
2023
National Veteran
Suicide Prevention
Annual Report
VA Suicide Prevention
Oce of Mental Health and Suicide Prevention
November 2023

2
Contents
Introduction 5
Anchors of Hope 5
A Call to Action for Each of You 6
Reviewing Veteran Suicide Within the Context of 2021 6
Key Findings 8
Need for a Whole-of-Nation Public Health Approach to Veteran Suicide Prevention: Themes for Action 10
Organization of Report 13
Part 1: Suicide Among Veterans, 2001–2021 14
Suicide Deaths 14
Average Number of Suicides Per Day 15
Suicide Rates 16
Suicide Rates, by Sex 17
Suicide Rates, by Age 18
Suicide Rates, by Sex and Age 19
Suicide Rates, by Race and Ethnicity 20
Suicide Rates in Year Following Military Separation 22
Method-Specific Suicide Rates 24
Method-Specific Suicide Rates, by Veteran Status and Sex 26
Method-Specific Suicide Rates, by Sex and Veteran status 26
Lethal Means Involved in Suicide Deaths 27
Comparing Suicide Mortality Among Veterans and Non-Veteran U.S. Adults 30
Veteran Leading Causes of Death 34
Years of Potential Life Lost 37
COVID-19 Pandemic: Suicide Surveillance 37

3
Review of Overall Veteran Suicide Data 37
Reflecting Back, Looking Forward: Laying the Foundation for Future
Courses of Action for Suicide Prevention for All Veterans 38
Promote Secure Firearm Storage for Veteran Suicide Prevention 38
Implement and Sustain Community Collaborations Focused Upon Community-Specific
Veteran Suicide Prevention Plans 40
Continue Expansion of Readily Accessible Crisis Intervention Services 42
Improve Tailoring of Prevention and Intervention Services to the Needs,
Issues, and Resources Unique to Veteran Subpopulations 44
Communication and Outreach 44
Community Prevention 44
Research and Innovation 45
Clinical Innovation 46
Part 2: Veterans with VHA or VBA Contact 47
Veterans Health Administration (VHA) Health Care 47
VHA Health Care Engagement, 2001–2021 47
Suicide Deaths 48
Suicide Rates 49
Marital Status 52
Mental Health and Substance Use Disorder Diagnoses 52
Homelessness 55
Veterans Justice Programs 55
Rurality 57
Gender Identity 57
VHA Priority Eligibility Groups 58
Veteran All-Cause Mortality, Overall and by VHA Engagement 61
Leading Causes of Death, for Recent Veteran VHA Users and Other Veterans 62
Recent Veteran VHA Users 62
Other Veterans 63
VA Community Care 64

4
Veterans, by Receipt of VHA and VBA Services 66
VBA Benefit Types Received, Percentage, Among Veterans with VBA Benefits, 2019–2021 68
Suicide Rates Among Veterans by Receipt of VBA or VHA Services 69
Suicide Decedents in 2021: Contacts with VHA and VBA 71
Suicide Decedents, VBA Contact 72
Suicide Decedents with Recent VBA Contact, VBA Services Received 72
Suicide Decedents, Recent Veteran VHA Users with Behavioral Health Autopsy Program Reviews 73
Reflecting Back, Looking Forward: Laying the Foundation for Future
Courses of Action for Suicide Prevention for VHA- and VBA-Engaged Veterans 74
Advance Suicide Prevention Meaningfully into Non-Clinical Support and
Intervention Services, Including Financial, Occupational, Legal and Social Domains 74
Increase Access to and Utilization of Mental Health Services Across a Full Continuum of Care 76
Integrate Suicide Prevention Within Medical Settings to Reach All Veterans 78
Conclusion 81
Appendix A: Brief Summary of 2021 VA Suicide Prevention Initiatives 83
Appendix B: Suicide Prevention Demonstration (Pilot) Projects, FY 2024 86

5
Introduction
This Department of Veterans Affairs (VA) “2023 National Veteran Suicide Prevention Annual Report” provides new
information regarding suicide mortality among Veterans and non-Veteran U.S. adults, from 2001 through 2021,
including the first full year of information since the onset of the COVID-19 pandemic, in March 2020. This annual report
of Veteran suicide mortality over time is a critical part of our public health approach to inform next steps in suicide
prevention across the Nation, reflecting on the lives lost and reviewing themes of action to move forward to prevent
suicide. In alignment with prior concerns about the potential for increases in suicide rates with the worldwide COVID-19
pandemic,
1,2
and consistent with trends for the overall U.S. population,
3
this report documents increases in suicide rates in
2021 for Veterans and non-Veteran U.S. adults. Overall reductions in suicide rates among U.S. adults in 2019 and 2020 were
not repeated in 2021. This may reflect a trend in which suicide rates are seen to initially remain stable or diminish during
emergencies and natural disasters, due to a collective “coming together,”
4
followed by increases in rates in ensuing years.
5,6
In 2021, 6,392 Veterans died by suicide, an increase of 114 suicides from 2020. When looking at increases in rates from
2020 to 2021, the age- and sex-adjusted suicide rate among Veterans increased by 11.6%, while the age- and sex-adjusted
suicide rate among non-Veteran U.S. adults increased by 4.5%. Veterans remain at elevated risk for suicide. These
numbers are more than statistics — they reflect Veterans’ lives prematurely ended, which continue to be grieved by
family members, loved ones and the Nation. One Veteran suicide is 1 too many. In this report we reflect on the context
of 2021 and the themes of data which will drive us towards further action for our work together in the mission of suicide
prevention. Our actions are built upon a foundation of hope, and we begin our review reflecting first upon these anchors
for our future work together.
Anchors of Hope
Hope is essential to life and hope serves an important role within suicide prevention efforts. Within the challenges faced
in 2021, key areas of hope emerged, including:
• From 2020 to 2021:
• Suicide rates fell by 8.1% for Veteran men aged 75-years-old and older.
• Among Recent Veteran Veterans Health Administration (VHA) Users
7
between ages 55- and 74-years-old, the
suicide rate fell by 2.2% overall (-0.6% for men, -24.9% for women).
• Among male Recent Veteran VHA Users, suicide rates fell by 1.9% for those aged 18- to 34-years-old.
1
Reger MA, Stanley IH, Joiner TE. 2020. Suicide Mortality and Coronavirus Disease 2019—A Perfect Storm? JAMA Psychiatry. 77(11), 1093-1094.
2
Banerjee D, Kosagisharaf JR, Rao TSS. 2021. ‘The Dual Pandemic’ of Suicide and COVID-19: A Biopsychosocial Narrative of Risks and Prevention.
Psychiatry Research. 295. https://doi.org/10.1016/j.psychres.2020.113577
3
Garnet MF, Curtin SC. 2023. Suicide Mortality in the U.S., 2001–2021. CDC National Center for Health Statistics, Data Brief 464.
4
These may have fragmented protective feelings of social integration that commonly follow elections. See: Classen TJ, Dunn RA. 2010. The Politics of
Hope and Despair: The Effect of Presidential Election Outcomes on Suicide Rates. Soc Sci Q. 91(3): 593–612.
5
Horney JA, Karaye IM, Abuabara A, Gearhart S, Grabich S, Perez-Patron M. 2020. The Impact of Natural Disasters on Suicide in the United States,
2003–2015. 42(5):328-334. doi: 10.1027/0227-5910/a000723.
6
Kolves K, Kolves KE, De Leo D. 2013. Natural Disasters and Suicidal Behaviours: A Systematic Literature Review. 146(1):1-14.
7
Recent Veteran VHA Users are defined as Veterans who were alive at the start of the year and who received inpatient or outpatient care from VHA
providers in the year or prior year.

6
• Among male Recent Veteran VHA Users, suicide rates fell by 8.6% for those aged 75-years-old and older.
• Among male Veterans not in VHA care who were aged 75-years-old and older, the suicide rate fell by 7.8%.
• From 2001 to 2021:
• The suicide rate among Recent Veteran VHA Users with mental health or substance use disorder diagnoses
fell from 77.8 per 100,000 to 58.2 per 100,000 in 2021.
• Suicide rates fell for Recent Veteran VHA Users with diagnoses of sedative use disorder (-40.4%), depression
(-32.9%), posttraumatic stress disorder (-27.6%) and anxiety (-26.9%).
• Recent Veteran VHA Users rates grew more slowly across 20 years when compared to rates of Veterans
without Recent VHA use. From 2001 to 2021, age-adjusted suicide rates rose 24.5% for male Veterans with
Recent VHA use and 62.6% for male Veterans without Recent VHA use. Age-adjusted suicide rates rose 87.1%
for female Veterans with recent VHA use and 93.7% for female Veterans without Recent VHA use.
• From 2011–2012 to 2020–2021, the suicide rate among Veterans in VHA care with diagnoses related to gender
identity fell from 267.9 per 100,000 person-years to 84.6 per 100,000 person-years.
Hope is the foundation for action in suicide prevention. As we reflect on these anchors of hope, we move to review the
larger context of 2021, laying out a pathway for our course of action for Veteran suicide prevention.
A Call to Action for Each of You
Reviewing Veteran Suicide Within the Context of 2021
This report reflects the complexity of suicide inherent in the Veteran population, and the United States as a whole, in the
context of 2021. Suicide prevention entails numerous and complex risks and protective factors across individual,
relational, community and societal levels.
8
Within 2021, Veterans and the entire U.S. population directly faced health and
mortality effects of the COVID-19 pandemic.
9
Weekly U.S. COVID-19 deaths peaked, ebbed, and climbed anew across
2021. By year’s end, over 837,000 Americans had died from COVID-19 since the pandemic began, including over 469,000
Americans who perished from COVID-19 in 2021 alone.
10
In 2020 and 2021, COVID-19 was the third leading cause of death
in the U.S., both overall
11,12
and for Veterans. There were 52,538 Veteran deaths from COVID-19 in 2020, and 60,356 in 2021.
Veteran age- and sex-adjusted all-cause mortality rates were 13.7% higher in 2020–2021 than in 2017–2019.
13
In addition
8
Reed J, Quinlan K, Labre M, Brummett S, Caine ED. 2021. The Colorado National Collaborative: A Public Health Approach to Suicide Prevention. Prev
Med. 152(Pt 1):106501.
9
In September 2021, COVID-19 became the deadliest respiratory pandemic in U.S. history. Lovelace B. CNBC. Covid is Officially America’s Deadliest
Pandemic as U.S. Fatalities Surpass 1918 Flu Estimates. 9/20/2021. https://www.cnbc.com/2021/09/20/covid-is-americas-deadliest-pandemic-as-us-
fatalities-near-1918-flu-estimates.html (Accessed 7/2/2023).
10
https://covid.cdc.gov/covid-data-tracker/#trends_weeklydeaths_select_00 (Accessed 7/7/2023). Also, in 2021 alone, there were over 2.5 million
COVID-19 hospitalizations in the United States, reaching over 3.6 million from the start of the pandemic through 12/31/2021. https://covid.cdc.gov/
covid-data-tracker/#trends_cumulativehospitalizations_select_00. Despite having substantial prevention resources, U.S. mortality outcomes were
poor relative to other countries. See: Ledesma JR, Isaac CR, Dowell SF, Blazes DL, Essix GV, Budeski K, Bell J, Nuzzo JB. 2023. Evaluation of the Global
Health Security Index as a Predictor of COVID-19 Excess Mortality Standardised for Under-Reporting and Age Structure. BMJ Global Health. doi:
10.1136/bmjgh-2023-012203.
11
Murphy SL, Kochanek KD, Xu J, Arias E. Mortality in the United States, 2020. NCHS Data Brief, 427. Hyattsville, MD: National Center for Health
Statistics. 2021. https://stacks.cdc.gov/view/cdc/112079/cdc_112079_DS2.pdf (Accessed 6/25/2023).
12
Xu J, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2021. NCHS Data Brief, 456. Hyattsville, MD: National Center for Health
Statistics. 2022. https://www.cdc.gov/nchs/data/databriefs/db456.pdf (Accessed 6/25/2023).
13
Assessed by comparing the average of the annual rates.

7
to these losses, the Nation faced greater financial strain,
14
housing
instability,
15
anxiety and depression levels,
16
barriers to health care and
increased firearms availability, all of which are associated with heightened
suicide risk.
17,18
With the increased purchasing of firearms noted in 2020
and 2021, those who purchased and owned firearms were more likely than
non-firearm owners to report experiencing thoughts of suicide,
19
and
first-time firearm purchasers were more likely to report suicidal ideation.
20
In 2021, potential further distress was experienced by many as a result of
social conflict and political violence.
21
Veteran distress increased from fall
2019 to fall and winter 2020, with evidence of the highest increases in
distress among Veterans aged 18- to- 44-years-old and among women
Veterans. These increases in reported distress were associated with
increasing socioeconomic concerns, greater problematic alcohol use and
decreased community integration.
22
During the COVID-19 pandemic, Veterans were found to experience more mental
health concerns than non-Veterans. A systematic review of 23 studies found increases in the prevalence rates of alcohol
use, anxiety, depression, posttraumatic stress disorder, stress, loneliness and suicidal ideation. The results of this
systematic review found key risk factors to include pandemic-related stress, family relationship strain, lack of social
support, financial concerns and preexisting mental health disorders.
23
14
Data from the 2021 Survey of Household Economics and Decisionmaking indicate that: 1) for both Veterans and non-Veteran U.S. adults,
financial hardships (e.g., lower income, greater debt, residence in economically challenged areas, lack of a rainy day fund) were associated with
poorer physical health, and 2) Veterans more commonly reported financial challenges involving credit card debt and overdraft fees. Personal
communication. 8/7/2023. E. Elbogen, VA National Veterans Financial Resource Center.
15
Elbogen EB, Lanier M, Blakey SM, Wagner HR, Tsai J. 2021. Suicidal Ideation and Thoughts of Self-Harm During the COVID-19 Pandemic: The Role of
COVID-19-Related Stress, Social Isolation, and Financial Strain. Depression Anxiety. 38:739-748.
16
Fischer IC, Na PJ, Harpaz-Rotem I, Krystal JH, Pietrzak RH. 2023. Characterization of Mental Health in US Veterans Before, During, and 2 Years After
the Onset of the COVID-19 Pandemic. JAMA Network Open. 6(2):e230463.
17
Monteith LL, Miller CN, Polzer E, Holliday R, Hoffmire CA, Iglesias CD, Schneider AL, Brenner LA, Simonetti JA. 2023. “Feel the need to prepare
for Armageddon even though I do not believe it will happen”: Women Veterans’ Firearm Beliefs and Behaviors During the COVID-19 Pandemic,
Associations with Military Sexual Assault and Posttraumatic Stress Disorder Symptoms. PLOS ONE. 18(2):e0280431. As noted by Monteith and
colleagues, “… it is unclear how women Veterans’ firearm beliefs and behaviors might have changed following 2020, nor whether the pandemic
itself or other relevant societal events (e.g., racial justice protests, political violence) were the predominant drivers of perceptions among any
individual participant.”
18
Miller M, Zhang W, Azrael D. 2022. Firearm Purchasing During the COVID-19 Pandemic: Results From the 2021 National Firearms Survey. Annals of
Internal Medicine. 175(2):219-225.
19
Also referred to as suicidal ideation.
20
Anestis MD, Bandel SL, Bond AE. 2021. The Association of Suicidal Ideation with Firearm Purchasing During a Firearm Purchasing Surge. JAMA
Network Open. 4(10):e2132111. doi: 10.1001/jamanetworkopen.2021.32111.
21
Of note, January 2021 included a single week with the most U.S. COVID-19 deaths of the entire pandemic (25,974 deaths in the week of 1/9/2021
https://covid.cdc.gov/covid-data-tracker/#trends_weeklydeaths_select_00); the invasion and looting of the U.S. Capitol by over 2,000 individuals;
impeachment of the former president for inciting insurrection; and the largest increase in the number of firearm purchases in the period from
1/1/2020-4/26/2021 (Miller M, Zhang W, Azrael D. 2022. Firearm Purchasing During the COVID-19 Pandemic: Results From the 2021 National
Firearms Survey. Annals of Internal Medicine. 175(2):149-304.) In summer 2021, the U.S. withdrawal from Afghanistan raised additional concerns
as a potential stressor for Veterans. In 2021, conflicting perspectives regarding pandemic responses, social justice, election integrity, and political
violence were in plain view.
22
Fischer IC, Na PJ, Harpaz-Rotem I, Krystal JH, Pietrzak RH. 2023. Characterization of Mental Health in US Veterans Before, During, and 2 Years After
the Onset of the COVID-19 Pandemic. JAMA Network Open. 6(2):e230463.
23
Li S, Huang S, Hu S, Lai J. Psychological Consequences Among Veterans During the COVID-19 Pandemic: A Scoping Review. Psychiatry Research.
2023 Jun;324:115229.
Heavily Impacted Groups in 2021
• Women Veterans
• American Indian or Alaska Native
Veterans
• VHA Veterans
• Homeless Veterans
• Justice-Involved Veterans

8
Simultaneously, VA was moving forward key suicide prevention initiatives in collaboration with other federal agencies,
Veterans Service Organizations (VSO), community partners, non-profit organizations, and others across the Nation
to address the rising needs outlined in 2021. These included the following: Veterans Crisis Line (VCL) 988 preparation;
Suicide Prevention 2.0 (SP 2.0) clinical telehealth expansion; SP 2.0’s Community-Based Intervention for Suicide
Prevention (CBI-SP) growth; Staff Sergeant Parker Gordon Fox Suicide Prevention Grant Program (SSG Fox SPGP) and
Mission Daybreak development; expansion of special population suicide prevention efforts; and firearm lethal means
safety (LMS) efforts (see Appendix A for a summary). Yet, more work remained for full implementation to occur in each of
the areas.
The context of 2021 challenges for the Nation, and for Veterans specifically, is critical to consider as we review highlights
of this year’s data and outline key courses of action moving forward. Veteran suicide deaths increased by 114 from 2020,
with 6,392 individual Veteran lives lost to suicide in 2021. It is also important to reflect on the subpopulations of Veterans
to identify the unique impacts and potential courses of action to address suicide prevention moving forward. From 2020
to 2021, suicide rates fell by 8.1% for Veteran men aged 75-years-old and older, which may reflect a Nation more fully
focused on connection and support for its more vulnerable individuals during the pandemic. Unfortunately, Veteran
suicide rates increased for other age groups. The increase in Veteran suicides seen in 2021, compared to 2020, was
particularly seen in women Veterans, for whom there was a 24.1% increase in the age-adjusted suicide rate, compared to
an increase of 6.3% among male Veterans. Similarly, when looking at race/ethnicity, we saw the largest increase in rate
among American Indian or Alaska Native Veterans. Among Veterans in VHA care, those with legal system involvement
were at increased risk of suicide-related behavior.
24
The suicide rate for recipients of VA Justice Program services was
10.2% higher in 2021 than in 2020. Additionally, in 2021, the unadjusted suicide rate among Recent Veteran VHA Users
with indications of homelessness was 38.2% higher than in 2020. Finally, 48.7% of all 6,392 Veterans who died by suicide
in 2021 had received either VHA or Veterans Benefits Administration (VBA) services in 2020 or 2021,
25
while 51.3%
had received neither VHA nor VBA services. This underscores the need to continue to reach outside of VA into local
communities and neighborhoods to connect with all Veterans as part of our national approach to end Veteran suicide.
Key Findings
• In 2021, suicide was the 13th-leading cause of death for Veterans overall, and the second-leading cause of death
among Veterans under age 45-years-old.
• There were 6,392 Veteran suicide deaths in 2021. This was 114 more than in 2020.
• In 2021, there were 6,042 suicide deaths among Veteran men and 350 suicide deaths among Veteran women.
• The unadjusted rate of suicide in 2021 among U.S. Veterans was 33.9 per 100,000, up from 32.6 per 100,000 in 2020.
• In 2021, unadjusted suicide rates were highest among Veterans between ages 18- and 34-years-old, followed by
those aged 35- to 54-years-old.
• In 2021, the unadjusted suicide rate was 46.3 per 100,000 for American Indian or Alaska Native Veterans; 36.3 per
100,000 for White Veterans; 31.6 per 100,000 for Asian, Native Hawaiian or Pacific Islander Veterans; 17.4 per 100,000
for Black or African American Veterans; and 6.7 per 100,000 for Veterans of multiple races.
• In 2021, the unadjusted suicide rate was 19.7 per 100,000 for Veterans with Hispanic ethnicity, and it was 33.4 per
100,000 for other Veterans.
24
Palframan KM, Blue-Howells, J, Clark SC, McCarthy JF. 2020. Veterans Justice Programs: Assessing Population Risks for Suicide Deaths and
Attempts. Suicide and Life-Threatening Behavior. 50(4):792-804.
25
Of the 6,392 Veterans who died from suicide in 2021, 38.1% received VHA services in 2020 or 2021 and 34.0% received VBA services in 2020 or 2021.

