15 to 30 minutes
●
G0397: Alcohol and/or substance (other than tobacco)
misuse structured assessment (e.g., audit, dast), and
intervention, greater than 30 minutes
●
Primary health care services
Part B pays for reasonable and necessary integrated health care services provided on the same day,
to the same patient, by the same or dierent professionals in the same or dierent locations.
The Eligible Professionals section lists eligible Part B providers that may provide diagnostic and
therapeutic mental, psychoneurotic, personality disorder, and SBIRT treatment services allowed
under state law.
AUDIT: Alcohol Use Disorders
Identication Test
DAST: Drug Abuse Screen Test

Medicare & Mental Health Coverage MLN Booklet
Page 44 of 44 MLN1986542 July 2024
We cover medically reasonable and necessary services or supplies to treat the patient’s overall
diagnosis and condition or improve a malformed body part. Services must meet standards of good
medical diagnosis, direct care, and patient medical treatment condition practice and must not be
mainly for patient, provider, or supplier convenience.
Services must also meet specic National Coverage Determination and Local Coverage Determination
medical necessity criteria.
Every service billed must indicate the specic sign, symptom, or patient complaint requiring the
service. Although a provider may consider a service or test good medical practice, we don’t pay for
services without patient symptoms, complaints, or specic documentation.
We also pay for multiple mental health services for the same patient on the same day. However, we
don’t pay for inappropriate or duplicate services on the same day. If you have questions about local
or national policies that may prevent you from billing certain services, nd your MAC’s website.
Resources
●
CMS Behavioral Health Strategy
●
CMS Blog: Important New Changes to Improve Access to Behavioral Health in Medicare
●
CMS Opioid Treatment Programs
●
Marriage and Family Therapist & Mental Health Counselors
●
Marriage and Family Therapists (MFTs) and Mental Health Counselors (MHCs) Provider
Enrollment Frequently Asked Questions (FAQs)
●
Medicare Benet Policy Manual, Chapters 2, 6, and 15
●
Medicare Claims Processing Manual, Chapters 3 and 4
●
MLN Matters®: Provider Enrollment Changes to the Medicare Program Integrity Manual (MM13331)
●
Notices and Forms
●
Quality Improvement Organizations
●
SAMHSA: What is Mental Health?
View the Medicare Learning Network® Content Disclaimer and Department of Health & Human Services Disclosure.
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department
of Health & Human Services (HHS).