9
• Suicide was the fourth-leading cause of years of potential life lost (YPLL)
26
in 2019, prior to the COVID-19 pandemic;
in 2020 and 2021, suicide was the fifth-leading cause of YPLL.
• Among U.S. adults who died from suicide in 2021, firearms were more commonly involved among Veteran deaths
(72.2%) than among non-Veteran deaths (52.2%).
• Within the overall unadjusted suicide rate for Veterans in 2021 (33.9 per 100,000), its largest component was firearm
suicide mortality (24.5 per 100,000), followed by suffocation suicide mortality (5.0 per 100,000), poisoning suicide
mortality (2.7 per 100,000) and suicide involving other methods (1.8 per 100,000).
• Among Veterans, in each year, firearm suicide and suffocation suicide mortality rates were greater for men than for
women, while the poisoning suicide mortality rate was lower for men than for women.
• Among U.S. adult men and women, rates of firearm and of poisoning suicide mortality were greater for Veterans
than for non-Veterans, and differentials in rates by Veteran status were particularly high among women (e.g., the
firearm suicide rate among Veteran women was 281.1% higher than that of non-Veteran women, while the firearm
suicide rate among Veteran men was 62.4% higher than for non-Veteran men).
• Consistent with higher-complexity medical and psychosocial needs among Veterans who seek VHA care, rates in
2021 were higher among Recent Veteran VHA Users than for Other Veterans for all-cause mortality and for leading
causes of death, including heart disease, cancer, COVID-19, unintentional injury, and suicide.
• Age- and sex-adjusted suicide rates were higher among Recent Veteran VHA Users than for Other Veterans. In
comparison with Veterans not receiving VHA care, Veterans receiving VHA care have a higher risk with being more
likely to have lower annual incomes; poorer self-reported health status;
27
more chronic medical conditions
28
and
self-reported disability due to physical or mental health factors;
29
greater depression and anxiety;
30
and greater
reporting of trauma, lifetime psychopathology and current suicidality.
31
These differences may help to explain the
greater suicide rates among Recent Veteran VHA Users compared to Other Veterans.
• However, Recent Veteran VHA Users rates grew more slowly across 20 years when compared to rates of Veterans
without Recent VHA use. From 2001 to 2021, age-adjusted suicide rates rose 24.5% for male Veterans with Recent
VHA use and 62.6% for male Veterans without Recent VHA use. Age-adjusted suicide rates rose 87.1% for female
Veterans with recent VHA use and 93.7% for female Veterans without Recent VHA use.
• Among Recent Veteran VHA Users experiencing homelessness, the suicide rate in 2021 (112.9 per 100,000) was the
highest observed over the period 2001–2021, after increasing 38.2% since 2020.
• The suicide rate in 2021 among Recent Veteran VHA Users who received Justice Program services was also the
highest over this period (151.0 per 100,000) after a 10.2% increase since 2020.
26
Years of potential life lost is a measure of premature death which expresses the number of years that would have been lived if premature death
had not occurred. It is calculated as the difference between age at death and 75 (approximate life expectancy). If individuals live to or beyond age
75, YPLL is equal to 0. See: CDC. 1986. Premature Mortality in the United States: Public Health Issues in the Use of Years of Potential Life Lost. MMWR,
12/19/1986, 35(2S):1s-11s. https://www.cdc.gov/mmwr/preview/mmwrhtml/00001773.htm (Accessed 7/4/2023).
27
Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. 2000. Are Patients at Veterans Affairs Medical Centers Sicker? A Comparative Analysis of Health
Status and Medical Resource Use. Arch Intern Med. 160:3252-3257.
28
Dursa EK, Barth SK, Bossarte RM, Schneiderman AI. 2016. Demographic, Military, and Health Characteristics of VA Health Care Users and Nonusers
Who Served in or During Operation Enduring Freedom or Operation Iraqi Freedom, 2009–2011. Public Health Reports. 131(6):839-843.
29
Nelson KM, Starkebaum GA, Reiber GE. 2007. Veterans Using and Uninsured Veterans Not Using Veterans Affairs (VA)
Health Care. Public Health Rep. 122:934-100.
30
Fink DS, Stohl M, Mannes ZL, Shmulewitz D, Wall M, Gutkind S, Olfson M, Gradus J, Keyhani S, Maynard C, Keyes KM, Sherman S, Martins S, Saxon
AJ, Hasin DS. 2022. Comparing Mental and Physical Health of U.S. Veterans by VA Healthcare Use: Implications for Generalizability of Research in the
VA Electronic Health Records. BMC Health Services Research. 22:1500 https://doi.org/10.1186/s12913-022-08899-y
31
Meffert BN, Morabito DM, Sawicki DA, Hausman C, Southwick SM, Pietrzak RH, Heinz AJ. 2019. U.S. Veterans Who Do and Do Not Utilize VA Health
Care Services: Demographic, Military, Medical, and Psychosocial Characteristics. Primary Care Companion CNS Disorders. 21(1):doi:10.4088/
PCC.18m02350.

10
• Among VHA-enrolled Recent Veteran VHA Users in 2021, the suicide rate was highest for those in Priority Eligibility
Group 5, which includes income-based eligibility (57.1 per 100,000).
• In 2020 and 2021, suicide rates were highest for Veterans who received any Community Care services, followed by
Veterans who received any VHA direct care, and suicide rates were lowest among Veterans who did not receive
either Community Care or VHA direct care.
32
• In 2020 and 2021, suicide rates were greater among Veterans who received VA Community Care services and did not
receive VHA direct care services than among Veterans who received VHA direct care services and did not receive VA
Community Care services.
• Overall, 48.7% of Veterans who died from suicide in 2021 had received VHA or VBA services in 2020 or 2021, while
51.3% of Veterans in 2021 did not.
• For the overall Veteran population in 2021, 47.2% received some VHA or VBA services in 2020 or 2021, while 52.8% of
the overall Veteran population in 2021 did not.
• In 2021, suicide rates were highest among Veterans who only received VHA services, followed by those who
received both VHA and VBA services, then those who received neither VHA nor VBA services. Suicide rates were
lowest among Veterans who received VBA services and did not receive VHA services.
• Among Recent Veteran VHA Users whose suicide deaths occurred in 2019–2021 and were reported to VHA Suicide
Prevention teams, VA Behavioral Health Autopsy Program data indicated that the most frequently identified risk
factors were: pain (55.9%), sleep problems (51.7%), increased health problems (40.7%), relationship problems (33.7%),
recent declines in physical ability (33.0%), hopelessness (30.6%) and unsecured firearms in the home (28.8%).
Need for a Whole-of-Nation Public Health Approach to Veteran Suicide Prevention:
Themes for Action
The significant and unprecedented challenges this country faced in 2021 fuel this report’s continued call to action related
to a whole-of-government and whole-of-Nation approach to suicide prevention. Suicide is a complex problem requiring
a full public health approach involving community prevention and clinical intervention. VA services are a critical part
of this public health approach, as the data from this report highlights. The data across 20 years reveals that Veterans
engaged in VHA care have shown a less sharp rise in suicide rates, underscoring the importance of VHA care. Over 20
years of Veteran suicide data also reveal a substantial reduction in suicide rates, specifically for Recent Veteran VHA Users
with mental health or substance use disorder diagnoses (77.8 per 100,000 in 2001 to 58.2 per 100,000 in 2021), falling
32.9% for Veterans with depression, 27.6% for those with posttraumatic stress disorder, 26.9% for those with anxiety and
40.4% for those with sedative use disorder. Comparing Veterans with Recent VHA use to other Veterans, we also find
notable trends. While overall rates of Veteran suicide rose across the 20 years, age-adjusted suicide rates rose 24.5% for
male Veterans with Recent VHA use compared to 62.6% for male Veterans without Recent VHA use. While less notable
for women Veterans, the age-adjusted suicide rates rose 87.1% for female Veterans with Recent VHA use and 93.7% for
female Veterans without Recent VHA use. Likewise, when looking more specifically across 2020 and 2021, we find the
greatest increase in unadjusted rates for Veterans who were neither engaged with VHA nor with VBA. From 2020 to
2021, there were also notable decreases for particular subpopulations of Veterans with Recent VHA use, including those
between ages 55- and 74-years-old (overall suicide rate -2.2%, -0.6% for men, -24.9% for women), males between ages
18- and 34-years-old (overall suicide rate -1.9%) and males aged 75-years-old and older (overall suicide rate -8.6%). These
findings underscore the importance of continuing to expand access to and engagement of Veterans in VHA and VBA
services, as over 50% of Veterans who died by suicide in 2021 had not been engaged in either service.
Yet, in order to address the complex interweaving of individual, relational, community and societal risks, VA must
continue to fully engage with other federal agencies; public-private partnerships; government at the local, state and
32
As noted above, Veterans receiving VHA care show evidence of higher risk with being more likely to have lower annual incomes, poorer self-
reported health status, more chronic medical conditions, and self-reported disability due to physical or mental health factors, greater depression
and anxiety, and greater reporting of trauma, lifetime psychopathology, and current suicidality.

11
national levels; VSOs; and local communities to reach all Veterans to support the implementation of a full public health
approach, as outlined in the White House Strategy Reducing Military and Veteran Suicide (2021)
33
and VA’s National
Strategy for Preventing Veteran Suicide (2018).
34
These guiding documents have been operationalized through SP 2.0;
Suicide Prevention Now initiative (SP Now); new laws, including the 2020 Commander John Scott Hannon Veterans Mental
Health Care Improvement Act; the Veterans Comprehensive Prevention, Access to Care and Treatment Act (COMPACT)
of 2020; the National Suicide Hotline Designation Act of 2020; and emerging innovations combined with research and
program evaluation. As 2021 has again shown, this public health approach must include both community-based prevention
and clinical interventions to reduce suicide in the Veteran population. As we reflect on the core of what we learned about
Veteran suicide in 2021, 7 themes emerge for our call to action (see summary listing and description below).
While no one solution can address the complexity of all factors involved in suicide, the data clearly outlines that significant
reductions in Veteran suicide will not occur without meaningful focused effort to address Veteran firearm suicide. While
we vigorously pursue enhanced policies, research, and programs to effectively address the broader socioecological and
individual risk and protective factors which speak to “why” a Veteran may consider suicide, we must address directly the
“how” of Veteran suicide. It is inescapable that the “how” in 72% of Veteran suicide deaths is firearm compared to 52% of
non-Veteran U.S. adult suicides. We therefore begin our call to action with a focus on secure firearm storage.
1. Promote secure firearm storage for Veteran suicide prevention. Firearm ownership and storage practices vary
among Veterans.
35
One in 3 Veteran firearm owners store at least 1 firearm unlocked and loaded. This unsafe storage
practice is more frequent among Veteran firearm owners who seek VHA care (38.0%) than among other Veterans
who own firearms (31.9%).
36
As seen across years of Veteran suicide data, Veteran suicide deaths disproportionately
involve firearms; Veteran suicide rates exceed those of non-Veterans; and differentials in suicide rates by Veteran
status are greater for women than for men. Promoting secure storage of firearms has been found to reduce suicide
— this is not about taking away firearms but about promoting time and space during a time of crisis.
37
2. Implement and sustain community collaborations focused upon community-specific Veteran suicide
prevention plans. Over 60% of Veterans who died by suicide in 2021 were not seen in VHA in 2020 or 2021, and
over 50% had received neither VHA nor VBA services. In order to reach all Veterans, we must continue to expand
our work in the community through the SP 2.0 Community Based Intervention (CBI) Program. This includes the joint
VA and Substance Abuse and Mental Health Services Administration (SAMHSA) Governor’s Challenge to Prevent
Suicide Among Service members, Veterans, and their Families, which encompasses all 50 states, 5 territories and
work in over 1,700 local community coalitions. This also includes the SSG Fox SPGP awarding $52.5 million to 80
community-based organizations in 43 states, the District of Columbia and American Samoa in fiscal year (FY) 2023.
33
White House: Reducing Military and Veteran Suicide: Advancing a Comprehensive, Cross-Sector, Evidence-Informed Public Health Strategy. 2021.
https://www.whitehouse.gov/wp-content/uploads/2021/11/Military-and-Veteran-Suicide-Prevention-Strategy.pdf
34
Department of Veterans Affairs (2018). National Strategy for Preventing Veteran Suicide.
https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-
Veterans-Suicide.pdf
35
Combining reports from Azrael et al., 2017, and Cleveland et al., 2017, and VetPop estimates of the 2015 populations of Veteran men and women,
we estimate that in 2015 household firearm ownership among Veteran men was 62.3% higher than for non-Veteran men, and household firearm
ownership among Veteran women was 106.6% higher than for non-Veteran women.
36
Simonetti JA, Azrael D, Rowhani-Rahbar A, Miller M. 2018. Firearm Storage Practices Among American Veterans. American Journal of Preventative
Medicine. 55(4):445-454.
37
Mann JJ, Michel CA, Auerbach RP. 2021. Improving Suicide Prevention Through Evidence-Based Strategies: A Systematic Review. American Journal
of Psychiatry. 178(7):611-624.

12
3. Continue expansion of readily accessible crisis
intervention services. The Nation saw a reduction of
access to mental health services initially during the
COVID-19 pandemic.
38,39
Veterans desired access that was
not in-person and available whenever they needed it
40
and VHA care rapidly expanded remote care services
delivery.
41
Continued expansion of access to 24/7/365
services through the VCL 988 expansion and through
COMPACT Act implementation paved the way for more
emergency services for Veterans in acute suicidal crisis to
be provided at no cost, whether enrolled in VA or not.
42
4. Improve tailoring of prevention and intervention
services to the needs, issues, and resources unique
to Veteran subpopulations. Creating culturally
sensitive and responsive interventions to meet each
population’s needs will be required to address what 2021
revealed to us, with growing rates in American Indian/
Alaska Native Veteran populations, younger Veterans,
transitioning Service member populations, women
Veterans and more, as seen in the data for 2021.A
one-size-fits-all Veteran suicide prevention strategy will
not be effective in meeting the needs of the diverse
population of Veterans.
5. Advance suicide prevention meaningfully into
non-clinical support and intervention services,
including financial, occupational, legal, and social
domains. Suicide risk factors include issues outside
of mental health and require meaningful upstream
interventions across the Nation, as denoted in the White
House Strategy Reducing Military and Veteran Suicide
(2021).
43
Impacts related to homelessness and legal issues
were seen for Veterans in 2021, as outlined above. A
whole-of-Nation approach for upstream interventions in
employment, housing, legal support, and financial strain
is needed to address Veteran suicide prevention.
38
Zhang J, Boden M, Trafton J. 2022. Mental Health Treatment and the Role of Tele-Mental Health at the Veterans Health Administration During the
COVID-19 Pandemic.Psychological Services. 19(2):375-385.https://doi.org/10.1037/ser0000530
39
Behavioral Health: Patient Access, Provider Claims Payment, and the Effects of the COVID-19 Pandemic. GAO-21-437R. Mar 31, 2021.
40
Goetter EM, Iaccarino MA, Tanev KS, Furbish KE, Xu B, Faust KA. 2022. Telemental Health Uptake in an Outpatient Clinic for Veterans During the
COVID-19 Pandemic and Assessment of Patient and Provider Attitudes.Professional Psychology: Research and Practice. 53(2):151-159.https://doi.
org/10.1037/pro0000437
41
Cornwell B, Szymanski BR, McCarthy JF. 2021. Impact of the COVID-19 Pandemic on Primary Care-Mental Health Integration Services in the VA
Health System. Psychiatric Services. 72(8):972-973.
42
The calls for action encompass work that has been ongoing since 2021 and needs for ongoing development. Thus, COMPACT and 988 are included
here, both of which had work underway in 2021.
43
White House: Reducing Military and Veteran Suicide: Advancing a Comprehensive, Cross-Sector, Evidence- informed Public Health Strategy. 2021.
https://www.whitehouse.gov/wp-content/uploads/2021/11/Military-and-Veteran-Suicide-Prevention-Strategy.pdf
Call to Action: 7 Themes
Promote rearm secure storage for
Veteran suicide prevention.
Implement and sustain community
collaborations focused upon community-specic
Veteran suicide prevention plans.
Continue expansion of readily accessible
crisis intervention services.
Improve tailoring of prevention and intervention
services to the needs, issues, and resources
unique to Veteran subpopulations.
Advance suicide prevention meaningfully into
non-clinical support and intervention services,
including nancial, occupational, legal,
and social domains.
Increase access to and utilization of mental
health across a full continuum of care.
Integrate suicide prevention within medical
settings to reach all Veterans.
13
6. Increase access to and utilization of mental health services across a full continuum of care. The COVID-19
pandemic saw increased distress in the Veteran population
44
with initial decreases in utilization of mental health
services, while telemental health services expanded. During the pandemic, weekly patient encounters at VHA
decreased by 3% for ongoing suicide attempt care, while new treatment initiation for suicide attempts decreased
30%.
45
Making access as easy as possible to a continuum of evidence-based mental health treatments is an
important part of the public health approach to suicide prevention.
7. Integrate suicide prevention within medical settings to reach all Veterans. Our data again showed that a
significant percentage of VHA Veterans who died by suicide did not have a VHA mental health or substance use
disorder diagnosis. We need to creatively address the needs of those at risk who may never seek mental health
services and who may have other risk factors outside of mental health (e.g., pain, cancer, sleep disturbance) through
expansion of suicide screening, assessment, and safety planning into all medical settings, within VHA and within
community care.
Organization of Report
This year’s report is organized in alignment with the call to action, as Veteran suicide prevention will take all of us.
After an initial summary of key findings, the report is organized into two overarching sections:
1) The overall Veteran population; and
2) Veterans with Recent VHA or VBA engagement.
Specifically, the data is broken out in the following manner to assist ongoing efforts, together with you, to
reduce Veteran suicide:
• Suicide among Veterans, overall and compared to non-Veteran U.S. adults, including patterns of Veteran mortality,
including the initial 2 calendar years of the COVID-19 pandemic.
• Suicide among Veteran subpopulations, including:
• By VHA engagement, including:
- Veterans who received VHA health care
46
in the year or prior year, who in this report are described as
“Recent Veteran VHA Users.”
- Veterans who were not Recent Veteran VHA Users, who in this report are described as “Other Veterans.”
• By VBA engagement
- Overall and by receipt of categories of VBA benefits.
After each of these sections, the report will reflect on relevant research that has served to inform next steps, where VA
is moving next steps forward, and specific actions that VA and each of us across the Nation can take to join together in
Veteran suicide prevention. The detailed analyses of suicide mortality over time and across Veteran subgroups can help
us together to advance suicide prevention initiatives across both the individual and societal levels.
44
Fischer IC, Na PJ, Harpaz-Rotem I, Krystal JH, Pietrzak RH. 2023. Characterization of Mental Health in US Veterans Before, During, and 2 Years After
the Onset of the COVID-19 Pandemic. JAMA Network Open. 6(2):e230463.
45
Zhang J, Boden M, Trafton J. 2022. Mental Health Treatment and the Role of Tele-Mental Health at the Veterans Health Administration During the
COVID-19 Pandemic. Psychological Services. 19(2):375-385.
46
VHA health care receipt is here defined as having at least 1 VHA inpatient or outpatient utilization record.

14
Part 1: Suicide Among Veterans, 2001–2021
Suicide Deaths
• In 2021, there were 46,412 suicides among U.S. adults. These included 6,392 suicides among Veterans
47
(114 more
than in 2020) and 40,020 among non-Veterans (2,000 more than in 2020).
• Among Veterans, non-Veteran adults, and U.S. adults overall, the number and rate of suicide deaths increased from
2020 to 2021 (Figure 1 and Figure 3).
Figure 1: Suicide Deaths Among Veterans and Non-Veteran U.S. Adults, by Year, 2001–2021
47
For this report, Veterans were defined as persons who had been activated for federal military service and were not currently serving at the time of
death. For more information see the accompanying 2023 National Veteran Suicide Prevention Annual Report Methods Summary.
Veterans Non-Veteran Adults
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
45,000
40,000
35,000
30,000
25,000
20,000
15,000
10,000
5,000
0
2020 2021
6,000
6,392
23,580
40,020
Number of Suicides

15
Figure 2 details variation in the number of Veteran suicides, by year from 2001 to 2021.
Figure 2: Veteran Suicide Deaths, 2001–2021
Average Number of Suicides Per Day
48
• In 2021, there were on average 127.2 suicides per day among U.S. adults, including 17.5 per day among Veterans and
109.6 per day among non-Veteran adults.
• Among all U.S. adults, including Veterans, the average number of suicides per day rose from 81.0 per day in 2001 to
127.2 in 2021. The average number per day among U.S. adults was highest in 2018 (127.4 per day).
• The average number of Veteran suicides per day rose from 16.4 in 2001 to 17.5 in 2021. For U.S. adults, the average
number of suicides per day was highest in 2018 for Veterans (18.4 per day). Of the on-average 17.5 Veteran suicides
per day in 2021, approximately 38.1% (6.7 per day) were among Recent Veteran VHA Users
49
and 61.9% (10.8 per day)
were among Other Veterans.
48
Decreases in the size of the Veteran population and increases in the size of the U.S. population over this period limit interpretation of these
statistics. Rates of suicide, stratified by group, are the appropriate for understanding changes in Veteran and non-Veteran populations. These are
included elsewhere in this report and in the accompanying data appendix.
49
Consistent with prior reports, Recent Veteran VHA Users were defined as Veterans who received inpatient or outpatient care health care (in person
or via telehealth) at a VHA facility in the year of interest or the prior year (here, 2021 or 2020). Health care received from non-VHA facilities, including
such care that was funded by VA (i.e., community care) was not included.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
7,000
6,800
6,600
6,400
6,200
6,000
5,800
5,600
2020 2021
6,000
6,142
6,008 6,004
6,035
6,126
6,249
6,567 6,545
6,519
6,447
6,441
6,501
6,645
6,467
6,481
6,616
6,686
6,392
6,278
6,718
Number of Suicides

16
Suicide Rates
From 2001 to 2021, the Veteran population decreased by 27.0%, from 25.8 million to 18.8 million. During this same
timeframe, the non-Veteran U.S. adult population increased by 28.4%, from 186.5 million to 239.5 million. In this context, it is
important to assess suicide mortality rates, which convey the incidence of suicide relative to the size of the population.
Unadjusted suicide rates represent the number of suicide deaths relative to the population’s time at risk of being
observed with a suicide death.
50
Rates are reported as suicides per 100,000.
51
Direct adjusted rates are used for
comparisons while adjusting for population differences, such as age and sex distributions.
52
To describe the burden of
suicide in a given population and period, we use unadjusted rates. To compare rates across populations or periods, we
use direct adjusted rates.
53
• The unadjusted suicide rate for Veterans was 23.3 per 100,000 in 2001 and 33.9 per 100,000 in 2021. For non-Veteran
U.S. adults, the suicide rate was 12.6 per 100,000 in 2001 and 16.7 per 100,000 in 2021.
• In 2021, Veterans between ages 18- and 34-years old had an unadjusted suicide rate of 49.6 per 100,000, while the
rate was 35.5 per 100,000 for those between ages 35- and 54-years old; 29.9 per 100,000 for those between ages 55-
and 74-years old; and 32.1 per 100,000 for those aged 75-years-old and older.
• In 2021, the unadjusted suicide rate of Veteran men was 35.9 per 100,000 (3.5% higher than in 2020) and it was 17.5
per 100,000 for Veteran women (23.7% higher than in 2020).
• Age- and sex-adjusted suicide rates from 2001 to 2021 are presented in Figure 3 for Veterans and non-Veteran U.S.
adults, by year. The difference in age- and sex-adjusted rates was greatest in 2021, when the age- and sex-adjusted
rate for Veterans was 71.8% greater than that of non-Veteran adults.
• Bivariate comparisons indicated that Veteran age- and sex-adjusted suicide rates were significantly greater in 2021
than in 2019 or 2020.
50
Risk time is measured using mid-year population estimates when individuals’ exact risk times were unavailable. It was calculated exactly for
analyses of subgroups of Veterans with recent VHA care.
51
For the Veteran population, risk time was assessed using the mid-year population estimate, as detailed in the accompanying methods summary.
When risk time was assessed per individual level risk-time information, we included “per 100,000 person-years.”
52
Unadjusted rates communicate the magnitude of suicide mortality in a given population in a time period. Suicide risks differ across age and sex
categories. Consequently, if groups differ in these characteristics, then that variation may account for some of the differences in unadjusted rates.
Adjusted rates translate the unadjusted rate for a population into a measure of what the rate would be if the compared populations had the same
distributions of the demographic factors that are adjusted for. Per standard practice, adjusted rates are calibrated to the demographic distribution
of the U.S. adult population in 2000. Calculating adjusted rates (e.g., age-adjusted or age- and sex-adjusted rates) enhances rate comparisons by
adjusting for population demographic differences. Notably, the Veteran and non-Veteran adult populations differ by age and sex, with Veterans
being on average older and more male.
53
The interpretation of adjusted rates is somewhat technical. They represent the level of suicide mortality that we would see in the population and
time period if the population had the same demographic distribution of a standard population, at least in terms of the adjustment variable(s).
Consistent with current practice, in this report adjusted rates use the U.S. adult population in 2000 as the standard population. Unadjusted rates
are presented when adjustment was not possible due to small numbers within strata. Use of the direct method and the standard U.S. population of
2000 for adjustment are consistent with CDC reporting (Garnet MF, Curtin SC. 2023. Suicide Mortality in the United States, 2001–2021. CDC NCHS,
Data Brief 464. Klein RJ, Schoenborn CA. Age Adjustment Using the 2000 Projected U.S. population. Healthy People 2000 Statistical Notes, no. 20.
Hyattsville, Maryland: NCHS. January 2001).

17
Figure 3: Age- and Sex-Adjusted Suicide Rate, Veterans and Non-Veteran U.S. Adults, 2001–2021
Suicide Rates, by Sex
• Figure 4 presents age-adjusted suicide rates for Veteran men and for Veteran women, by year, 2001–2021. For
Veteran men and Veteran women, rates were highest in 2021.
• From 2020 to 2021, the age-adjusted suicide rate increased 6.3% among Veteran men and 24.1% among Veteran
women. From 2020 to 2021, the age-adjusted suicide rate increased 4.9% among non-Veteran men and 2.6% among
non-Veteran women.
• In 2021, the age-adjusted suicide rate of Veteran men was 43.4% greater than that of non-Veteran U.S. adult
men, and the age-adjusted suicide rate of Veteran women was 166.1% higher than that of non-Veteran U.S.
adult women.
54
54
For men and for women, differentials in adjusted rates by Veteran status were highest in 2021.
Veterans Non-Veteran Adults
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
35
30
25
20
15
10
5
0
2020 2021
Age- and Sex-Adjusted Rate per 100,000

18
Figure 4: Age-Adjusted Suicide Rate, Male and Female Veterans, 2001–2021
Suicide Rates, by Age
Figure 5 presents unadjusted suicide rates for Veterans, by age categories and year, 2001–2021.
From 2020 to 2021, the suicide rate among Veterans aged 18- to 34-years-old increased by 7.1%; the rate for Veterans
aged 35- to 54-years-old rose by 10.7%; the rate for Veterans aged 55- to 74-years old rose by 7.4%; and for Veterans aged
75-years-old and older, the suicide rate fell by 8.0%.
Figure 5: Unadjusted Suicide Rate, Veterans, by Age Group, 2001–2021
Male Veterans Female Veterans
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
45
40
35
30
25
20
15
10
5
0
2020 2021
Age-Adjusted Rate per 100,000
18-34 35-54 55-74 75+
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
60
50
40
30
20
10
0
2020 2021
Rate per 100,000

19
Suicide Rates, by Sex and Age
Figures 6 and 7 present suicide rates
55
for Veteran men and women, by age categories and year, 2001–2021.
• In 2021, suicide rates were highest among Veterans between ages 18- and 34-years-old (55.4 per 100,000 among
Veteran men aged 18- to 34-years-old, and 24.8 per 100,000 among Veteran women aged 18- to 34-years-old).
• Suicide rates among male Veterans aged 75-years-old and older decreased by 8.1% from 2020 to 2021, while rates
for all other groups increased.
Figure 6: Unadjusted Suicide Rate, Male Veterans, by Age Group, 2001–2021
Figure 7: Unadjusted Suicide Rate, Female Veterans, by Age Group,
56
2001–2021
55
As rates are specific to age- and sex-subgroups, adjustment was not applicable.
56
Due to the small number of deaths among older age groups of female Veterans, the 55- to 74-years-old and 75-years-old and older age groups are
combined, for reporting purposes.
18-34 35-54 55-74 75+
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
60
50
40
30
20
10
0
2020 2021
Rate per 100,000
18-34 35-54 55+
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
60
50
40
30
20
10
0
2020 2021
Rate per 100,000

20
Suicide Rates, by Race and Ethnicity
Figure 8 presents unadjusted Veteran suicide rates, by race.
57
• In 2021, the suicide rate was 36.3 per 100,000 for White Veterans; 31.6 per 100,000 for Asian, Native Hawaiian or
Pacific Islander Veterans; 46.3 per 100,000 for American Indian or Alaska Native Veterans; 17.4 per 100,000 for Black
or African American Veterans; and 6.7 per 100,000 for Veterans of multiple races.
• In 2021, the highest suicide rate was among American Indian or Alaska Native Veterans and the lowest rate was
among Veterans of multiple races.
• Among the U.S. adult general population in 2021, which includes Veteran and non-Veteran adults and uses more
detailed race categories, unadjusted suicide rates were also highest among those who were American Indian or
Alaska Native, followed by those who were White, Native Hawaiian or other Pacific Islander, multiple races, Black or
African American and Asian.
58
Figure 8: Unadjusted Suicide Rate, Veterans, by Race,
59
2001–2021
57
It was not possible to generate adjusted rates, due to data constraints. Consequently, differences in rates may in part be due to population
differences in demographic factors that are independently associated with suicide risk.
58
Note that the U.S. adult population includes both Veteran and non-Veteran U.S. adults. Suicide rates for adults in the U.S. general population are
derived from CDC WONDER. For more information on CDC WONDER, see: https://wonder.cdc.gov/ucd-icd10-expanded.html. Unadjusted suicide
rates among U.S. adults in 2021 were as follows: American Indian or Alaska Native: 21.7 per 100,000; White: 20.1 per 100,000; Native Hawaiian or
other Pacific Islander: 14.0 per 100,000; multiple races: 12.0 per 100,000; Black or African American: 10.6 per 100,000; and Asian: 8.3 per 100,000.
59
Categories presented are mutually exclusive. The availability of information regarding race demographics for the overall Veteran population
is limited, sometimes combining the Asian, Native Hawaiian, and Pacific Islander race categories. To provide the most complete information
available, we present information using this combined category. The percentage of Veteran suicide deaths missing race information was 7.8% in
2001, 7.7% in 2002, 7.7% in 2003, 8.0% in 2004, 7.5% in 2005, 6.9% in 2006, 7.4% in 2007, 11.0% in 2008, 13.7% in 2009, 2.9% in 2010, 2.3% in 2011,
2.5% in 2012, 2.6% in 2013, 3.0% in 2014, 2.7% in 2015, 2.9% in 2016, 2.5% in 2017, 2.8% in 2018, 3.4% in 2019, 4.7% in 2020 and 4.2% in 2021.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
50
45
40
35
30
25
20
15
10
5
0
2020 2021
Rate per 100,000
White
Black or African
American
American Indian
or Alaska Native
Asian, Native Hawaiian,
or Pacific Islander
Multiple Race

21
Figure 9 presents unadjusted suicide rates for Veterans, by Hispanic ethnicity.
60
• From 2020 to 2021, suicide rates increased 0.5% for Hispanic Veterans and 4.7% for non-Hispanic Veterans. By
comparison, in the U.S. adult general population, suicide rates increased by 6.1% among individuals with Hispanic
ethnicity and by 3.7% among other adults.
Figure 9: Unadjusted Suicide Rate, Veterans, by Hispanic Ethnicity, 2001–2021
60
It was not possible to generate adjusted rates, due to data constraints. Consequently, differences in rates may in part be due to population
differences in demographic factors that are independently associated with suicide risk.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
40
35
30
25
20
15
10
5
0
2020 2021
Rate per 100,000
Hispanic Non-Hispanic
13.3
19.7
20.4
33.4

22
Suicide Rates in Year Following Military Separation
Figure 10 presents the unadjusted suicide rate per 100,000 over 12 months following Veterans’ separation from active
military service, by year of separation, 2010–2020.
61,62
Suicide rates in the 12 months following separations ranged from 34.8 per 100,000, for Veterans who separated in 2010,
to 48.9 per 100,000, for Veterans who separated in 2019.
Figure 10: Unadjusted Suicide Rate, 12 Months Following Separation from Active Military Service, by Year
of Separation, 2010–2020
61
Twelve-month suicide mortality rates are reported for cohorts of Veterans who separated from military service in the years 2010 through 2020.
Separations were identified using VA/Department of Defense Identity Repository (VADIR) data. Reporting is not included for years prior to 2010
due to data constraints. Given small cell sizes, it was not possible to calculate adjusted rates. The 12-month observation period for the most recent
cohort (separations in calendar year 2020) extended into 2021, using the most current available mortality data. Review of 95% confidence intervals
(not shown) indicated that these were overlapping for each year, indicating no statistical differences in rates over this period.
62
In 2010, there were 226,928 Veterans with most recent separations from active military service, and there were 195,385 in 2020. For Veterans who
separated in 2010, 16.8% were female and the median age at separation was 26. For those who separated in 2020, 17.4% were female and the
median age at separation was 27. There were 79 and 93 Veteran suicides within 12 months of military separations in 2010 and 2020, respectively.
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
60
50
40
30
20
10
0
2020
Rate per 100,000 Person-Years
Year of Separation
34.8
42.8
39.4
42.1
41.7
35.6
35.8
46.7
48.1
48.9
47.6

23
Figure 11 presents unadjusted suicide rates in the 12 months following separation, by year of separation and service branch.
For the most recent separation cohort, who separated from active military service in 2020, suicide rates over the
following 12 months were highest among those who separated from the Marines Corps (80.9 per 100,000), followed by
the Navy (50.1 per 100,000) and Army (46.1 per 100,000).
63
Figure 11: Unadjusted Suicide Rate, 12 Months Following Separation from Active Military Service, by
Branch of Service and Year of Separation, 2010–2020
64
63
Not presented for Veterans who separated from the Air Force in 2020, as there were fewer than 10 suicide deaths.
64
Rates are suppressed if there were fewer than 10 suicide deaths, with dotted lines connecting non-suppressed data points. The dotted lines
represent suppressed rates and should not be interpreted as estimated rates.
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
90
80
70
60
50
40
30
20
10
0
2020
Rate per 100,000
Year of Separation
Army Air Force Navy Marines

24
Method-Specific Suicide Rates
Figure 12 presents method-specific
65
suicide rates among Veterans, by year, 2001–2021, and the percentage change in
rates from 2001 to 2021.
• In each year, Veteran firearm suicide rates exceeded those of all other categories.
• Changes in Veteran method-specific suicide rates are listed below:
2001 to 2021 2019 to 2020 2020 to 2021
Firearm suicide rate +58.3% +1.4% +5.5%
Poisoning suicide rate (-13.4%) +0.4% (-1.1%)
Suocation suicide rate +55.6% (-10.8%) +5.0%
Other methods suicide rate +18.2% +6.3% (-5.9%)
Figure 12: Unadjusted Method-Specific Suicide Rate, Veterans, 2001–2021, and Change from 2001 to 2021
Similar to patterns for Veterans, among non-Veteran U.S. adults firearm suicide mortality rates exceeded all other
method-specific suicide rates in each year.
66
For non-Veteran U.S. adults, there was also a decrease from 2001 to 2021 in
poisoning suicide mortality rates (-11.2%) and increases in rates of firearm suicide mortality (+30.9%), suffocation suicide
mortality (+70.7%) and suicide involving other methods (+39.8%).
67
65
Methods were assessed from death certificate data per ICD-10 codes X72-X74 for firearm, X60-X69 for poisoning (including intentional overdose)
and X70 for suffocation (including strangulation). “Other Means” (U03, X71, X75-X84, Y87.0) included cutting/ piercing, drowning, falls, fire/flame,
other land transport, being struck by/against and other specified or unspecified injury.
66
Results not shown.
67
Firearm suicide mortality accounted for a larger portion of the overall Veteran suicide rate in 2001 and 2021 (66.5% and 72.2%, respectively) than
for non-Veterans (52.7% and 52.2%, respectively).
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
30
25
20
15
10
5
0
2020 2021
Rate per 100,000
+58.3
-13.4
+55.6
+18.2
Percentage Change,
2001 to 2021
Firearm Poisoning Suffocation Other

25
Figures 13 and 14 show method-specific suicide rates for male Veterans and female Veterans, respectively.
Figure 13: Unadjusted Method-Specific Suicide Rate, Male Veterans, 2001–2021, and Change from 2001 to 2021
Figure 14: Unadjusted Method-Specific Suicide Rate, Female Veterans, 2001–2021, and Change from 2001
to 2021
68
68
Rates are suppressed for female Veterans, Other Means, for 2002 and 2013. Dashed lines are for presentation purposes and do not represent
estimated rates.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
30
25
20
15
10
5
0
2020 2021
Rate per 100,000
+61.8
-17.6
+54.0
+21.7
Percentage Change,
2001 to 2021
Firearm Poisoning Suffocation Other
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
30
25
20
15
10
5
0
2020 2021
Rate per 100,000
+157.7
+249.5
+2.2
-8.6
Percentage Change,
2001 to 2021
Firearm Poisoning Suffocation Other

26
Method-Specific Suicide Rates, by Veteran Status and Sex
Here we compare method-specific rates of Veteran men and women, and we compare rates of non-Veteran men and
women.
69
As indicated below, method-specific suicide rates varied by sex for Veterans and non-Veterans. The magnitude
of this variation differed by Veteran status.
• Among Veterans, in each year, firearm suicide and suffocation suicide mortality rates were higher for men than for
women, while poisoning suicide mortality rates were lower for men than for women. In 2021:
• Firearm suicide rate: 190.1% higher for Veteran men than for Veteran women
• Suffocation suicide rate: 50.9% higher for Veteran men than for Veteran women
• Poisoning suicide rate: 40.4% lower for Veteran men than for Veteran women
• Among non-Veteran U.S. adults, in each year, all method-specific suicide rates were greater for men than for
women. In 2021:
• Firearm suicide rate: 580.7% higher for non-Veteran men than for non-Veteran women
• Suffocation suicide rate: 313.0% higher for non-Veteran men than for non-Veteran women
• Poisoning suicide rate: 9.6% higher for non-Veteran men than for non-Veteran women
• Poisoning suicide mortality rates were lower for Veteran men than for Veteran women, and they were higher for
non-Veteran men than for non-Veteran women.
Method-Specific Suicide Rates, by Sex and Veteran status
Here we compare method-specific rates of male Veterans to those of male non-Veterans, and we compare method-
specific rates of female Veterans to those of female non-Veterans.
70,71
As indicated below, method-specific suicide rates
varied by Veteran status, for both men and women. The magnitude of this variation differed by sex.
• Among men, in each year, 2001–2021, firearm suicide mortality and poisoning suicide mortality rates were higher,
and suffocation mortality rates were lower, for Veteran men than for non-Veteran men. In 2021:
• Firearm suicide rate: 62.4% higher for Veteran men than for non-Veteran men
• Poisoning suicide rate: 14.3% higher for Veteran men than for non-Veteran men
• Suffocation suicide rate: 31.3% lower for Veteran men than for non-Veteran men
• Among women, in each year, 2001–2021, firearm suicide mortality and poisoning suicide mortality rates were higher
for Veteran women than for non-Veteran women. In 2021:
• Firearm suicide rate: 281.1% higher for Veteran women than for non-Veteran women
• Poisoning suicide rate: 110.1% higher for Veteran women than for non-Veteran women
• Among women, the suffocation suicide rate in 2021 was 88.0% higher for Veteran women than for non-
Veteran women.
72
69
Due to small cell sizes, it was not possible to provide age-adjusted method-specific rates.
70
Due to small cell sizes, it was not possible to provide age-adjusted method-specific rates.
71
Compared to non-Veteran adults, Veterans are more likely to own firearms. Estimates derived from 2015 National Firearm Survey reports and
VetPop data suggest that in 2015 firearm ownership was approximately 62% higher for Veteran men than for non-Veteran men, and it was
approximately 107% higher for Veteran women than for non-Veteran women.
72
This direction and scale of this differential ranged from 2006, when Veteran women had a 13.7% lower rate of suffocation suicide than non-Veteran
women, to 2021, when Veteran women had an 88.0% higher suffocation suicide rate than non-Veteran women.

27
Lethal Means Involved in Suicide Deaths
Table 1 provides information on lethal means, or methods, involved in suicide deaths of Veterans and non-Veteran U.S.
adults in 2021 and a measure of change compared to suicides in 2001.
• Overall and by sex, suicide deaths among Veterans were more likely to involve firearms than suicide deaths among
non-Veteran U.S. adults. For example, firearms were involved in 73.4% of suicide deaths in 2021 among Veteran
men, compared to 57.2% of suicide deaths among non-Veteran men; and firearms were involved in 51.7% of suicides
by Veteran women in 2021, compared to 34.6% of non-Veteran women.
• Among Veteran suicide deaths in 2021, relative to those in 2001, there were increases in the percentage involving
firearms (+5.7%) and suffocation (+0.9%) and decreases for poisoning (-5.4%) and other means (-1.2%).
• For suicide deaths of non-Veteran U.S. adults, there were increases from 2001 to 2021 in the percentage involving
suffocation (+6.1%) and other means (+0.5%) and decreases in the percentage involving firearms (-0.5%) and
poisoning (-6.0%).
72%
Firearm
Suicide
5.7%
1 in 3
of Veteran suicides
were by firearm in 2021.
Veteran firearm suicides
from 2001 to 2021
increased by
Firearm suicide rate among
Veteran men was
62.4% higher
than for non-Veteran
men in 2021.
Firearm suicide rate among
Veteran women was
281.1%
higher
than non-Veteran
women in 2021. There was a
14.7% increase in Veteran
women firearm suicide deaths
from 2001
–
2021.
Firearm ownership is
more prevalent
among Veterans (45%)
than non-Veterans (19%).
Veteran firearm owners store
at least one firearm
unlocked and loaded.
.

28
Table 1: Suicide Deaths, Methods Involved, 2021 and Difference From 2001, by Veteran Status, Sex and
Age Groups
73
Veterans
Non-Veteran
U.S. Adults
Veteran
Men
Non-Veteran
Men
Veteran
Women
Non-Veteran
Women
2021 Change 2021 Change 2021 Change 2021 Change 2021 Change 2021 Change
All Ages
Firearms 72.2% +5.7% 52.2% -0.5% 73.4% +6.1% 57.2% -0.8% 51.7% +14.7% 34.6% -0.9%
Poisoning 7.8% -5.4% 12.4% -6.0% 6.9% -5.5% 7.7% -4.7% 23.7% -19.2% 28.8% -9.2%
Suocation 14.9% +0.9% 26.8% +6.1% 14.6% +0.5% 26.9% +4.5% 19.7% +9.3% 26.8% +11.1%
Other 5.2% -1.2% 8.6% +0.5% 5.2% -1.1% 8.3% +1.0% 4.9% -4.9% 9.8% -1.0%
Ages 18–34
Firearms 66.2% +5.3% 49.7% -1.9% 68.0% +5.9% 53.9% -0.8% 49.4% +12.7% 31.9% -3.9%
Poisoning 5.9% -5.4% 8.9% -3.8% 4.6% -5.5% 6.2% -3.1% 18.8% -17.9% 20.9% -9.5%
Suocation 22.7% +0.6% 32.5% +4.0% 22.0% -0.5% 31.4% +2.2% 29.4% -- 36.8% +12.7%
Other 5.2% -0.5% 8.9% +1.6% 5.4% +0.2% 8.6% +1.7% -- -- 10.4% +0.7%
Ages 35–54
Firearms 62.1% +7.7% 46.5% -0.1% 63.3% +8.2% 50.1% -1.8% 49.7% +10.4% 34.9% +2.3%
Poisoning 9.0% -10.0% 13.4% -11.4% 7.7% -10.2% 8.7% -8.8% 23.5% -22.3% 28.5% -15.6%
Suocation 23.2% +3.8% 31.5% +11.6% 23.3% +3.5% 32.6% +10.1% 21.5% -- 28.0% +14.9%
Other 5.7% -1.4% 8.6% -0.1% 5.7% -1.4% 8.6% +0.5% -- -- 8.7% -1.5%
Ages 55–74
Firearms 72.7% -3.2% 56.8% -6.2% 73.5% -2.8% 63.8% -7.4% 55.3% -- 36.5% -5.4%
Poisoning 8.9% -1.1% 15.6% -1.1% 7.9% -1.8% 9.0% -0.5% 30.1% -- 34.9% -0.5%
Suocation 12.4% +4.0% 18.6% +6.6% 12.6% +4.2% 18.7% +6.4% -- -- 18.3% +6.8%
Other 6.0% +0.3% 9.0% +0.8% 6.0% +0.4% 8.5% +1.5% -- -- 10.3% -0.9%
Ages 75+
Firearms 86.5% +5.1% 73.5% +4.8% 86.6% +4.9% 81.8% +3.3% -- -- 36.4% +0.4%
Poisoning 6.1% -0.3% 11.8% +1.6% 6.1% -0.4% 6.0% +0.7% -- -- 38.4% +11.1%
Suocation 4.0% -2.0% 9.1% -4.0% 4.1% -1.8% 7.8% -3.2% -- -- 14.9% -5.6%
Other 3.3% -2.8% 5.6% -2.3% 3.3% -2.7% 4.5% -0.9% -- -- 10.3% -5.9%
73
“Change” is the absolute difference comparing the percentage of suicide deaths in 2021 to the percentage of suicide deaths in 2001. Percentages
and differences are not presented when based on fewer than 10 deaths, indicated by “--”.
29
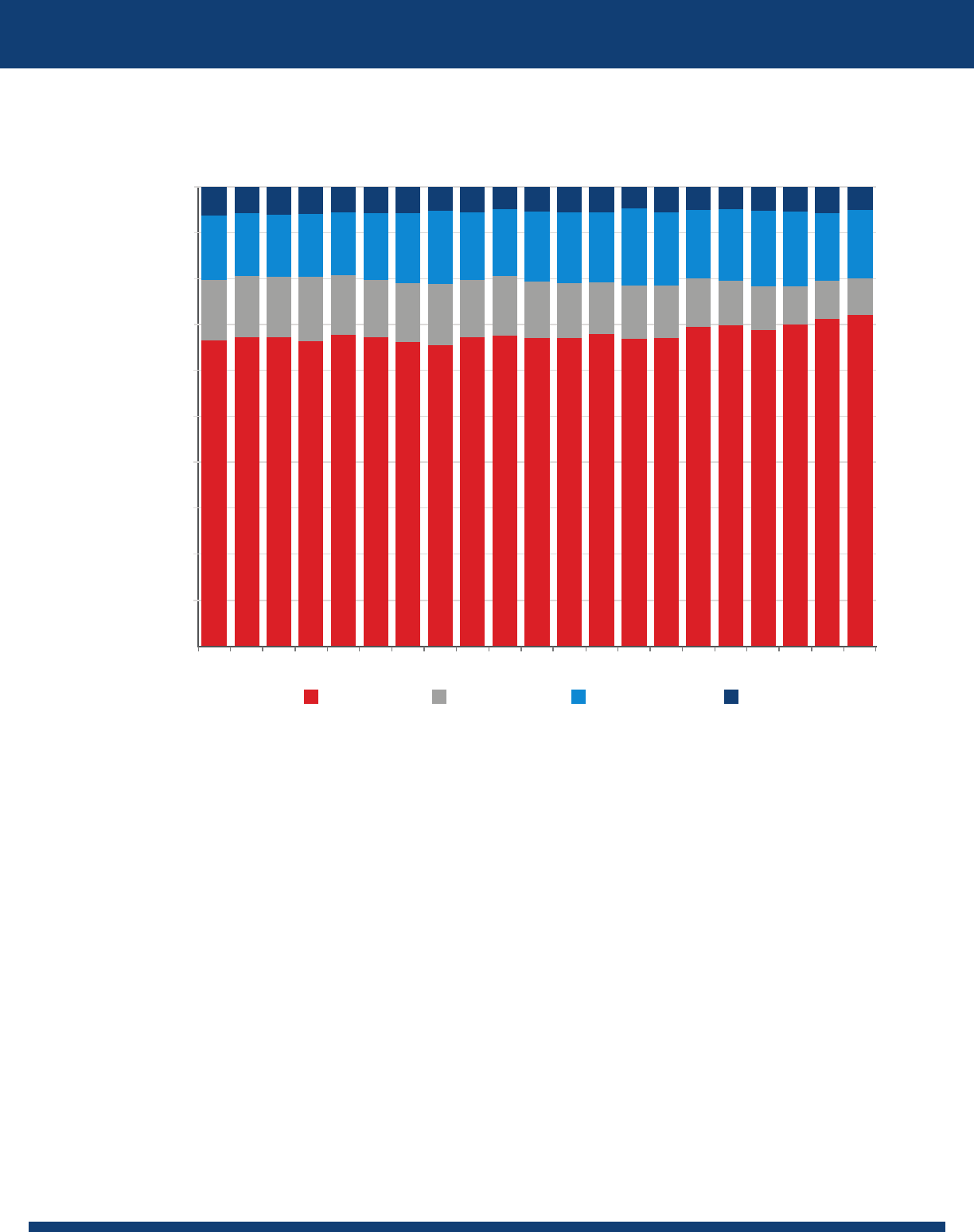
Figure 15 presents the distribution of methods involved in Veteran suicide deaths, from 2001–2021.
Figure 15: Methods Involved, Percentage, Veteran Suicide Deaths, 2001–2021
• From 2020 to 2021, among Veteran suicide deaths, the involvement of firearms and suffocation increased from
71.3% to 72.2% and 14.8% to 14.9%, respectively, while the involvement of poisoning and other methods decreased,
from 8.3% to 7.8% and from 5.7% to 5.2%, respectively.
• In 2021, firearms were involved in 73.4% of suicides by male Veterans, up from 72.3% in 2020, and in 51.7% of
suicides by female Veterans, up from 48.6% in 2020.
• The distribution of methods involved in suicides by non-Veteran U.S. adults changed from 2020 to 2021.
Involvement of firearms increased from 50.2% to 52.2%, while poisoning and suffocation decreased, from 12.9% to
12.4% and from 28.5% to 26.8%, respectively.
• Considering trends from 2019, prior to the first year of the COVID-19 pandemic, from 2019 to 2021, among Veteran
suicide deaths, the involvement of firearms increased from 70.0% to 72.2%, while the involvement of poisoning,
suffocation and other methods decreased, from 8.2% to 7.8%, 16.5% to 14.9% and 5.4% to 5.2%, respectively. Among
non-Veteran U.S. adults from 2019 to 2021, involvement of firearms increased from 47.6% to 52.2%, while poisoning,
suffocation, and other methods decreased, from 13.9% to 12.4%, 29.7% to 26.8% and 8.7% to 8.6%, respectively.
Firearm Poisoning Suffocation Other
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
Percent
6.4
5.9
5.2
5.7
5.4
5.2
5.0
5.2
5.6
4.8
5.55.6
5.4
5.0
5.6
5.3
5.75.8
5.5
5.9
6.2
13.9
13.6
14.9
14.8
16.5
16.6
15.5
14.8
16.0
16.7
15.4
15.4
15.4
14.5
14.7
15.9
15.2
14.5
13.7
13.8
13.5
13.2
13.3
7.8
8.3
8.2
9.3
9.7
10.5
11.4
11.6
11.1
11.9
12.2
13.0
12.6
13.4
12.9
12.4
13.1
14.0
13.1
66.5
67.3
72.2
71.3
70.0
68.9
69.9
69.6
67.1
66.9
68.0
67.267.1
67.5
67.2
65.4
66.1
67.2
67.7
66.3
67.3
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%

30
Comparing Suicide Mortality Among Veterans and Non-Veteran U.S. Adults
Efforts to understand Veteran suicide include comparisons of suicide statistics for Veterans and non-Veteran U.S. adults.
Here, we consider suicide measures as resources for comparisons, and we discuss findings.
• Counts of suicide deaths. In 2021, there were 6,392 suicides among Veterans and 40,020 among non-Veteran
U.S. adults.
• Limitation: These data points tell us the actual number of suicides that occurred; however, they are not
comparable because they do not account for the size of the populations, which differed substantially. In 2021,
there were 18.8 million Veterans and 239.5 million non-Veteran U.S. adults.
• Unadjusted suicide rates. Also known as crude rates, these measure the annual number of suicide deaths per
100,000 people in the population of interest. In 2021, the unadjusted suicide rate for Veterans was 33.9 per 100,000,
and for non-Veteran U.S. adults, 16.7 per 100,000. Unadjusted suicide rates summarize the number of suicides
relative to the size of the population, for the year specified.
• Limitation: They do not account for population differences in factors that may be related to suicide risk, such
as sex and age. The sex and age distributions of the Veteran and non-Veteran U.S. adult populations differ
substantially. For example, in 2021, the Veteran population included a higher proportion of men (89.4%) than
the non-Veteran adult population (45.9%). This difference matters for comparisons because, for example,
among U.S. adults, suicide rates in 2021 were 4 times greater for men than for women. To better understand
suicide patterns related to Veteran status, rather than the demographic characteristics of individuals who
become Veterans,
74
it is important to account for population differences.
This report employs two approaches for comparing suicide rates across populations and time periods.
75
• Compare unadjusted rates for subgroups. The first and most informative approach
76
is to compare unadjusted
suicide rates for Veterans and non-Veterans in specific demographic subgroups (or strata), such as men aged 18- to
34-years-old. The Data Appendix that accompanies this report
77
provides rate information stratified by age and sex
for Veterans and non-Veteran U.S. adults.
• Note: This approach offers as many comparisons as the number of subgroups and time periods examined; it
does not yield a single overall comparison measure.
• Compare adjusted rates for Veterans and non-Veterans. The second approach is to generate a summary
measure of rate differences that adjusts for population demographic differences. For example, Figure 3 presents
age- and sex-adjusted suicide rates for Veterans and non-Veteran U.S. adults. These were generated using direct
adjustment.
78
Specifically, we calculated what the overall suicide rates would be for Veterans and for non-Veteran
U.S. adults in each year if their age- and sex-specific suicide rates occurred in a population with the distribution of
a standard reference population. Following scientific recommendations and Department of Health and Human
74
Griffin BA, Grimm GE, Smart R, Ramchand R, Jaycox LH, Ayer L, Leidy EN, Davenport S, Schell TL, Morral AR. Comparing the Army’s Suicide Rate to
the General U.S. Population: Identifying Suitable Characteristics, Data Sources, and Analytic Approaches. Santa Monica, CA: RAND Corporation,
2020. https://www.rand.org/pubs/research_reports/RR3025.html
75
Even within a defined population, population characteristics may change over time. For example, from 2001 to 2021 the percentage of Veterans
who were male decreased from 93.7% to 89.4%.
76
Anderson RN, Rosenberg HM. 1998. Age Standardization of Death Rates: Implementation of the Year 2000 Standard. CDC National Vital Statistics
Reports. 47(3):1-17.
77
The Data Appendix is available here: https://www.mentalhealth.va.gov/about/data-reporting/suicide-prevention-data.asp
78
Curtin LR, Klein RJ. 1995. Direct Standardization (Age-Adjusted Death Rates). CDC/National Center for Health Statistics. DHHS Publication No. (PHS)
95-1237. https://www.cdc.gov/nchs/data/statnt/statnt06rv.pdf

31
Services policy,
79
this report uses the standard 2000 U.S. adult population as the reference population.
80
We
then created overall adjusted rates for the two populations, with each standardized to the same demographic
distribution. The adjusted rates can then be compared. For example, in 2021, the age- and sex-adjusted rate for
Veterans was 71.8% greater than that of non-Veteran adults.
• Note: Use of direct adjusted rates aligns with reporting by other federal agencies and facilitates comparisons
with other populations. They provide a consistent metric for comparisons; however, their interpretation is not
as straightforward as for unadjusted rates. Essentially, they enable consistent “what if” comparisons across
populations and time periods. For each, they tell us what the overall suicide rate would be if the population
of interest had the demographic distribution of the standard 2000 U.S. adult population. They are useful only
for comparisons and not for measuring absolute magnitude.
81,82
Indirect adjustment offers yet another method for comparing suicide mortality.
• Compare the number of Veteran suicide deaths to the number that would have occurred if the Veteran
population had the same age- and sex-subgroup-specific suicide rates as the non-Veteran population.
Indirect adjustment involves applying the subgroup-specific suicide rates of one population (e.g., non-Veteran U.S.
adults) to the demographic distribution of the population of interest (e.g., Veterans) in order to estimate the ratio of
the number of deaths that would occur if the strata-specific rates of the first population occurred in a population
with the demographic distribution of the second. The ratio of the number of deaths that were actually observed
in the second population (e.g., Veterans) to the number that would be expected if the second population had the
subgroup-specific rates of the first population is called a Standardized Mortality Ratio (SMR). Ratios greater than 1.0
indicate increased mortality in the second population; ratios less than 1.0 indicate decreased mortality.
• Note: Applying indirect adjustment, analyses evaluated the observed number of Veteran suicides in 2021
relative to the number that would have been observed if the Veteran population had the age- and sex-
specific suicide rates of the non-Veteran U.S. adult population. The resulting SMR was 1.124.
83
This indicates
that the number of Veteran suicide deaths in 2021 was 12.4% higher than what would be observed if the
Veteran population had the age- and sex-specific suicide rates of the non-Veteran U.S. adult population.
79
Anderson RN, Rosenberg HM. 1998. Age Standardization of Death Rates: Implementation of the Year 2000 Standard. CDC National Vital Statistics
Reports. 47(3):1-17. Use of the 2000 standard was recommended by a national workshop including representatives from CDC, the National Academy
of Sciences, the National Institutes of Health, State health departments, and academia. The authors note, “the choice (of a standard population) can
make a difference in some cases, when age-specific rates trace divergent trends, or when the age structure of the alternative standard populations
differ.” Further, they note that “standardization is an important and useful tool, (yet) some of its limitations become apparent when changing the
population standard.”
80
Klein RJ, Schoenborn CA. 2001. Age Adjustment Using the 2000 Projected U.S. Population. Healthy People Statistical Notes, no. 20. Hyattsville,
Maryland: National Center for Health Statistics.
81
Curtin LR, Klein RJ. 1995. Direct Standardization (Age-Adjusted Death Rates). CDC/National Center for Health Statistics. DHHS Publication No. (PHS)
95-1237. https://www.cdc.gov/nchs/data/statnt/statnt06rv.pdf
82
Population alignment is specific to the measures used for adjustment. Of note, the approach applies to suicide rates of strata-specific subgroups to
their demographic distribution in the U.S. standard 2000 adult population. Consequently, this increases the relative influence of underrepresented
subpopulations (relative to their distribution in the U.S. standard 2000 adult population) in terms of the overall adjusted suicide mortality rate.
Notably, the Veteran population includes proportionally fewer women and younger adults than did the 2000 U.S. adult population. See: Morral
AR, Schell TL, Smart R. 2023. Comparison of Suicide Rates Among US Veteran and Nonveteran Populations. JAMA Network Open. 6(7):e2324191.
doi:10.1001/jamanetworkopen.2023.24191.
83
The 95 % confidence interval was from 1.096 to 1.152.

32
The direct and indirect adjustment methods indicated that Veterans were at increased risk of suicide in 2021, accounting
for differences in age and sex distributions. Each approach addresses a distinct question.
• Comparison of direct adjusted rates tells us that if the Veteran and non-Veteran U.S. adult populations in 2021 had
the demographic profile of the standard 2000 U.S. adult population, then the Veteran suicide rate would be 71.8%
higher than the rate among non-Veteran adults.
• Indirect adjustment tells us that in 2021 the Veteran population experienced 12.4% more suicide deaths than if the
Veteran population had the strata-specific suicide rates of non-Veteran U.S. adults.
Each approach is valid, and each indicates greater suicide among Veterans in 2021 compared to non-Veteran adults. The
variation between these summary measures relates to differences in population distributions and subgroup-specific
suicide risk differentials.
84
Both approaches have limitations.
• Direct adjustment is best suited for comparing populations with distributions similar to that of the
standard population.
85
• A limitation of indirect adjustment is that SMRs may not be comparable over time if the demographic distribution
of the target population varies over time. Note: The age and sex distributions of the Veteran population changed
substantially from 2001 to 2021.
To address this concern, we examined SMRs standardized to the distribution of the Veteran population of 2021.
86
These
analyses documented elevated suicide mortality among Veterans in 2009 and 2010 and 2014–2021, and lower suicide
mortality among Veterans 2001–2008, relative to non-Veteran U.S. adults. Also, we conducted analyses stratified by sex,
with standardization by age. These analyses indicated that among women, Veteran status was associated with elevated
suicide mortality in each year, and among men, Veteran status was associated with reduced suicide mortality 2001–2008
and 2011–2013 and with increased suicide mortality 2017–2021.
As noted, the variation in trends for the composite adjusted suicide measures is related to heterogeneity in the
populations and strata-specific suicide risks. It is thus important to examine the ratios of strata-specific unadjusted
suicide rates for Veterans relative to non-Veteran U.S. adults. As noted previously, this is the “most informative method of
making comparisons of mortality risk between groups.”
87
Figure 16 shows for U.S. men and women, by age groups, the ratio of the Veteran unadjusted suicide rate and the
unadjusted suicide rate for non-Veteran U.S. adults, 2001–2021.These are rate ratios, rather than rates. Values greater than
1.0 indicate increased risk among Veterans in the age and sex group, and values less than 1.0 indicate decreased suicide
risk among Veterans in the age and sex group.
84
For example, direct adjustment’s weighting of strata-specific suicide rates to the distributions of the Standard U.S. population results in a
reweighting of the differentials in strata-specific rates by Veteran status. Of note, the Standard U.S. population includes proportionally more
women and younger adults than the Veteran population, and for both women and younger adults, the differential in rates by Veteran status is
particularly elevated. As a result, the differential in suicide patterns appears greater using direct adjustment than when using indirect adjustment.
85
Curtin LR, Klein RJ. 1995. Direct Standardization (Age-Adjusted Death Rates). CDC/National Center for Health Statistics. DHHS Publication No. (PHS)
95-1237. https://www.cdc.gov/nchs/data/statnt/statnt06rv.pdf
86
This was calculated as: (Number of suicides that would have occurred if Veteran age- and sex-strata-specific rates in the year occurred in a
population with the distribution of the Veteran population in 2021) / (Number of suicides that would have occurred if non-Veteran U.S. adult
population’s age- and sex-strata-specific rates occurred in a population with the distribution of the Veteran population in 2021).
87
Anderson RN, Rosenberg HM. 1998. Age Standardization of Death Rates: Implementation of the Year 2000 Standard. CDC National Vital Statistics
Reports. 47(3):1-17.

33
Figure 16: Veterans to Non-Veteran U.S. Adults, Age-Group-Specific Suicide Rate Ratios, 2001–2021, Male
and Female
18-34
Male
35-54 55-74 75+
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
4.0
3.5
3.0
2.5
2.0
1.5
1.0
0.5
0
2020 2021
Rate Ratio
18-34
Female
35-54 55
+
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
4.0
3.5
3.0
2.5
2.0
1.5
1.0
0.5
0
2020 2021
Rate Ratio

34
The suicide rate ratios provide the clearest information regarding differentials in suicide risks by Veteran status and how
these vary by sex and age. In all years from 2001–2021, Veterans had greater suicide rates than non-Veterans among men
and women under age 55-years-old (rate ratio greater than 1.0). In all years, Veteran men aged 75-years-old and older had
lower suicide rates than non-Veteran men in the same age group (rate ratio less than 1.0). For men and women, from 2003
through 2021, the highest rate ratios were among those aged 18- to 34-years-old, indicating that for those aged 18- to
34-years-old, increased rates for Veterans were most pronounced, relative to those of non-Veteran men and women.
Veteran Leading Causes of Death
This section provides information on suicide as a leading cause of death among Veterans in 2021. For each leading cause,
we also report age-adjusted cause-specific mortality rates for 2019, 2020 and 2021. In 2021, suicide was the 13th leading
cause of death among Veterans.
88
88
There were 481,718 Veteran deaths in 2019, 529,156 in 2020 and 514,845 in 2021. The unadjusted all-cause Veteran mortality rate in 2019 was 2,430.8
per 100,000, 2,745.0 per 100,000 in 2020 and 2,732.6 in 2021.Thirteen leading causes were presented to be inclusive of suicide, the 13th leading
cause among Veterans in 2021, overall. Causes of death are classified based on the underlying cause of death; leading causes are ranked based on
the number of deaths, by cause.

35
Figure 17 presents leading causes of death, based on counts of deaths, and the age-adjusted mortality rate per 100,000,
for each cause, in 2019–2021.
Figure 17: Leading Causes of Death in 2021, Veterans, and Associated Age-Adjusted Mortality Rates,
2019–2021
89
89
There is no comparison rate for 2019. COVID-19 deaths were identified based on underlying cause of death ICD-10 code U07.1, which was added as
a cause of death code in 2020.
0 50 100 200 250 300150
(1) Heart Disease
(2) Cancer
(3) COVID-19
(5) Stroke
(6) Unintentional Injuries
(7) Diabetes
(8) Alzheimer’s Disease
(9) Kidney Disease
(10) Parkinson’s Disease
(12) Influenza and Pneumonia
(13) Suicide
(11) Chronic Liver Disease and
Cirrhosis
(4) Chronic Lower Respiratory
Disease
Rate per 100,000
241.8
249.7
246.9
218.1
213.7
212.1
100.8
56.5
54.6
50.5
42.2
43.7
44.2
74.0
83.5
90.8
31.2
34.9
35.3
27.7
29.4
25.4
16.7
16.4
17.0
15.2
16.6
14.9
17.7
20.4
22.5
15.5
16.1
13.0
35.8
36.2
38.7
142.8
*
2019
2021
2020

36
The relative rank of suicide as a leading cause of death was higher among younger Veterans (Table 2).
Table 2: First and Second Leading Causes of Death and Suicide Ranking, Veterans, by Age and Sex, 2021
90
First Leading Cause of Death Second Leading Cause of Death
Rank of Suicide as a
Leading Cause of Death
All Veterans
All Ages Heart Disease Cancer 13th
18 to 34 Accident (Unintentional Injury) Suicide 2nd
35 to 44 Accident (Unintentional Injury) Suicide 2nd
45 to 54 COVID-19 Heart Disease 5th
55 to 64 Heart Disease Cancer 9th
65 to 74 Cancer Heart Disease 14th
75 to 84 Heart Disease Cancer 17th
85 and older Heart Disease Cancer 17th
Male Veterans
All Ages Heart Disease Cancer 13th
18 to 34 Accident (Unintentional Injury) Suicide 2nd
35 to 44 Accident (Unintentional Injury) Suicide 2nd
45 to 54 COVID-19 Heart Disease 5th
55 to 64 Heart Disease Cancer 9th
65 to 74 Cancer Heart Disease 14th
75 to 84 Heart Disease Cancer 17th
85 and older Heart Disease Cancer 17th
Female Veterans
All Ages Cancer Heart Disease 9th
18 to 34 Accident (Unintentional Injury) Suicide 2nd
35 to 44 Accident (Unintentional Injury) Cancer 4th
45 to 54 Cancer COVID-19 6th
55 to 64 Cancer Heart Disease 9th
65 to 74 Cancer Heart Disease 13th
75 to 84 Heart Disease Cancer --
85 and older Heart Disease Alzheimer's disease --
90
Ranking is not reported when based on fewer than 10 deaths, indicated by “--.”

37
Years of Potential Life Lost
One measure of the relative impact of different causes of death is their contributions to premature mortality, measured in
terms of Years of Potential Life Lost (YPLL).
91
Analyses for 2019–2021 that are not detailed in this report indicate that suicide was the fourth leading cause of premature
mortality among Veterans in 2019, and it ranked fifth in 2020 and 2021.
92
COVID-19 Pandemic: Suicide Surveillance
Figure 18 shows the number of Veteran suicide deaths, by week, from 12 months prior to the declaration of the COVID-19
pandemic through 2021.
Figure 18: Veteran Suicide Deaths, By Week, 12 Months Prior to Onset of the COVID-19 Pandemic through 2021
• Trend analyses did not identify a change in Veteran suicide mortality trends at onset of the pandemic in 2020.
93
Review of Overall Veteran Suicide Data
In the U.S. adult population as a whole, including Veterans and non-Veteran adults, there were substantial increases
in suicide deaths in 2021. Among Veterans, despite a 2.3% decrease in the Veteran population from 2020 to 2021, the
number of suicide deaths increased, from 6,278 to 6,392. Among non-Veteran U.S. adults, the population increased by
91
YPLL for individuals who died before age 75 are calculated as (75 minus age at death). YPLL are set to zero for individuals who died at age 75 or older.
92
The average number of years of premature mortality per Veteran suicide rose from 17.4 in both 2019 and 2020 to 18.1 in 2021. In 2021, the 6,392
Veteran suicide deaths resulted in an estimated 115,626 years of potential life lost, 5.8% of all YPLL for Veterans who died in 2021. Also, COVID-19
emerged in 2020 as the fourth-leading cause of premature mortality. In 2021, COVID-19 ranked third, with 272,736 estimated YPLL, or 13.7% of all
YPLL for Veterans who died in 2021.
93
Comparing 2019 and 2020, trend analyses using Joinpoint did not identify changes in suicide mortality rates for Veterans or for non-Veteran U.S.
adults, or for Recent Veteran VHA Users or for Other Veterans.
40
60
80
180
160
140
120
100
20
0
3/14/2019
3/28/2019
4/11/2019
4/25/2019
5/9/2019
5/23/2019
6/6/2019
6/20/2019
7/4/2019
7/18/2019
8/1/2019
8/15/2019
8/29/2019
9/12/2019
9/26/2019
10/10/2019
10/24/2019
11/7/2019
11/21/2019
12/5/2019
12/19/2019
1/2/2020
1/16/2020
1/30/2020
2/13/2020
2/27/2020
3/12/2020
3/26/2020
4/9/2020
4/23/2020
5/7/2020
5/21/2020
6/4/2020
6/18/2020
7/2/2020
7/16/2020
7/30/2020
8/13/2020
8/27/2020
9/10/2020
9/24/2020
10/8/2020
10/22/2020
11/5/2020
11/19/2020
12/3/2020
12/17/2020
12/31/2020
1/14/2021
1/28/2021
2/11/2021
2/25/2021
3/11/2021
3/25/2021
4/8/2021
4/22/2021
5/6/2021
5/20/2021
6/3/2021
6/17/2021
7/1/2021
7/15/2021
7/29/2921
8/12/2021
8/26/2021
9/9/2021
9/23/2021
10/7/2021
10/21/2021
11/4/2021
11/18/2021
12/2/2021
12/16/2021
1 2/30/2021
Week Ending

38
0.6% from 2020 to 2021 and the number of suicide deaths increased from 38,020 to 40,020. When looking at increases in
rates over 2020 to 2021, the age- and sex-adjusted suicide rate among Veterans increased by 11.6%, while the age- and
sex-adjusted suicide rate among non-Veteran U.S. adults increased by 4.5%. We also observed that from 2001–2021,
age- and sex-adjusted rates rose significantly faster for Veterans than for non-Veteran U.S. adults. In 2021, the age- and
sex-adjusted suicide rate for Veterans was 71.8% greater than for non-Veteran adults. It is clear from these findings that
Veterans remain at elevated risk for suicide.
Certain sub-populations in 2021 were found to have substantial increases in suicide rates from 2020 to 2021, including
Veterans aged 35- to 54-years-old with an increase of 10.7% in the age-specific suicide rate, women Veterans with an
increase of 24.1% in the age-adjusted suicide rate and American Indian and Alaska Native Veterans with an increase of
51.8% in the unadjusted suicide rate. Further, the prevalence of firearm involvement in Veteran suicide deaths rose from
71.3% to 72.2%, the highest percentage recorded for Veterans over the last 20 years, continuing to be significantly higher
than the non-Veteran U.S. adult population at 52.2%.
Reflecting Back, Looking Forward: Laying the Foundation for Future Courses of
Action for Suicide Prevention for All Veterans
Promote Secure Firearm Storage for Veteran Suicide Prevention
Suicide attempts involving firearms are particularly lethal
94
with an 85–90% likelihood of death compared to 5–10% for
other methods of suicide.
95
Additionally, firearm ownership is more prevalent among Veterans (45%) than non-Veterans
(19%), and the differential in firearm ownership is particularly high among women.
96,97,98,99,100
Veteran suicide deaths
continue to disproportionately involve firearms and Veteran suicide rates exceed those of U.S. non-Veteran adults. One in
3 Veteran firearm owners store at least 1 firearm unlocked and loaded.
101
Building in time and space between a suicidal
impulse and taking action may offer enough time for crisis to pass. Veteran suicide rates will likely not significantly
improve until there is increased collective engagement regarding the relationship between Veteran suicide and firearms.
As such, VA has focused on the secure storage of firearms as a method for reducing Veteran suicide.
94
Spicer RS, Miller TR. 2000. Suicide Acts in 8 States: Incidence and Case Fatality Rates by Demographics and Method. American Journal of Public
Health. 90:1885-1891.
95
Centers for Disease Control and Prevention (2016). Web-based Injury Statistics and Query and Reporting System. Retrieved from http://www.cdc.
gov/injury/wisqars/index.html
96
Combining reports from Azrael et al., 2017, and Cleveland et al., 2017, and VetPop estimates of the 2015 populations of Veteran men and women,
we estimate that in 2015 household firearm ownership among Veteran men was 62.3% higher than for non-Veteran men, and household firearm
ownership among Veteran women was 106.6% higher than for non-Veteran women.
97
Cleveland EC, Azrael D, Simonetti J, Miller M. 2017. Firearm Ownership Among American Veterans: Findings from the 2015 National Firearm Survey.
Injury Epidemiology. 4(1). doi:10.1186/s40621-017-0130-y.
98
Azrael D, Hepburn L, Hemenway D, Miller M. 2017. The Stock and Flow of U.S. Firearms: Results from the 2015 National Firearms Survey. The Russell
Sage Foundation Journal of the Social Sciences. 3(5):38-57.
99
Data from the 2015 National Firearm Survey indicate that 22% of U.S. adults (including Veterans) owned firearms (32% of men, 12% of women). 19%
of non-Veteran adults owned firearms, while 44.9% of Veterans reported firearm ownership (47.2% of Veteran men, 24.4% of Veteran women).
100
Among Veterans receiving VHA mental health care in 2015, 45.3% had firearms in their households, as did 46.9% of those with thoughts of suicide
and 55.6% of those who reported having a plan for suicide. Also, of those respondents who reported household firearms, 83.1% had at least 1
handgun and 38.5% reported having a firearm at home that was both unlocked and loaded. See: Valenstein M, Walters H, Pfeiffer PN, Ganoczy
D, Ilgen MA, Miller MJ, Fiorillo M, Bossarte RM. 2020. Possession of Household Firearms and Firearm-Related Discussions with Clinicians Among
Veterans Receiving VA Mental Health Care. Archives Suicide Research. 24:S260-S279.
101
Simonetti JA, Azrael D, Rowhani-Rahbar A, Miller M. 2018. Firearm Storage Practices Among American Veterans. American Journal of Preventive
Medicine. 55(4):445-454.

39
In 2023, VA continued expansion of secure firearm storage initiatives in training, gun lock distribution, collaboration
efforts and communication and outreach efforts. VA launched an updated VA S.A.V.E.
102
refresher training, required for all
non-clinicians, that includes a larger focus on LMS and secure firearm storage. VA suicide prevention is also collaborating
with the Caregiver Support Program to provide trainings to assist caregiver support personnel in discussing LMS
(firearms and medication) with Veterans/caregivers. VA is on target to reach its agency priority goal of a 10-fold increase
in training of community providers in LMS. VA is actively marketing two LMS trainings to community providers, including
the Community Care Network providers, SSG Fox SPGP grantees and other community providers via a communications
toolkit. This toolkit has been shared with community health care systems (e.g., Kaiser, Cigna, Wounded Warrior Project,
Cohen Veterans Network, Bush Institute) and professional provider organizations and associations (e.g., American
Medical Association, American Psychological Association, American Psychiatric Association and National Association
of Social Workers) and includes an hour-long version and a shorter 25-minute version, provided in collaboration with
PsychArmor. VA also exceeded its agency priority goal to exceed its gun lock distribution to external partners by tenfold
by the end of FY 2023. In FY 2023, from October 2022 through June 2023, VA provided more than 409,000 gun locks
to VHA staff for distribution and more than 245,000 to entities outside VA for distribution. VA Suicide Prevention also
collaborated with the National Cemetery Administration (NCA) to provide gun locks and lethal means safety resources
at all NCA sites. VA continues to expand suicide prevention collaboration across the Nation, including relationships that
are established to amplify lethal means safety messaging across industries. To follow up on a successful initial Firearm
Industry Veteran Suicide Prevention Roundtable in July 2022, co-hosted with the National Shooting Sports Foundation
(NSSF), VA coordinated a follow-up meeting in September 2023, during Suicide Prevention Month, with firearm industry
and trade advocates, manufacturers, retailers and range owners/operators to advance joint efforts to promote secure
firearm storage as part of suicide prevention.
The Keep It Secure campaign has more than 326 million impressions and approximately 100 million video views and
7.8 million LMS website resource visits in FY 2023, to date. Future phases of the secure firearm storage campaign are
underway, including the development of a new national call to action campaign, including industry toolkits, technical
assistance, training, and public service assets. This encompasses the development of a national suicide prevention LMS
resource repository website; the development and dissemination of multi-state maps for out-of-home and secure storage
options; and education training materials in various formats for dissemination. VA also initiated a full Keep It Secure LMS
campaign evaluation to inform impacts, targeting of messaging to diverse populations and efficacy of messaging.
102
The acronym S.A.V.E. helps one remember the important steps involved in suicide prevention: S=Signs of suicidal thinking should be recognized;
A=Ask the most important question of all—“Are you thinking of killing yourself?”; V=Validate the Veteran’s experience; E=Encourage treatment and
Expedite getting help.

40
Reection: Secure Firearm Storage
Summary: The majority of Veterans who die by suicide die by rearm. As many as 9 in 10 suicide attempts that
involve rearms prove lethal. People who attempt suicide by less lethal means are more likely to survive. Storing
your rearm in a locked location and with the ammunition stored separately can allow time and space for reection,
which can save a life.
What You Can Do: Normalize the discussion. It’s okay to ask if someone is having thoughts about suicide. And it
is okay to ask about how they are storing their rearms too. This brochure provides a guide in how to have these
discussions with loved ones. Work within your local communities to promote secure rearm storage, utilizing this
community toolkit and messaging to help Veterans, families and communities learn about putting “time and space”
between a Veteran in crisis and a rearm. Obtain a free gun lock from your local VA and ensure your loved ones
have access to one. Placing objects that have personal meaning, such as pictures of loved ones or personal notes,
by your gun lock or safe, along with a reminder of the Veterans Crisis Line’s number (Dial 988 then Press 1) can serve
as reminders of hope during a time of crisis. All community care providers can assist with reducing rearm Veteran
suicide by taking this training about how to incorporate discussions about secure storage within their clinical care.
Implement and Sustain Community Collaborations Focused Upon Community-
Specific Veteran Suicide Prevention Plans
VA’s SP 2.0 CBI model is grounded in evidence-based practices of community-based prevention and community
implementation science paired with a focus on disseminating suicide prevention strategies within communities across
the country.
103,104
This work is informed by prior community-based and public health suicide prevention approaches
which have been shown to effectively reduce suicide rates in diverse communities.
105
VA’s efforts include effective
community-based suicide prevention programs that focus on both health promotion and “upstream” strategies,
as well as efforts to improve the delivery of clinical and crisis services throughout the community and across other
organizations.
106,107,108
The Governor’s Challenge has now expanded to include all 50 states and 5 U.S. territories. VA’s community-based
interventions support more than 1,700 local community suicide prevention coalitions, an 815% increase from 2021.
These efforts in SP 2.0 CBI-SP are continuing to work across federal, state and community collaborations to reduce
Veteran suicide. The coalitions provide a unifying model to coordinate shared messaging on lethal means safety, suicide
prevention outreach, education, intervention, and the distribution of secure storage resources. To date, almost 40% of the
1,700 coalitions have moved through forming and planning stages to implementation of strategies, meaning more than
7,150,000 Veterans are starting to see efforts locally to prevent suicide. These efforts, which were established to further
the reach of VA’s Public Health Model for Suicide Prevention, now extend to more than 11 million Veterans nationwide.
While this is a major accomplishment, perhaps most important is that this work reflects a deep commitment from states
and communities to work toward ending Veteran suicide.
103
Frieden TR. 2014. Six components necessary for effective public health program implementation. Am J Public Health. 104(1):17-22.
104
Lai C, Law YW, Shum AK, Ip FW, Yip PS. 2019. A Community-Based Response to a Suicide Cluster: A Hong Kong Experience. Crisis: The Journal of
Crisis Intervention and Suicide Prevention. 41(3):163-171.
105
Hegerl U, Althaus D, Schmidtke A, Niklewski G. 2006. The Alliance Against Depression: 2-Year Evaluation of a Community-Based Intervention to
Reduce Suicidality. Psychological Medicine. 36(9):1225-1233.
106
Caine, E. D. (2013, May). Forging an agenda for suicide prevention in the United States. American Journal of Public Health. 103(5), 822-9.
107
Lai C, Law YW, Shum AK, Ip FW, Yip PS. 2019. A Community-Based Response to a Suicide Cluster: A Hong Kong Experience. Crisis: The Journal of
Crisis Intervention and Suicide Prevention. 41(3):163-171.
108
Oyama H, Watanabe N, Ono Y, Sakashita T, Takenoshita Y, Taguchi M, Takizawa T, Miura R, Kumagai K. 2005. Community‐Based Suicide Prevention
Through Group Activity for the Elderly Successfully Reduced the High Suicide Rate for Females. Psychiatry and Clinical Neurosciences. 59(3):337-344.

41
VA has also continued to expand the work with the Ad Council. Since launching “Don’t wait. Reach out.” in October of
2021, the campaign has garnered over $40 million in donated media support, across broadcast, digital, and out-of-home
mediums, resulting in more than 3.5 million visits to VA.gov/REACH. The campaign has worked with several high-profile
media organizations, including Fox Sports, Meta, Twitch, Reddit, We Are the Mighty, Yahoo and YouTube, to reach
Veterans. The campaign has reached 7.9 million Veterans, according to Ad Council campaign tracking studies. This is
approximately 44% of Veterans in the U.S. In FY 2023 through August 31, 2023, there were nearly 2 billion donated media
impressions (opportunities to view the campaign’s PSA), 142,229 donated media detections (times the PSA was shown)
and 3.5 million website visits. In September 2023, VA launched new PSAs for Suicide Prevention Month, continuing the
work of this successful effort.
In addition to expansion of SP 2.0 CBI-SP and communication campaigns to reach all Veterans, VA expanded its reach
to Veterans through a new grant effort. The Staff Sergeant Parker Gordon Fox Suicide Prevention Grant Program (SSG
Fox SPGP), authorized as part of the Commander John Scott Hannon Veterans Mental Health Care Improvement Act of
2019, has awarded $52.5 million to 80 awardees in 43 states, the District of Columbia and American Samoa for services in
FY 2023. The mission of SSG Fox SPGP is to reduce Veteran suicide through awarding grants to eligible entities providing or
coordinating suicide prevention services to eligible individuals and their families. Through June 2023, grantee organizations
have reached more than 10,000 Veterans and families in need and completed assessments that resulted in the identification
of approximately 130 imminent-risk Veterans, 800 non-emergency referrals and approximately 1,800 social service referrals
to address drivers of risk (including homelessness, employment, income supports, legal services and other resources).
Ongoing program evaluation is underway to continue to assess the impact of these services in the community.
SSG Fox SPGP Grantee:
Oneida County and Utica Center for Development
“The Neighborhood Center is honored to be involved in developing and assisting with suicide prevention services for
Veterans alongside Oneida County and Utica Center for Development,” said Sandra Soroka, Executive Director of The
Neighborhood Center.
“The diculties often facing many Veterans can feel overwhelming, especially if they don’t receive help. Society sees
Veterans as heroes, which they are,” she continued.
“They have made sacrices for our country and in return we have an obligation to ensure they receive meaningful
services to help deal with the complexities of emotions, life changes, diculties in resuming their pre-service jobs
and relationships, as well as treatment for Posttraumatic Stress Disorder.”
Reection: Community Prevention
Summary: The majority of Veterans who die by suicide are not engaged in VHA care. We must continue to ensure
methods of outreach and engagement for all Veterans, reminding them of resources and support, both in VA, but
also in their local communities. Connection saves lives.
What You Can Do: Consider joining your Governor’s Challenge state partners to identify ways to support your
local communities in Veteran suicide prevention. Promote the “Don’t wait. Reach out.” campaign messages of hope
through your social media connections and local community networks, using the “Spread the Word” materials
available. Encourage local community organizations that provide or coordinate suicide prevention services to
consider applying for the Sta Sergeant Parker Gordon Fox Suicide Prevention Grant Program.

42
Continue Expansion of Readily Accessible Crisis Intervention Services
The passing of the National Suicide Hotline Designation Act of 2020 provided a critical pathway forward for expanding
ease of access to the National Suicide Prevention Lifeline, now the 988 Suicide & Crisis Lifeline, and VCL with a 3-digit
number (Dial 988 then Press 1 for VCL). VCL is an important part of VA’s public health approach to address Veteran
suicide as it is for all Veterans, not only those engaged in VHA services. VCL is also 1 of the few crisis lines in the country
integrated within an existing health system, as noted by a recent RAND evaluation.
109
Below, we discuss VCL’s growth in
preparation for 988 and its expansion of services after the launch of 988.
From 2021 to 2023, VCL continued preparing for the implementation of 988, hiring over 900 individuals. From the
launch of 988 on July 16, 2022, through June 30, 2023, VCL fielded nearly 1 million contacts, including over 750,000
calls — an increase of 12.5% compared to the same timeframe from the previous year and with an average speed to
answer of 9.4 seconds. In addition, there was a year-over-year increase in text messages (45%) and online chats received
(8.6%). This increase in contacts reflects the work of the VCL campaign to share the message of the easier way to reach
VCL through 988, then Press 1. The VCL communications campaign provided specific resources for connecting to
care as well as nationwide messaging resources through the VeteransCrisisLine.net/Spread-the-Word site. More than
2.1 billion impressions, 575 million completed video views, and more than 100,000 resource locator uses, and self-
check quiz completions reflect that this outreach is working. The growth of VCL’s reach is also supported by extensive
collaboration with SAMHSA, National Action Alliance for Suicide Prevention, Federal Communications Commission,
Cellular Telecommunications Industry Association, Department of Defense, Veterans Service Organizations, community
organizations and more who raised awareness of 988 and VCL. In alignment with ongoing expansion of peer specialist
services into suicide prevention efforts,
110
VCL also expanded its services in 2021 with the establishment of its Peer
Support Outreach Center (PSOC) to provide support, hope, and recovery-oriented services to Veterans beyond their
initial VCL call.
Veterans Crisis Line Services Matter
109
Ramchand R, Jaycox LH, Ebener PA. 2017. Suicide Prevention Hotlines in California: Diversity in Services, Structure, and Organization and the
Potential Challenges Ahead. Rand Health Q. 19;6(3):8. PMID: 28845360; PMCID: PMC5568153.
110
Pfeiffer PN, King C, Ilgen M, Ganoczy D, Clive R, Garlick J, Abraham K, Kim HM, Vega E, Ahmedani B, Valenstein M. 2019. Development and Pilot
Study of a Suicide Prevention Intervention Delivered by Peer Support Specialists. Psychological Services, 16(3), 360-371. https://doi.org/10.1037/
ser0000257
111
Britton PC, Karras E, Stecker T, Klein J, Crasta D, Brenner LA, Pigeon WR. 2022. Veterans Crisis Line Call Outcomes: Distress, Suicidal Ideation, and
Suicidal Urgency. American Journal of Preventive Medicine, 62(5), 745-751. https://doi.org/10.1016/j.amepre.2021.11.013
112
Johnson LL, Muehler T, Stacy MA. 2021. Veterans’ Satisfaction and Perspectives on Helpfulness of the Veterans Crisis Line. Suicide and Life-
Threatening Behavior, 51(2), 263-273. ht t ps://do i.org /10.1111/sl tb.12702
• Over 5 times more likely to have less distress
at the end of the call than at the beginning
• Almost 5 times more likely to have less
suicidal ideation at the end of the call than
at the beginning
• 11 times more likely to have a less suicidal urgency
at end of call than beginning
111
• 82.6% reported that using the Veterans Crisis Line
played a role in stopping them from acting on
suicidal thoughts
112

43
While VCL operations continued to expand, so did the program evaluation efforts to assess VCL effectiveness and impact
on VCL services during the COVID-19 pandemic. During the initial period of the pandemic, “suicidal thoughts or crisis”
were reported by approximately 1 in 5 callers. Female Veteran callers were 15% more likely to report suicidal thoughts
or crisis than male Veteran callers. The VCL program evaluation efforts found that VHA using Veteran callers were over 5
times more likely to have less distress at the end of the call than at the beginning, were almost 5 times more likely to have
less suicidal ideation at the end of the call than at the beginning and were 11 times more likely to have a reduced suicidal
urgency at end of call than beginning.
113
Further, among Veterans who had suicidal thoughts who called VCL, 82.6%
reported that using VCL played a role in stopping them from acting on those thoughts.
114
In addition to the significant expansion of crisis services through VCL, under section 201 of the COMPACT Act, most
Veterans, including those not traditionally eligible for VHA health care, who experience an acute suicidal crisis can go to
any VA or non-VA health care facility for emergent suicide care at no cost — including inpatient or crisis residential care
for up to 30 days and outpatient care for up to 90 days. Like VCL, these services do not require VA enrollment, increasing
access to acute suicide care for all eligible Veterans. Since the launch in January 2023 through August 20, 2023, 30,674
Veterans have received care under the provisions of the COMPACT Act.
115
There has been a tremendous expansion of
access for Veterans in times of crisis both with the COMPACT Act and with the implementation of 988. Yet more must be
done to reach Veterans prior to the time of crisis, which includes laying a foundation for early prevention efforts through
work in the community.
Reection: Crisis Intervention
Summary: Despite the signicant expansion of crisis services through the Veterans Crisis Line and the COMPACT Act,
more work remains with each of you. Many Veterans are not aware that these services are available to them 24/7/365
— and at no cost. With nancial stressors being a critical suicide risk factor, we must ensure Veterans not only know
about the service but that it is free of charge.
What You Can Do: More upstream communications are needed to reach Veterans and their loved ones, reminding
them of support available to them at any time. Help is needed to spread the word about VCL and the COMPACT Act
emergency suicide prevention services by saving 988 (then Press 1) in your phones and using your social media
platforms and local connections to spread the word about VCL and the COMPACT Act.
113
Dichter ME, Krishnamurti LS, Chhatre S, Hoffmire CA, Monteith LL, Bellamy SL, Iverson KM, Montgomery AE, Agha A, McCoy I. 2022. Gender
Differences in Veterans’ Use of the Veterans Crisis Line (VCL): Findings from VCL Call Data. General Hospital Psychiatry. 74:65-70. https://doi.
org/10.1016/j.genhosppsych.2021.12.006
114
Britton PC, Karras E, Stecker T, Klein J, Crasta D, Brenner LA, Pigeon WR. 2022. Veterans Crisis Line Call Outcomes: Distress, Suicidal Ideation, and
Suicidal Urgency. American Journal of Preventive Medicine. 62(5):745-751.
https://doi.org/10.1016/j.amepre.2021.11.013
115
This data is based on notifications, claims, and visits and includes both VA direct care and VA authorized community care.

44
Improve Tailoring of Prevention and Intervention Services to the Needs, Issues,
and Resources Unique to Veteran Subpopulations
The Veteran population is made up of diverse racial and ethnic groups, with minorities currently comprising 26% of
the Veteran population with expectations to rise to 40% by 2040.
116
Women Veterans are likewise a growing Veteran
population, comprising 4% of the Veteran population in 2000 and forecasted to make up 18% of the Veteran population
by 2040. Further, 43% of women utilizing VHA services in FY 2020 belonged to a racial or ethnic minority group.
117
Rural
Veterans comprise approximately 34% of the VHA population and there is an estimated 1 million Veterans who identify
as LGBTQ+.
118,119,120
It is important to note that Veterans are not uni-dimensional in their identity, but rather are defined
by multiple dimensions (e.g., age, race, gender, disability status, rurality, etc.), with each factor impacting their daily
experiences. This intersectionality of diversity is important to attend to as we adapt suicide prevention services for each
Veteran. Focused work is required to study the specific suicide risk factors for each subpopulation and to create suicide
prevention interventions to meet the unique needs for each subpopulation.
121
Below we describe efforts focused on
meeting the diverse needs of Veterans in 2021 and beyond.
Communication and Outreach
The launch of a new PSA for the 2023 Suicide Prevention Month with the “Don’t wait. Reach out.” campaign continued
the ongoing focus of reaching the diverse population that make up America’s Veterans (across age, gender, race, and
ethnicity) through PSA placements in donated media, outreach, influencer engagement and other communication
strategies. Since its first launch in 2021, over 2.8 million Veterans are aware of the campaign and have taken action to
reach out for help. To date, the PSAs have secured over $40 million in donated media support, resulting in more than
3.5 million visits to VA.gov/REACH. Phase II of the national secure firearm storage communication campaign is being
prepared for launch in 2024, continuing a similar focus of designing PSAs to speak to the diverse subpopulations
comprising Veterans across the Nation. This includes specific focus on Veteran subpopulations, particularly those at
higher risk for suicide, including, but not limited to, women Veterans under age 35-years-old, Veterans 18- to 34-years-
old, American Indian or Alaska Native Veterans, Asian American Pacific Islander Veterans, LGBTQ+ Veterans, rural
Veterans, survivors of military sexual trauma and White male Veterans over the age of 55-years-old.
Community Prevention
With the implementation of the Staff Sergeant Fox Suicide Prevention Grant Program (SSG Fox SPGP), VA awarded 80
grants in 43 states, the District of Columbia and American Samoa for services in FY 2023. In awarding grants under the
program, VA prioritized funding of applications to organizations that proposed to serve eligible individuals and their
families in rural communities, on tribal lands, in U.S. territories, in medically underserved areas, in areas with a high
number or percentage of minority Veterans or women Veterans and in areas with a high number or percentage of
calls to VCL. Twenty-one grantees are furnishing services specifically across tribal lands, including: the Navajo Nation,
Cherokee Nation, and Choctaw Nation under this inaugural round of funding. In addition to significantly advancing
the reach to diverse Veteran populations through the SSG Fox SPGP, the ongoing expansion of the CBI-SP work to all
50 states, 5 territories and over 1,700 coalitions also provided the opportunity to reach a larger population of Veterans.
116
National Veteran Health Equity Report (https://vha-healthequity.shinyapps.io/NVHER_Shiny).
117
Facts and Statistics - Women Veterans Health Care (va.gov).
118
LGBTQ+ refers to lesbian, gay, bisexual, transgender, and queer identities. The “+” sign captures identities beyond LGBTQ, including but not limited
to questioning, pansexual, asexual, agender, gender diverse, nonbinary, gender-neutral, and other identities.
119
Washington DL (ed). National Veteran Health Equity Report 2021. Focus on Veterans Health Administration Patient Experience and Health Care Quality.
Washington, DC: VHA Office of Health Equity; September 2022.
120
VA LGBTQ+ Veterans (dav.org).
121
Ramchand R, Gordon JA, Pearson JL. Trends in Suicide Rates by Race and Ethnicity in the United States. JAMA Netw Open. 2021;4(5):e2111563.
doi:10.1001/jamanetworkopen.2021.11563.

45
One of the unexpected yet positive outcomes of the local and state suicide prevention work is the broad and diverse
groups engaging, with almost 95% of local coalition membership coming from non-VHA sources. Key members include
a diverse set of individuals from faith-based groups, local government, education, media, community wellness, health
care, business, and public safety along with traditional collaborators focused on mental health. This is resulting in
strong coalitions, driven by the community, with broad representation that can bring additional resources to the work
and address upstream prevention before the point of crisis. CBI-SP is also supporting more than 300 VA employees
both locally, at the Veterans Integrated Service Network (VISN) level and nationally devoted to implementing the CBI-
SP program at all levels by providing technical assistance, education, training, public health expertise and community
coalition facilitation support to local and state efforts. By focusing on supporting local efforts, VA helps communities
adapt evidence-informed models to local opportunities and resources and plan interventions that fit the community
and the diverse populations they serve. In FY 2024, VA looks forward to continuing to support communities, applying
lessons learned, and moving towards broader coverage of Veteran populations, including specific sub-populations, with
coalitions moving to implementation of strategies.
Research and Innovation
In 2023 and beyond, VA Suicide Prevention continued expansion of its funding of demonstration projects, research, and
innovation to support meeting the needs of a diverse population. This included a process for prioritizing several high-
risk for suicide populations and broader subpopulations for which additional research and intervention development
is needed: Asian American and Pacific Islander Veterans, American Indian and Alaskan Native Veterans, Veterans with
co-morbid medical conditions that increase suicide risk (e.g., non-mental health drivers of services to high-risk Veterans),
LGBTQ+, Older Veterans, Transitioning Service Members (TSM), Women Veterans, Black Veterans, Hispanic Veterans and
younger Veterans (aged 18- to 34-years-old). In particular, VA will be moving forward with a study of the adaptation of
suicide prevention evidence-based treatments for effective delivery of these treatments within diverse subpopulations,
with specific study of treatments, such as: Cognitive Behavioral Therapy for Suicide Prevention, Problem Solving Therapy
for Suicide Prevention and Dialectical Behavioral Therapy for Suicide Prevention. Additional efforts are underway for
the development and delivery of Lethal Means Safety interventions with older Veterans, Veterans aged 18- to 34-years-
old, caregivers and concerned others. This research will include efforts to understand the unique drivers of suicide
risk and effective approaches for serving Asian American and Pacific Islander Veterans, defining methods for reducing
firearm risks among Veterans with substance use disorders, the most effective outreach and engagement methods to
reduce suicide risk among American Indian and Alaska Native Veterans, risk reduction strategies for homeless Veterans,
establishing suicide risk reduction outreach strategies for LGBTQ+ Veterans, collaboration opportunities with firearm
retailers to promote and provide out-of-home firearm storage options and transitioning Service member risk reduction
strategies. Please see Appendix A for a full listing of all projects.
Additionally, VA’s Suicide Prevention Research Impact NeTwork (SPRINT) continues its critical work to accelerate VA
suicide prevention research to improve care and reduce suicidal thoughts and behaviors among Veterans. In the coming
year, SPRINT is specifically focusing studies upon the following 4 Veteran groups to advance efforts: younger Veterans,
women Veterans, underserved Veterans and minority Veterans, including those from disadvantaged groups. In 2023,
VA also announced the final winners of Mission Daybreak, VA’s $20 million suicide prevention grand challenge. Sourcing
outside entities, such as academia, industry experts, nonprofits, and community organizations, can improve Veteran
suicide prevention efforts by providing platforms to engage solutions for a multifactorial problem. This open innovation
program created an opportunity for a diversity of solvers, including Veterans, researchers, technologists, advocates,
clinicians, and health innovators, to offer solutions for Veteran suicide prevention. One of the 2 first-place winners,
Televeda’s Project Hózhó, developed the first mental health app for American Indian and Alaska Native populations in
collaboration with American Indian and Alaska Native communities and communities for Navajo Veterans.

46
Clinical Innovation
In addition to the efforts in Diversity, Equity and Inclusion (DEI) communication and outreach, community prevention
and research and innovation, VA worked extensively to incorporate DEI principles within its rollout of Suicide Prevention
2.0 Clinical Telehealth.
122
DEI subject matter experts (SME) worked in collaboration with each suicide prevention
evidence-based psychotherapy (SP-EBP) training program, and provided feedback related to training materials (e.g.,
didactic PowerPoint slides, training videos, case formulation templates) and practices (e.g., workshops, case-based
consultation meetings). SMEs participated in training events and actively collaborated in the creation or review/audit
of materials. Each SP-EBP training program implemented DEI SME recommendations related to training components
(e.g., checklist to promote awareness of one’s own cultural biases; rehearsal of positionality statements; considerations
of disability accommodations; video recordings demonstrating cultural discussions in both the therapeutic setting and
in the therapist-training context; integration of DEI elements in training PowerPoint slides; provision of theoretical and
empirical literature regarding cultural considerations in the context of suicide prevention, etc.). Ongoing efforts are
underway to translate SP-EBP training material to Spanish.
Reection: Suicide Prevention Eorts for Diverse Populations
Summary: A one-size-ts-all approach will not be eective in meeting the needs of the diverse Veteran population.
Ongoing work is needed to ensure prevention and intervention frameworks are modied in a culturally appropriate
manner to meet the unique needs of each population in the broader Veteran community, not just those engaged in
VHA or VBA services.
What You Can Do: If you are a researcher with expertise in suicide prevention focused on meeting the needs of
diverse populations, reach out to VA’s Suicide Prevention Research Impact NeTwork (SPRINT) to discuss potential
opportunities for joint research. VA also collaborates with external organizations in research through the VA
Partnered Research Program. If you are part of an organization providing suicide prevention services in a diverse
subpopulation of Veterans, consider submitting a future application to the Sta Sergeant Parker Gordon Fox Suicide
Prevention Grant Program. If you are a Veteran, consider visiting the Make the Connection website, where you can
search for Veterans from diverse backgrounds and experiences and hear their personal stories of hope and resilience.
122
Program described further in the latter part of this report.

47
Part 2: Veterans with VHA or VBA Contact
This section of the report provides information regarding suicide among Veterans who have had contact with VHA and
among Veterans who have had contact with VBA.
123
Findings include suicide rates for annual cohorts of Veterans who received VHA health care
124
in the year or prior year,
who in this report are described as “Recent Veteran VHA Users” or as “VHA Veterans”, including by demographic and clinical
subgroups, rurality, VHA enrollment, and VA eligibility priority groups. Rates are also included for Veterans by receipt of
VBA benefits and for Veteran subgroups defined by receipt of VBA or VHA services. For Veterans who died from suicide in
2021, we report on points of VA contact, including receipt of VHA health care, VHA enrollment and receipt of VBA services.
Veterans Health Administration (VHA) Health Care
VHA Health Care Engagement, 2001–2021
From 2001 to 2021, the Veteran population decreased by 27.0%. Over these years, VA continued to expand health care
eligibility
125
and there were substantial increases in Veteran receipt of VHA health care. Despite decreases in the overall
Veteran population, the number of Veterans with VHA health care encounters in the year or prior year (Recent Veteran
VHA Users) rose 52.8%, from 3.8 million in 2001 to 5.9 million in 2021. In 2021, Recent Veteran VHA Users accounted for
31.2% of all Veterans, up from 14.9% in 2001.
Prior studies report differences between Veterans with versus without VHA health care services utilization. For example,
Veterans receiving VHA care are more likely to be unmarried, smokers and from minority populations, with less
education, lower annual incomes, poorer self-reported health status,
126
more chronic medical conditions
127
and self-
reported disability due to physical or mental health factors,
128
greater depression and anxiety,
129
and greater reporting
123
VHA delivers health services for Veterans. VBA supports Veterans in 5 areas of benefits and entitlements: Compensation and Pension; Education;
Home Loan Guaranty; Insurance; and Veteran Readiness and Employment.
124
VHA health care receipt is here defined as having at least 1 VHA inpatient or outpatient utilization record, per VHA Corporate Data Warehouse
records. VHA health care is regarded “as good as or better than non-VA care in terms of clinical quality and safety.” Apaydin EA, Paige NM,
Begashaw MM, Larkin J, Miake-Lye IM, Shekelle PG. 2023. Veterans Health Administration (VA) vs. non-VA Healthcare Quality: A Systematic
Review. J Gen Intern Med. doi: 10.1007/s11606-023-08207-2. O’Hanlon C, Huang C, Sloss E, et al. 2016. Comparing VA and non-VA Quality of Care:
A Systematic Review. 32(1):105-121.
125
For example, the National Defense Authorization Act of 2008 extended the period of eligibility for health care for Veterans who had served in a
theater of combat operations after 11/11/1998 to 5 years following discharge or release. Qualifying Veterans would be eligible for enrollment in Priority
Group 6 unless eligible for enrollment in a higher priority group. https://www.va.gov/healthbenefits/assets/documents/publications/FS16-4.pdf
126
Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. 2000. Are Patients at Veterans Affairs Medical Centers Sicker? A Comparative Analysis of Health
Status and Medical Resource Use. Arch Intern Med. 160:3252-3257.
127
Dursa EK, Barth SK, Bossarte RM, Schneiderman AI. 2016. Demographic, Military, and Health Characteristics of VA Health Care Users and Nonusers
Who Served in or During Operation Enduring Freedom or Operation Iraqi Freedom, 2009–2011. Public Health Reports. 131(6):839-843.
128
Nelson KM, Starkebaum GA, Reiber GE. 2007. Veterans Using and Uninsured Veterans Not Using Veterans Affairs (VA)
Health Care. Public Health Rep. 122:934-100.
129
Fink DS, Stohl M, Mannes ZL, Shmulewitz D, Wall M, Gutkind S, Olfson M, Gradus J, Keyhani S, Maynard C, Keyes KM, Sherman S, Martins S, Saxon
AJ, Hasin DS. 2022. Comparing Mental and Physical Health of U.S. Veterans by VA Healthcare Use: Implications for Generalizability of Research in the
VA Electronic Health Records. BMC Health Services Research. 22:1500 https://doi.org/10.1186/s12913-022-08899-y

48
of trauma, lifetime psychopathology and current suicidality.
130
To inform Veteran suicide prevention approaches —
including clinical-and community-focused initiatives — we continue to work to understand trends in suicide mortality
among Recent Veteran VHA Users and among Other Veterans.
Suicide Deaths
Figure 19 presents the annual number of Veteran suicide deaths, 2001–2021, and the percentage among Recent Veteran
VHA Users (“VHA Veterans”) and Other Veterans.
Among Veteran suicide decedents, the percentage with Recent VHA encounters increased from 26.2% in 2001 to 38.1% in
2021. From 2019 to 2021, the percentage of Veteran suicide decedents with Recent VHA encounters fell from 38.3% to 38.1%.
Figure 19: Veteran Suicide Decedents, Number and Percentage With and Without Recent VHA Health Care
Encounters,
131
2001–2021
130
Meffert BN, Morabito DM, Sawicki DA, Hausman C, Southwick SM, Pietrzak RH, Heinz AJ. 2019. U.S. Veterans Who Do and Do Not Utilize VA Health
Care Services: Demographic, Military, Medical, and Psychosocial Characteristics. Primary Care Companion CNS Disorders. 21(1):doi:10.4088/
PCC.18m02350.
131
With a VHA health care encounter in the year of interest or the prior year.
VHA Veterans Other Veterans
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
Number
7,000
6,000
5,000
4,000
3,000
2,000
1,000
0
26%
28%
27%
29% 28%
30%
29%
30%
29%
30%
33% 33%
34%
34%
35%
36% 35%
36%
38%
39% 38%
74%
72%
73%
71%
72% 70%
71%
70%
71%
70%
67%
67%
66%
66% 65%
64%
65%
64%
62%
61%
62%

49
Suicide Rates
Table 3 presents changes in suicide rates from 2001 to 2021 and from 2020 to 2021 for age- and sex-subgroups of Recent
Veteran VHA Users
132
and Other Veterans.
Table 3: Suicide Rate per 100,000,
133
Change from 2001 to 2021 and from 2020 to 2021, Veteran VHA Users
and Other Veterans, by Sex and Age
134
2001 2021 Change 2020 2021 Change
Recent Veteran VHA Users
Men
Aged 18–34 35.6 71.5 +100.1% 73.0 71.5 -1.9%
Aged 35–54 52.1 50.9 -2.3% 44.3 50.9 +14.9%
Aged 55–74 36.5 33.2 -9.0% 33.4 33.2 -0.6%
Aged 75+ 43.9 50.3 +14.6% 55.0 50.3 -8.6%
Women
Aged 18–34 -- 40.5 -- 23.8 40.5 +70.6%
Aged 35–54 17.2 21.6 +25.6% 13.4 21.6 +61.9%
Aged 55–74 -- 12.1 -- 16.1 12.1 -24.9%
Aged 75+ -- -- -- -- -- --
Other Veterans
Men
Aged 18–34 25.5 49.9 +95.5% 44.9 49.9 +11.2%
Aged 35–54 25.9 34.3 +32.4% 32.4 34.3 +6.1%
Aged 55–74 14.2 30.7 +116.6% 27.2 30.7 +12.8%
Aged 75+ 23.8 25.6 +7.7% 27.8 25.6 -7.8%
Women
Aged 18–34 7.3 18.2 +150.1% 18.1 18.2 +1.0%
Aged 35–54 13.4 17.2 +27.7% 15.4 17.2 +11.5%
Aged 55–74 -- 15.5 -- 10.3 15.5 +50.4%
Aged 75+ -- -- -- -- -- --
132
Among Recent Veteran VHA Users between ages 55- and 74-years-old, overall, the suicide rate fell from 2020 to 2021 by 2.2% (-0.6% for men and
-24.9% for women).
133
As rates are specific to age- and sex-subgroups, adjustment was not applicable.
134
Rates are suppressed if there were fewer than 10 suicide deaths, and rates are more variable for smaller Veteran subpopulations.
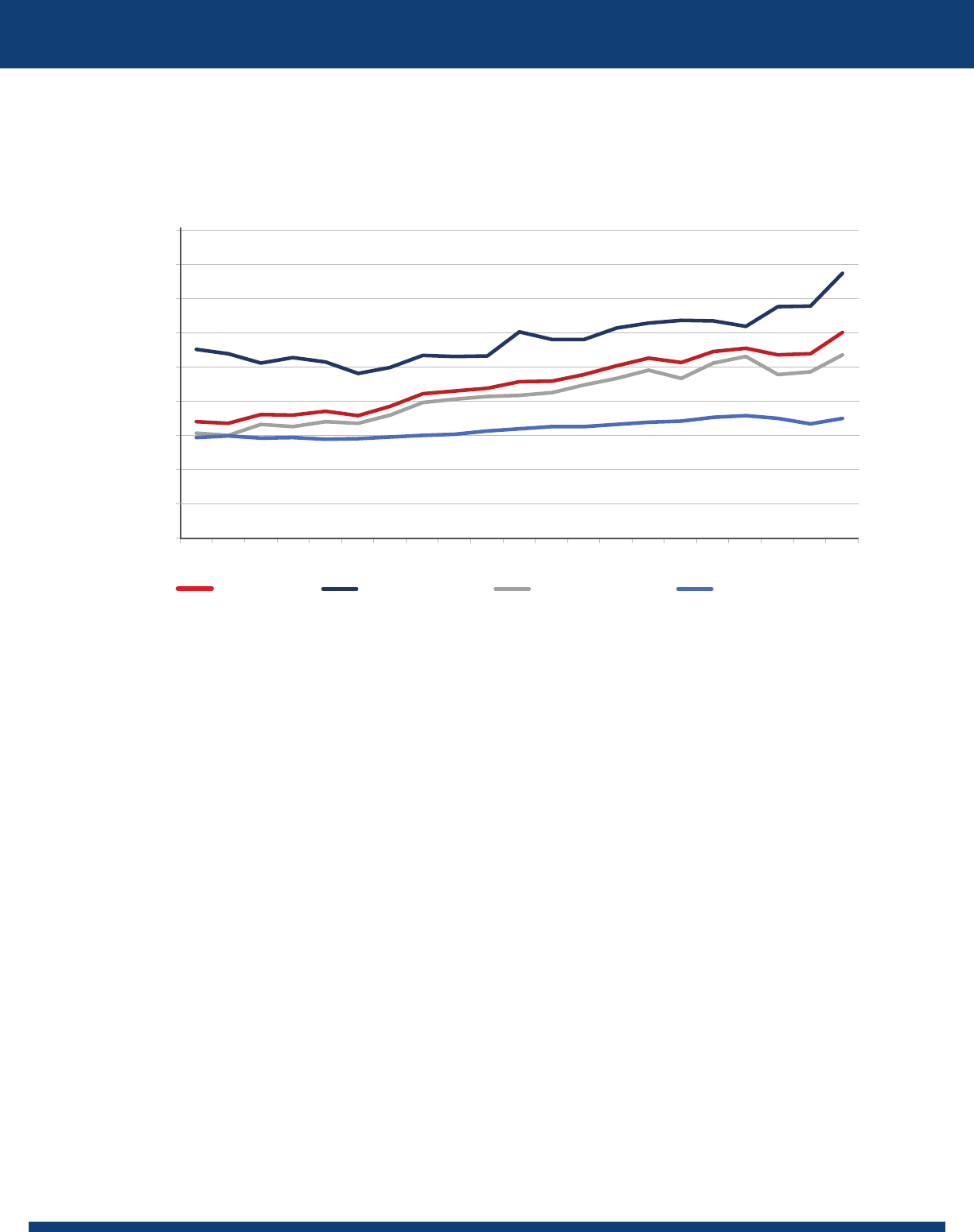
50
Figure 20 presents age- and sex-adjusted suicide rates among Veterans overall, Recent Veteran VHA Users (“VHA
Veterans”), Other Veterans, and non-Veteran U.S. adults, 2001–2021.
Figure 20: Age- and Sex-Adjusted Suicide Rates, Veterans, Overall and by Recent VHA Care, and Non-
Veteran U.S. Adults, 2001–2021
• Age- and sex-adjusted suicide rates were higher among Recent Veteran VHA Users (VHA Veterans) than for
Other Veterans.
• From 2001 to 2021, age- and sex-adjusted rates increased by 40.1% for Recent Veteran VHA Users and by 73.7%
among Other Veterans.
• From 2020 to 2021, adjusted rates among Recent Veteran VHA Users increased by 13.9% and rates among Other
Veterans increased by 10.2%.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
45
40
35
30
25
20
15
10
5
0
2020 2021
Age- and Sex-Adjusted Rate per 100,000
Veterans VHA Veterans Other Veterans Non-Veteran Adults

51
Figure 21 highlights age- and sex-adjusted suicide rates for Recent Veteran VHA Users and for Other Veterans, 2001–2021,
including 95% confidence intervals. Rates were higher for Recent Veteran VHA Users than for Other Veterans.
Figure 21: Age- and Sex-Adjusted Suicide Rate, with 95% Confidence Interval, Veterans, by Recent VHA Use,
2001–2021
Table 4 presents comparisons, by sex, of age-adjusted suicide rates, for 2021 and 2001 and for 2021 and 2020.
Adjusted rates rose substantially from 2001 to 2021 for Recent Veteran VHA Users and for Other Veterans. From 2020 to
2021, age-adjusted rates rose for Recent Veteran VHA Users and for Other Veterans.
Table 4: Age-Adjusted Suicide Rate per 100,000, Change from 2001 to 2021 and from 2020 to 2021, Veteran
VHA Users and Other Veterans, by Sex
2001 2021 Change 2020 2021 Change
Recent Veteran VHA Users
Men 43.1 53.6 +24.5% 51.9 53.6 +3.4%
Women 13.4 25.2 +87.1% 16.8 25.2 +49.8%
Other Veterans
Men 23.2 37.7 +62.6% 34.8 37.7 +8.3%
Women 8.3 16.1 +93.7% 14.4 16.1 +12.1%
• For Veteran men with recent VHA care, the age-adjusted rate rose by 3.4% from 2020 to 2021, while for Veteran
women with recent VHA care, the age-adjusted suicide rate rose by 49.8%.
135
• From 2001 to 2021, age-adjusted suicide rates rose 24.5% for male Veterans with Recent VHA use and 62.6% for male
Veterans without Recent VHA use. Age-adjusted suicide rates rose 87.1% for female Veterans with recent VHA use
and 93.7% for female Veterans without Recent VHA use.
135
Due to increases in suicides among women Recent Veteran VHA Users between ages 18–54 and those aged 75 and older. Given the relatively smaller
population size for women Veterans in VHA care, there is greater variability in rates from year to year.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
45
40
35
30
25
20
15
10
5
0
2020 2021
Age- and Sex-Adjusted Rate per 100,000
VHA Veterans Other Veterans

52
Marital Status
Figure 22 presents suicide rates among Recent Veteran VHA Users by marital status.
136
In each year, suicide rates were lowest among Recent Veteran VHA Users who were married, compared to those with
other categories of marital status.
Figure 22: Unadjusted Suicide Rate, Recent Veteran VHA Users, by Marital Status, 2001–2021
Mental Health and Substance Use Disorder Diagnoses
Ensuring access to mental health and substance use disorder (SUD) services is a VHA priority and part of VA’s National
Strategy for Preventing Veteran Suicide (2018).
137
The prevalence of VHA mental health or SUD diagnoses among annual cohorts of Recent Veteran VHA Users was 27.8% in
2001; 40.7% in 2019; and then 41.7% and 41.9% in 2020 and 2021, respectively.
138
• Among annual cohorts of Recent Veteran VHA Users who died from suicide, VHA mental health or SUD diagnoses
were documented for 56.1% of those who died in 2001; 59.4% of suicide decedents in 2019; 58.0% of suicide
decedents in 2020; and 60.9% of suicide decedents in 2021.
• Among those who died from suicide in 2021, the prevalence of depression diagnoses was 38.4%, anxiety 27.6%,
posttraumatic stress disorder (PTSD) 25.4%, alcohol use disorder 19.7%, bipolar disorder 8.7%, cannabis use disorder
8.4%, opioid use disorder 4.2%, personality disorder 4.2% and schizophrenia diagnoses 3.5%.
• Conversely, 39.1% of Recent Veteran VHA Users who died from suicide in 2021 did not have a documented VHA
mental health or SUD diagnosis.
• The suicide rate among cohorts of Recent Veteran VHA Users with mental health or SUD diagnoses fell from 77.8 per
136
Per VHA visit records, using the most recent status in the year or prior year. Excludes those with unknown marital status.
137
https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-
Veterans-Suicide.pdf. (Accessed 7/10/2023)
138
Diagnoses were assessed in the year or prior calendar year. An individual’s likelihood of having a documented diagnosis may vary by the
number of VHA health care contacts in the relevant period. VHA transitioned from International Classification of Diseases, Ninth Revision, Clinical
Modification (ICD-9-CM), to ICD-10-CM diagnosis codes on Oct. 1, 2015. Diagnoses were not mutually exclusive, and analyses do not adjust for
demographic differences or comorbidities.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
70
60
50
40
30
20
10
0
2020 2021
Rate per 100,000
Single or Never Married
Married
Divorced or Separated
Widowed

53
100,000 in 2001 to 58.2 per 100,000 in 2021. In 2019, prior to the COVID-19 pandemic, the rate was 57.2 per 100,000.
This fell to 55.5 per 100,000 in 2020 and then rose to 58.2 per 100,000 in 2021. By contrast, the rate among Recent
Veteran VHA Users who did not have documented mental health or SUD diagnoses rose from 25.5 per 100,000 in
2001 to 28.5 per 100,000 in 2021. This rose from 28.0 per 100,000 in 2019 to 29.7 per 100,000 in 2020, then fell to 28.5
per 100,000 in 2021.
• Trends in rates varied by condition. From 2001 to 2021, suicide rates fell 25.2% for patients with mental health/SUD
diagnoses, while rising 12.0% for patients without documented mental health/SUD diagnoses.
• From 2001 to 2021, suicide rates fell for Recent Veteran VHA Users with diagnoses of:
• Sedative use disorder (-40.4%);
139
• Depression (-32.9%);
• PT SD (-27.6%);
• Anxiety (-26.9%);
• Alcohol use disorder (-12.6%);
• Substance use disorders (-9.9%);
• Personality disorder (-7.3%); and
• Schizophrenia (-4.2%).
• From 2001 to 2021, suicide rates rose for Recent Veteran VHA Users with diagnoses of:
• Bipolar disorder (+7.3%);
• Opioid use disorder (+21.1%);
• Cocaine use disorder (+50.9%);
• Cannabis use disorder (+17.0%); and
• Stimulant use disorder (+18.6%).
139
In 2001, there were 21 suicides among Recent Veteran VHA Users with sedative use disorder. In 2021, there were 29.

54
For 2021 and 2020 Recent Veteran VHA User cohorts, Table 5 presents the number of suicide deaths and unadjusted
suicide rates per 100,000.
• From 2020 to 2021, suicide rates rose for those with any mental health or SUD diagnosis and also for those with any
SUD diagnosis, while declining for patients without a mental health or SUD diagnosis.
Table 5: Suicide Deaths and Unadjusted Suicide Rates, Recent Veteran VHA Users, by Mental Health (MH)
and Substance Use Disorder (SUD) Diagnoses,
140
2020 and 2021
Diagnoses Suicide Deaths
Suicide Rates per 100,000
Person-Years
2020 2021 2020 2021 Rate Change
141
Without MH Condition/SUD 1,024 954 29.7 28.5 -1.1
With Any MH Condition/SUD 1,416 1,483 55.5 58.2 +2.7
Anxiety 625 673 64.8 67.9 +3.1
Bipolar disorder 184 212 111.5 131.0 +19.6
Depression 859 936 60.9 66.5 +5.6
Personality disorder 112 102 148.0 142.1 -5.8
Posttraumatic stress disorder 596 620 53.0 54.1 +1.1
Schizophrenia 109 84 123.6 100.0 -23.6
Substance Use Disorder 626 618 89.9 90.8 +0.9
Alcohol use disorder 478 480 90.2 93.2 +3.1
Cannabis use disorder 202 204 108.9 112.2 +3.4
Cocaine use disorder 67 70 74.9 86.1 +11.1
Opioid use disorder 119 102 133.2 119.1 -14.1
Sedative use disorder 33 29 185.9 180.4 -5.5
Stimulant use disorder 93 95 159.9 177.7 +17.8
140
Diagnosis categories are not mutually exclusive.
141
Change in suicide deaths per 100,000; these were calculated using non-rounded numbers.

55
Homelessness
Figure 23 presents suicide rates among annual cohorts of Recent Veteran VHA Users, by homelessness status,
142
2001–2021.
• In each year, the unadjusted suicide rate of Recent Veteran VHA Users with indications of homelessness was
elevated compared to those without indications of homelessness.
• In 2001, the suicide rate for Recent Veteran VHA Users with indications of homelessness was 72.8% higher
than for those without indications of homelessness.
• In 2021, the suicide rate among homeless Recent Veteran VHA Users was 186.5% higher than for those
without indications of homelessness.
• In 2021, the unadjusted suicide rate among Recent Veteran VHA Users with indications of homelessness was 62.4%
higher than in 2001, 30.5% higher than in 2019, and 38.2% higher than in 2020.
Figure 23: Unadjusted Suicide Rate, Recent Veteran VHA Users, by Homelessness Status, 2001–2021
Veterans Justice Programs
Among Veterans in VHA care, those with legal system involvement are at increased risk of suicide-related behavior.
143
VHA
connects with Veterans who are at various points in the legal system, through Veterans Justice Programs. These support
Veterans in prison through the Health Care for Re-Entry Veterans (HCRV) Program and they support Veterans in courts,
jails, and law enforcement settings through the Veterans Justice Outreach (VJO) program.
142
Homelessness is identified using ICD-9 Code V60.0 and ICD-10 Code Z59.0 recorded during encounters at VA hospitals. Though additional
methods exist to identify homelessness status among VA patients (Tsai J, Szymkowiak D, Jutkowitz E. 2022. Developing an Operational Definition
of Housing Instability and Homelessness in Veterans Health Administration’s Medical Records. PLOS ONE.17(12):e0279973.) ICD codes were a
consistently available indicator across the years 2001–2021. We considered individuals as having an indication of homelessness if they had an ICD
code during an encounter in the year or year prior.
143
Palframan KM, Blue-Howells J, Clark SC, McCarthy JF. 2020. Veterans Justice Programs: Assessing Population Risks for Suicide Deaths and Attempts.
Suicide and Life-Threatening Behavior. 50(4):792-804.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
120
100
80
60
40
20
0
2020 2021
Rate Per 100,000 Person-Years
Homeless Without Homelessness Indication

56
Figure 24 presents information on suicide rates among annual cohorts of Recent Veteran VHA Users who received
services through the HCRV or VJO programs.
• In each year, suicide rates for Recent Veteran VHA Users were elevated among those with Veterans Justice Program
services compared to those without such contact.
• The suicide rate for recipients of Veterans Justice Program services was 10.2% higher in 2021 than in 2020, while
rising 1.8% for other Veterans in VHA care.
Figure 24: Unadjusted Suicide Rate, Recent Veteran VHA Users, by Receipt of Veterans Justice Program
Services, 2010–2021
144
144
Assessed per VHA outpatient encounters codes 591 (Health Care for Re-Entry Veterans) or 592 (Veterans Justice Outreach) or with encounters for
which “Justice Outreach” was identified as the activity type. We considered individuals as having receipt of Veterans Justice Program services if
they had these encounters in the year or year prior.
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
160
140
120
100
80
60
40
20
0
20212020
Rate per 100,000 Person-Years
Other VeteransWith Veterans Justice Program Contact

57
Rurality
• Among Recent Veteran VHA Users, suicide rates were elevated for residents of rural areas, compared to urban
areas (Figure 25). For example, in 2021 for individuals in rural or highly rural areas, the rate was 44.3 per 100,000,
and it was 40.0 per 100,000 for those in urban areas. These differences may be partly attributed to demographic
differences among Veteran VHA Users, by rurality status.
145
• For Recent Veteran VHA Users in rural areas, rates rose from 2019 to 2020 (43.5 per 100,000 to 44.9 per 100,000) then
fell to 44.3 per 100,000 in 2021.
• For Recent Veteran VHA Users in urban areas, rates rose from 38.6 per 100,000 in 2019 to 38.7 per 100,000 in 2020
and to 40.0 per 100,000 in 2021.
Figure 25: Unadjusted Suicide Rate Per 100,000 Person-Years, Recent Veteran VHA Users, By Urban, Rural
or Highly Rural Status, 2001–2021
Gender Identity
VA is continuing work to enhance data resources to inform suicide prevention for Veteran subgroups by gender identity.
Self-identified gender identity remains the best approach for ascertaining gender identity, including transgender
identity. However, current systems are not yet sufficiently developed for comprehensive reporting. Transgender Veterans
— whose gender identity differs from the identity assumed by their assigned sex at birth — in VHA care are at increased
risk for suicidal ideation
146
and non-fatal suicide attempts.
147
For this report, we assessed a measure of transgender
identity using diagnosis indicators
148
linked to transgender identity that are most often used in the context of gender-
affirming therapy.
149
145
Peltzman T, Gottlieb DJ, Levis M, Shiner B. 2022. The Role of Race in Rural-Urban Suicide Disparities. Journal of Rural Health. 38[2]:346-354.
146
https://www.va.gov/HEALTHEQUITY/docs/LGBT_Veterans_Disparities_Fact_Sheet.pdf
147
Blosnich JR, Boyer TL, Brown GR, Kauth MR, Shipherd JC. 2021. Differences in Methods of Suicide Death Among Transgender and Nontransgender
Patients in the Veterans Health Administration, 1999-2016.59:S31-S35.
148
Diagnoses related to gender identity include ICD-9-CM codes 302.5, 302.6, and 302.85 and ICD-10-CM codes F64 and Z87.890.
149
This approach likely undercounts the number of transgender Veterans in VHA care.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
50
45
40
35
30
25
20
15
10
5
0
2020 2021
Rate per 100,000 Person-Years
Rural or Highly RuralUrban

58
To enhance sensitivity of ascertainment, we generated annualized suicide rates for cohorts from 2011–2020, for suicide in
the year of interest through the end of the subsequent year, for Recent Veteran VHA Users with a VHA diagnosis related to
gender identity occurring in the year or the prior 3 years.
The number of Veteran VHA patients with diagnoses related to gender identity increased from 2,514 in 2011 to 9,218 in
2020 (Table 6), and the unadjusted annualized suicide rate fell from 267.9 per 100,000 person-years in 2011 to 84.6 per
100,000 person-years in 2020.
Table 6: Unadjusted Suicide Rate in Year and Following Year, Veteran VHA Users with Diagnoses in the Year
or Prior 3 Years Related to Gender Identity, 2011–2020
150
Year
Veteran VHA Patients
with Diagnoses Related to
Gender Identity in Year or
Prior 3 Years
Percentage of Veteran
VHA Users
Suicide Deaths
in Year
or Subsequent Year
Unadjusted Suicide Rate Per
100,000 Person-Years
2011 2,514 0.04% 13 267.9
2012 2,843 0.05% -- --
2013 3,311 0.05% -- --
2014 3,830 0.06% 10 134.7
2015 4,623 0.07% 12 133.1
2016 5,556 0.09% 11 101.7
2017 6,436 0.10% 17 136.1
2018 7,426 0.11% 17 117.9
2019 8,321 0.13% 16 98.5
2020 9,218 0.14% 15 84.6
VHA Priority Eligibility Groups
Veterans who apply for VHA care are assigned to 1 of 8 priority eligibility groups, which affect care costs.
151
Group status
is based on military service history, disability rating, income, Medicaid qualification and other factors.
150
Information is not presented when based on fewer than 10 suicide deaths. Note that suicide mortality is assessed for the year and the subsequent
year. For example, for the 2020 cohort, we assess suicide mortality in 2020 and in 2021.
151
https://www.va.gov/health-care/about-va-health-benefits/cost-of-care/ (Accessed 7/12/2023).

59
Table 7 presents unadjusted suicide rates per 100,000 person-years for annual cohorts of Veteran VHA Users, 2011–2021.
152
Table 7: Unadjusted Suicide Rates, Enrolled Recent Veteran VHA Users, by VHA Priority Eligibility Group,
2011–2021
Suicide Rate per 100,000 Priority Eligibility Group Criteria
2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
Group 1
36.1 39.4 38.3 39.5 41.8 38.8 38.8 39.7 40.3 39.9 40.2
Service-connected disability rated as 50% or more
disabling, or have service-connected disability that
makes one unable to work, or received the Medal
of Honor.
Group 2
31.9 33.1 28.6 32.3 27.7 30.1 29.1 33.7 29.5 33.5 32.6
Service-connected disability rated as 30% or
40% disabling.
Group 3
36.8 28.5 29.7 29.7 31.9 31.9 32.9 32.9 34.6 28.8 31.6
Former prisoner of war, or received the Purple
Heart medal, or were discharged for a disability
that was caused by — or got worse because of —
one’s active-duty service, or service-connected
disability rated as 10% or 20% disabling, or
awarded special eligibility classication under Title
38, U.S.C § 1151, "benets for individuals disabled
by treatment or vocational rehabilitation."
Group 4
25.5 41.5 24.9 43.0 45.3 48.7 37.8 39.0 42.2 44.9 38.7
Are receiving VA aid and attendance or
housebound benets, or received a VA
determination of being catastrophically disabled.
Group 5
51.7 47.9 49.7 51.3 49.4 51.2 52.5 48.9 51.6 52.0 57.1
Do not have a service-connected disability, or have
a non-compensable service-connected disability
rated as 0% disabling, and have an annual income
level below our adjusted income limits (based
on resident ZIP code), or receiving VA pension
benets, or eligible for Medicaid programs.
Group 6
23.7 20.0 17.4 23.0 25.1 21.1 25.7 32.3 28.8 33.3 36.4
Have a compensable service-connected disability
rated as 0% disabling, or exposed to ionizing
radiation during atmospheric testing or during
the occupation of Hiroshima and Nagasaki, or
participated in Project 112/SHAD, or served in
the Republic of Vietnam between 1/9/1962 and
5/7/1975, or served in Persian Gulf War between
9/2/1990 and 11/11/1998, or served on active duty
at Camp Lejeune 30+ days between 8/1/1953 and
12/31/1987. VA may also assign a Veteran to priority
group 6 if they meet all of the requirements listed
below. Veterans are: Currently or newly enrolled in
VA health care, and served in a theater of combat
operations after 11/11/1998, or were discharged
from active duty on or after 1/28/2003, and were
discharged less than 5 years ago.
153
Group 7
41.8 33.4 37.4 35.8 39.9 44.9 35.7 36.0 44.7 33.5 47.7
Gross household income is below the
geographically adjusted income limits (GMT) for
where one lives and agrees to pay copays.
152
https://www.va.gov/health-care/eligibility/priority-groups/ Group 8 refers to subgroups A-D. Group 8EG (non-enrolled) is not reported, due to small
numbers for most years. In 2021, Veteran VHA Users in Group 8EG had 12 suicides and a suicide rate of 33.1 per 100,000 person-years. Reporting does not
include Veterans whose eligibility was categorized as No Priority. Per the VA Enrollment System Administrative Data Repository.
153
Returning combat Veterans are eligible for these enhanced benefits for five years after discharge. At the end of this enhanced enrollment period,
VA assigns Veterans to the highest priority group they qualify for at that time.

60
Suicide Rate per 100,000 Priority Eligibility Group Criteria
2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
Group 8
33.1 35.5 41.3 37.9 37.9 39.3 38.9 36.4 41.2 46.2 43.0
Gross household income is above VA income
limits and geographically adjusted income limits
for where one lives, and agree to pay copays.
Eligibility for VA health care benets will depend
on subpriority group.
• Each year from 2005–2021, rates were highest for Veterans in Group 5, which includes income-based eligibility.
• In 2021, the suicide rate per 100,000 was highest for Group 5 (57.1 per 100,000), followed by groups 7 (47.7 per
100,000), 8 (43.0 per 100,000), 1 (40.2 per 100,000), 4 (38.7 per 100,000), 6 (36.4 per 100,000), 2 (32.6 per 100,000) and
3 (31.6 per 100,000).
• From 2020 to 2021, suicide rates increased for groups 1 (+0.8%), 3 (+9.7%), 5 (+9.8%), 6 (+9.5%) and 7 (+42.2%), and
rates fell for groups 2 (-2.7%), 4 (-13.8%) and 8 (-6.9%).
• For Groups 5, 6 and 7, the suicide rates in 2021 were higher than in any of the prior 20 years.
• Figure 26 provides rates by age group for Recent Veteran VHA Users in Priority Group 5, 2001–2021.
154
Veterans
between ages 18- and 34-years-old in Priority Group 5 had the lowest suicide rate in 2001 (40.8 per 100,000) and the
highest suicide rate in 2021 (82.8 per 100,000). From 2020 to 2021, the suicide rate increased 18.3% for those aged
18- to 34-years-old, 36.8% for those aged 35- to 54-years-old, 0.6% for those aged 55- to 74-years-old and 12.0% for
those aged 75-years-old and older.
Figure 26: Unadjusted Suicide Rate, Enrolled Recent Veteran VHA Users in Priority Group 5, by Age Group,
2001–2021
154
For all other priority groups, reporting is unavailable by age groups in these years due to small numbers.
2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
90
80
70
60
50
40
30
20
10
0
2020 2021
Rate per 100,000 Person-Years
18-34 55-74 75
+
35-54

61
Veteran All-Cause Mortality, Overall and by VHA Engagement
Figure 27 shows Veteran unadjusted all-cause mortality rates in the 3 years prior to the COVID-19 pandemic (2017–2019)
and in 2020 and 2021.
155
Understanding patterns of all-cause mortality over this period is helpful to understanding trends
in suicide risk factors, including medical morbidity and stressors, and patterns of risk across Veteran populations.
• All-cause mortality increased from 2017–2019 to 2020–2021.
• Consistent with reports of increased morbidity among Veterans who seek VHA care, all-cause mortality was greater
in all years for Recent Veteran VHA Users than for Other Veterans. These findings highlight the increased burdens
of morbidity and mortality among Veterans during the pandemic years and the greater morbidity and mortality
among Veterans who seek care from the VA health system.
Figure 27: Unadjusted All-Cause Mortality, Veterans, Overall and by VHA Engagement, 2017–2021
Similar patterns were observed with regard to age- and sex-adjusted all-cause mortality rates. For Veterans, these were
13.7% higher in 2020–2021 than in 2017–2019.
156
155
Unadjusted rates are presented here to document the magnitude of mortality increases in the pandemic years.
156
For Recent Veteran VHA Users, age- and sex-adjusted all-cause mortality rates were 13.7% higher in 2020–2021 than in 2017–2019, and for Other
Veterans, age- and sex-adjusted all-cause mortality rates were 13.0% higher in 2020–2021 than in 2017–2019.
Veterans Recent Veteran VHA Users Other Veterans
Rate per 100,000
0
500
1,000
1,500
2,000
2,500
3,000
3,500
4,000
20182017 2019
2020 2021

62
Leading Causes of Death, for Recent Veteran VHA Users and Other Veterans
Recent Veteran VHA Users
• Among Recent Veteran VHA Users in 2021, suicide was the 15th leading cause of death (Figure 28).
Figure 28: Top 10 Leading Causes of Death, and Suicide, in 2021, Recent Veteran VHA Users and Associated
Age-Adjusted Mortality Rates, 2019–2021
157
157
There is no comparison rate for 2019. COVID-19 deaths were identified based on underlying cause of death ICD-10 code U07.1, which was added as
a cause of death code in 2020.
0 100 200 300 400
(1) Heart Disease
(2) Cancer
(3) COVID-19
(5) Unintentional Injury
(6) Stroke
(7) Diabetes
(8) Alzheimer’s Disease
(9) Kidney Disease
(10) Parkinson’s Disease
(15) Suicide
(4) Chronic Lower Respiratory
Disease
Rate per 100,000
342.3
330.2
303.6
297.3
295.2
*
142.4
192.0
85.9
83.6
76.8
98.6
114.2
123.8
54.7
57.2
59.6
48.2
54.4
54.7
31.3
34.3
31.8
24.4
23.4
24.8
20.7
22.8
22.2
44.8
46.5
49.1
346.8
2019
2021
2020

63
Other Veterans
• Among Other Veterans in 2021, suicide was the 11th-leading cause of death (Figure 29).
Figure 29: Top 10 Leading Causes of Death, and Suicide, in 2021, Other Veterans and Associated Age-
Adjusted Mortality Rates, 2019–2021
158
• While sharing the same top 3 leading causes of death (heart disease, cancer, COVID-19), Recent Veteran VHA Users
and Other Veterans differed in the ranking of other leading causes of death.
• Despite suicide having a lower rank among leading causes for Recent Veteran VHA Users than for Other Veterans,
Recent Veteran VHA Users had a higher age-adjusted suicide mortality rate.
158
There is no comparison rate for 2019. COVID-19 deaths were identified based on underlying cause of death ICD-10 code U07.1, which was added as
a cause of death code in 2020.
2019
2021
2020
0 50 100 150 200 250
(1) Heart Disease
(2) Cancer
(3) COVID-19
(4) Stroke
(5) Chronic Lower Respiratory
Disease
(6) Unintentional Injury
(7) Alzheimer's Disease
(8) Diabetes
(9) Kidney Disease
(10) Parkinson’s Disease
(11) Suicide
Rate per 100,000
204.1
209.8
203.7
180.3
36.9
43.3
63.8
26.4
23.4
32.1
176.7
175.0
82.7
*
121.2
38.1
37.6
41.3
38.4
71.1
77.2
27.5
22.9
26.0
26.3
13.4
13.3
13.6
12.9
13.8
11.6
32.1
34.6

64
• For each of the leading causes listed, the age-adjusted mortality rate was greater among Recent Veteran VHA Users
than among Other Veterans.
159
For example, age-adjusted mortality rates in 2021 were:
Cause of Death Recent Veteran VHA Users Other Veterans
Heart disease 346.8 per 100,000 203.7 per 100,000
COVID-19 192.0 per 100,000 121.2 per 100,000
Unintentional injury 123.8 per 100,000 77.2 per 100,000
VA Community Care
Figure 30 presents unadjusted suicide rates among Veterans who received VHA direct care and Community Care
services
160
, by year, for 2020 and 2021.
161
• In both 2020 and 2021, suicide rates were highest for Veterans who received any Community Care services, followed
by Veterans who received any VHA care, and suicide rates were lowest among Veterans who did not receive either
Community Care or VHA care.
162
Figure 30: Unadjusted Suicide Rate, Veterans with Any Community Care and Veterans with Any VHA Care
163
in Year or Prior Year, 2020–2021
159
Differences may relate to greater prevalence of men among Recent Veteran VHA Users in older age groups than among Other Veterans. Among Recent
Veteran VHA Users aged 55-years-old and older, 93.5% were male, compared to 92.8% among Other Veterans aged 55-years-old and older.
160
Services receipt was measured by any care in the calendar year of interest or in the prior year.
161
The number of Veterans, by categories of receipt of VHA and VA Community Care in the year or prior year, were as follows for 2020 and 2021
(Counts are based on mid-year estimates.): Number of Veterans (Thousands)
2020 2021
VHA Direct Care Only 3,670 3,544
VHA Direct Care and Community Care 2,288 2,334
Community Care Only 94 111
Neither VHA Direct Care nor Community Care 13,225 12,851
162
The categories “Any Community Care” and “Any VHA Care” were not mutually exclusive.
163
Here and throughout this report, VHA care refers to VHA delivered care by VHA providers, also known as VHA direct care. Community Care refers to VA
purchased care. See: https://www.va.gov/COMMUNITYCARE/programs/veterans/CCN-Veterans.asp
2020 2021
Rate per 100,000
Neither VHA nor Community CareAny VHA CareAny Community Care
60
50
40
30
20
10
0

65
Figure 31 presents unadjusted suicide rates among Veterans by mutually exclusive categories of VHA direct care and VA
Community Care services receipt in the year or prior year, for 2020 and 2021.
In 2020 and 2021, among those receiving care through VHA, when comparing those solely receiving VA Community Care
services vs. those receiving VHA direct care services, Veterans who “received Community Care services only” had higher
suicide rates than those who “received VHA direct care alone.”
Figure 31: Unadjusted Suicide Rate, Veterans, by Mutually Exclusive Categories of VHA and VA Community
Care Services Receipt and for Any Community Care and Any VHA Care, by Year, 2020–2021
2020 2021
Rate per 100,000
60
50
40
30
20
10
0
VHA Only
Community Care Only
Community Care and VHA
Neither VHA nor Community Care

66
Veterans, by Receipt of VHA and VBA Services
Figure 32 presents the distribution of Veterans by categories of contact with VBA and VHA in the year or prior year, for
Veteran cohorts from 2019 to 2021.
164
• In 2021, nearly 6.9 million Veterans had some VBA contact, and over 5.8 million Veterans had some VHA contact in
2020 or 2021. This included over 1.9 million Veterans who only received VHA care (10.5%), over 3.0 million who only
received VBA services (16.0%) and nearly 3.9 million who received both VBA and VHA services (20.7%). In 2021, over
9.9 million Veterans (52.8%) had neither VBA nor VHA services in 2020 or 2021.
• From 2019 to 2021, the number of Veterans who received only VBA services in the year or prior year increased 12.7%,
the number receiving only VHA services fell by 14.0%, the number receiving both VBA and VHA services increased
by 0.5%, and the number receiving neither VBA nor VHA services decreased by 9.2%.
165
Figure 32: Number of Veterans, by Categories of VBA and VHA Contact
166
in the Year or Prior Year, 2019–2021
164
Analyses examined VBA data from 2018–2021, enabling assessment for 2019–2021.
165
From 2019 to 2021, the overall Veteran population fell 4.9%, from 19,817,000 to 18,841,000.
166
Counts are based on mid-year estimates.
2019 2020 2021
Number of Veterans
0
1,000,000
2,000,000
3,000,000
4,000,000
5,000,000
6,000,000
7,000,000
8,000,000
9,000,000
10,000,000
11,000,000
12,000,000
VHA and VBA
VHA Only VBA Only
Neither

67
Figure 33: Distribution of Veteran Population, Percentage, by VBA and VHA Contact
167
in Year or Prior Year,
2019–2021
167
Counts are based on mid-year estimates.
2019 2020 2021
Percentage
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
11.7%
19.5%
13.5%
55.3%
10.9%
20.0%
14.4%
54.7%
10.5%
20.7%
16.0%
52.8%
VHA and VBAVHA Only VBA Only
Neither

68
VBA Benefit Types Received, Percentage, Among Veterans with VBA Benefits,
2019–2021
Figure 34 provides information on types of VBA benefits received, for each of the 5 categories of VBA services, for cohorts
of Veterans who received some VBA services
168
in the year of interest or the prior year, for 2019–2021.
• In 2021, among VBA service recipients, most received VBA compensation and pension benefits (77.7%), followed
by home loan services (43.0%), educational benefits (9.2%), life insurance (5.6%) and Veteran Readiness and
Employment services (2.1%).
Figure 34: VBA Services Received,
169
Percentage, Veterans with VBA Services in Year or Prior Year,
2019–2021
168
https://benefits.va.gov/BENEFITS/about.asp. Also see description of VBA benefits, later in this report.
169
Veteran Readiness and Employment includes Chapter 31 benefit recipients, excluding those whose status at the beginning of the year was
“Applicant,” “Not Eligible,” “Rehabilitated,” “Interrupted” or “Discontinued.”
Percentage
Compensation
and Pension
Education Home Loan Life Insurance
Veteran Readiness
and Employment
2019 2020 2021
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
77.9%
37.5%
11.2%
2.0%
6.7%
79.1%
10.3%
2.2%
6.1%
77.7%
9.2%
43.0%
2.1%
5.6%
39.3%

69
Suicide Rates Among Veterans by Receipt of VBA or VHA Services
Figure 35 presents unadjusted suicide rates among Veterans by mutually exclusive categories of VHA and VBA services
receipt in the year or prior year, by year, from 2019 to 2021.
Suicide rates were highest among Veterans who only received VHA services, followed by those who received both VHA
and VBA services, then those who received neither VHA nor VBA services. Suicide rates were lowest among Veterans who
received VBA services and did not receive VHA services.
Figure 35: Unadjusted Suicide Rate, Veterans, by Mutually Exclusive Categories of VHA and VBA Services
Receipt,
170
by Year, 2019–2021
170
Suicide rates were calculated as the number of suicide deaths among individuals with that category of services receipt in the year or prior year,
divided by the mid-year population estimate of individuals with that category of services receipt, multiplied by 100,000.
2019 2020 2021
Rate per 100,000
0
5
10
15
20
25
30
35
40
45
50
VHA OnlyAll Veterans VHA and VBA
VBA Only Neither
44.1
37.7
32.7
30.4
25.0
30.4
22.8
22.4
32.6
33.9
33.0
37.5
38.5
47.2 47.3

70
Figure 36 presents age-adjusted suicide rates among Veterans who received VBA benefits, by sex and year, for 2019 to
2021. Consistent with overall Veteran suicide findings, rates were elevated among Veteran men compared to Veteran
women. Rates fell from 2019 to 2021 among Veteran men who had VBA engagement. Among Veteran women with VBA
engagement, age-adjusted suicide rates fell in 2020 and then rose in 2021 to levels comparable to those in 2019.
Figure 36: Age-Adjusted Suicide Rate, Veterans with VBA Benefits, by Sex and Year, 2019–2021
2019 2020 2021
Rate per 100,000
0
5
10
15
20
25
30
35
40
Male VeteransFemale Veterans

71
Suicide Decedents in 2021: Contacts with VHA and VBA
This section presents analyses regarding points of VA contact by Veteran decedents, including VHA health care
encounters, VHA enrollment and VBA contacts. We present findings for the 6,392 Veterans who died from suicide in
2021 (Figure 37).
Figure 37: Veteran Suicide Decedents in 2021, Sequential Mutually Exclusive Categories of VA Points of
Contact, Percentage and Average Suicides Per Day
171
171
Sequential mutually exclusive categories of VA points of contact are ordered from 1 to 5.
5. Veteran, no contact with
VHA or receipt of VBA benefits,
42.0%, 7.4 suicides per day
4. Veteran, any receipt of VBA
benefits in year of death or year prior,
4.1%, 0.7 suicides per day
3. VHA-enrolled Veteran, without VHA
encounters within past five years, 9.3%,
1.6 suicides per day
2. Veteran, had VHA encounter
within five years prior to death,
6.4%, 1.1 suicides per day
1. Veteran, had VHA encounter
in year of death or year prior,
38.1%, 6.7 suicides per day
17.5 Veteran Suicide Decedents per Day in 2021

72
Suicide Decedents, VBA Contact
Figure 38 shows the prevalence of VBA contact among annual cohorts of Veteran suicide decedents, 2019–2021. This rose
from 32.7% in 2019 to 33.9% in 2021.
Figure 38: VBA Contact in the Year or Year Prior, Percentage, Veteran Suicide Decedents, 2019–2021
Suicide Decedents with Recent VBA Contact, VBA Services Received
Figure 39: VBA Services Receipt, Percentage, Veteran Suicide Decedents with VBA Contact in the Year or
Year Prior to Death, 2019–2021
2019 2020 2021
40%
35%
30%
25%
20%
15%
10%
5%
0%
Percentage
32.7%
33.1%
33.9
2019 2020 2021
Percentage
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Compensation
or Pension
Home Loan
Veteran Readiness
and Employment
Education
Life Insurance

73
Suicide Decedents, Recent Veteran VHA Users with Behavioral Health Autopsy
Program Reviews
For Veterans, whose suicide deaths are reported to VHA suicide prevention teams,
172
the VA Behavioral Health Autopsy
Program (BHAP) gathers information that may help to prevent future suicides. Through BHAP, suicide prevention teams
perform standardized reviews of health records to identify factors relevant to Veteran suicides, considering all available
information.
173
VHA electronic health record reviews include assessment of clinical diagnoses and conditions (e.g., notes
regarding pain), life circumstances and psychosocial factors. Findings provide a unique resource for understanding the
characteristics and contexts of Veteran suicide deaths among Recent Veteran VHA Users.
174
Figure 40 presents the prevalence of documented risk factors in the year prior to death among 2,545 Recent Veteran VHA
Users whose suicide deaths occurred in 2019–2021 and were reported to VHA Suicide Prevention teams. Results are presented
in 5 domains, related to Risk Assessment, Stress, Interpersonal Factors, Death of Family or Friend and Health. The most
frequently identified risk factors were pain (55.9%), sleep problems (51.7%), increased health problems (40.7%), relationship
problems (33.7%), recent declines in physical ability (33.0%), hopelessness (30.6%) and unsecured firearms in the home (28.8%).
Figure 40: Documented Suicide Risk Factors, Percentage, Recent Veteran VHA Users Who Died by Suicide in
2019–2021 and Received BHAP Reviews
172
Palframan KM, Szymanski BR, McCarthy JF. 2021. Ascertainment of Patient Suicides by VA Facilities and Associations with Veteran, Clinical, and Suicide
Characteristics. American Journal of Public Health. 111(S2):S116-S125.
173
Sources include health records, coroner and medical examiner reports, death certificate records, reports from law enforcement agencies, media and
news outlets, and information shared by family members.
174
Caution should be exercised when drawing conclusions, as the absence of documentation of a characteristic does not necessarily indicate that the
Veteran did not experience the risk factor. It only indicates that no documentation of this risk factor was located within the medical chart or any other
available source of information.
0% 60%40% 50%30%20%10%
28.8%
30.6%
27.9%
17.1%
6.5%
6.3%
5.6%
3.8%
1.3%
24.7%
12.6%
11.5%
33.7%
55.9%
51.7%
40.7%
33.0%
17.9%
13.9%
9.1%
2.9%
10.9%
Risk Assessment
Stress
Interpersonal Factors
Death of Family or Friend
Health
Hopelessness
Unsecured Firearms in Home
Impulsivity/Poor Self-Control
Financial Loss
Legal Problems or Arrest
Risk of Homelessness
Relationship Problems
Alienation
Death of Family or Friend (past year)
Suicide of Family or Friend (past year)
Perceived Burden to Others
Recent Plan
Writing a Suicide Note
Other Preparatory Act
Recent Efforts to Acquire/Hide Lethal Means
History of Non-Suicidal Self-Harm
Giving Away Possessions
Pain in the Year Prior to Death
Sleep Problems
Increased Health Problems
Recent Decline in Physical Activity
Cognitive Decline

74
Reflecting Back, Looking Forward: Laying the Foundation for Future Courses of
Action for Suicide Prevention for VHA- and VBA-Engaged Veterans
Advance Suicide Prevention Meaningfully into Non-Clinical Support and
Intervention Services, Including Financial, Occupational, Legal and Social Domains
Multiple factors, in addition to mental health and clinical issues, contribute to Veterans being at increased risk for
suicide. For example, Veterans who have ever experienced homelessness are at increased risk for suicidal ideation,
suicide attempts and suicide deaths.
175
Similarly, housing instability (measured as concern over being able to pay rent
or a mortgage) is also associated with suicide. In 1 study, Veterans with past-year housing instability were 6 times as
likely as those who did not experience housing instability to report suicidal ideation.
176
Like homelessness, economic
and financial uncertainty are associated with suicide risk and increased distress, including during times of recession,
177
unemployment
178
and financial strain.
179
Additionally, disability status has been reported to be associated with suicidal
behaviors.
180
In contrast, Veterans in VHA care who have service-connected disability status benefits are less likely to die
by suicide when compared to those without a service-connected disability status.
181,182
VBA work in recent years in suicide
prevention is notable based on these findings. VA’s public health approach to suicide prevention includes interventions
targeting these issues, in addition to continuing its traditional clinical interventions within health care settings.
Beginning in 2023, VA Suicide Prevention expanded work with homelessness through developing improved methods for
enhancing suicide risk screening in homeless populations and Homeless Safety Planning in the Emergency Department
(SPED). Veterans who are homeless may be more likely to obtain care in emergency departments, and assessing suicide risk at
that time of engagement may improve the likelihood of early identification of suicide risk. VA also continues to fully focus on
meeting its 2023 goals for reducing homelessness. As of August 2023, VA has permanently housed 30,695 Veterans, on pace
to exceed its goal of housing 38,000 homeless Veterans in 2023. VA also announced at the end of August 2023, that it awarded
more than $1 billion in grants to help Veterans who are homeless and at risk of homelessness through the Supportive Services
for Veteran Families and Homeless Programs’ Grant and Per Diem Program. These grants are a critical part of VA’s efforts to
provide housing for Veterans in collaboration with the community. VA’s efforts to end Veteran homelessness are built upon the
evidence-based “Housing First” approach, which prioritizes getting a Veteran into housing and providing them with additional
services, including health care, job training, legal services, and education assistance, which also lower suicide risk overall.
175
Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. 2018. Suicidal Self‐Directed Violence Among Homeless US Veterans: A Systematic
Review. Suicide and Life‐Threatening Behavior 48(4):481–498.
176
Bossarte RM, Blosnich JF, Piegari RI, Hill LL, Kane V. 2013. Housing Instability and Mental Distress Among US Veterans. American Journal of Public
Health. 103(S2):S213–16.
177
Chang SS, Stuckler D, Yip P, Gunnell D. 2013. Impact of 2008 Global Economic Crisis on Suicide: Time Trend Study in 54 Countries. BMJ 347:f5239.
178
Haw C, Hawton K, Gunnell D, Platt S. 2015. Economic Recession and Suicidal Behaviour: Possible Mechanisms and Ameliorating Factors.
International Journal of Social Psychiatry 61(1):73–81.
179
Blosnich J, Montgomery A, Dichter M, et al. 2019. Social Determinants and Military Veterans’ Suicide Ideation and Attempt: A Cross-Sectional
Analysis of Electronic Health Record Data. Journal of General Internal Medicine.
180
Fässberg MM, Cheung G, Canetto SS, Erlangsen A, Lapierre S, Lindner R, Draper B, Gallo JJ, Wong C, Wu J, Duberstein P, Waern M. 2016. A Systematic
Review of Physical Illness, Functional Disability, and Suicidal Behaviour Among Older Adults. Aging and Mental Health. 20(2):166-194. https://doi.org/10.1
080/13607863.2015.1083945.
181
McCarthy JF, Bossarte RM, Katz IR., Thompson C, Kemp J, Hannemann CM, Nielson C, Schoenbaum M. 2015. Predictive Modeling and Concentration of
the Risk of Suicide: Implications for Preventive Interventions in the US Department of Veterans Affairs. American Journal of Public Health. 105(9):1935-
1942. https://doi.org/10.2105/AJPH.2015.302737
182
Dobscha SK, Denneson LM, Kovas AE, Teo A, Forsberg CW, Kaplan MS, Bossarte R, McFarland BH. 2014. Correlates of Suicide Among Veterans Treated in
Primary Care: Case-Control Study of a Nationally Representative Sample. Journal of General Internal Medicine. 29(S4):853–860. https://doi.org/10.1007/
s11606 - 014 -3028-1.

75
VA is launching the National Veterans Financial Resource Center, funded by VA Suicide Prevention. The center is focused
on addressing the challenges of financial strain in Veterans at risk of suicide and will provide Veterans access to education,
tools, and resources to successfully navigate challenges to financial wellness and, thereby, reduce risk of suicide. VA is
finalizing a website and mobile platform enabling Veterans to select their own financial goals. They will be able to link
to local and national financial resources, including housing counselors, legal aid, credit and financial counseling, job
centers and food banks. Veterans will also be able to link to short videos, interactive learning, and decision tools (e.g.,
creating spending plans, managing debt, taking out a car loan, lowering utility bills). Currently, hiring is underway for
a consultation hub, which will provide consultation and financial tools/resources to VA clinicians for the Veterans they
serve. Additionally, VA staff will have access to financial resource tools to support Veterans, including a SharePoint site,
consultation services and local financial health champions. In 2023, VA is expanding outreach to justice-involved Veterans
through the Veterans Justice Program (VJP) positions, with 86.5 full-time-equivalent (FTE) employees provided across
the Nation. Incarceration is both a significant predictor of homelessness and a risk factor for suicide. Adding more VJP
positions in the field will enable VA to support more Veteran Treatment Courts and conduct outreach to Veterans in more
local jails and other criminal justice settings during times of heightened risk for homelessness and suicide. VA is also
expanding access to legal support services by building upon and expanding its current 28 Medical-Legal Partnerships.
VA awarded 75 grants under its new Legal Services for Homeless Veterans and Veterans at Risk for Homelessness (LSV-H)
program to provide legal services to Veterans who are homeless or at risk of homelessness.
VBA continues to provide significant upstream approaches for suicide prevention through the provision of a variety
of benefits and services to reduce economic and financial drivers of suicide risk. These include programs such as Solid
Start, Disability Compensation, Pension, Veteran Readiness and Employment (VR&E) and Education/GI Bill assistance, to
facilitate successful transitions to civilian life. Additional VBA supports include:
• Services to promote connections to caregiver supports and protect financial wellness:
• VBA provides need-based benefits to Veterans and their survivors. This includes tax-free, income-based
benefits for wartime Veterans who are permanently and totally disabled (or are aged 65 or older) and their
eligible survivors.
• Seriously disabled Veterans and their eligible survivors may qualify for increased benefits if they need the
aid and attendance of another person or are housebound. The Fiduciary Program oversees appointment of
fiduciaries for VA beneficiaries unable to manage their VA benefits as a result of injury, disease, advanced age
or those less than 18 years of age.
• VBA provides monthly monetary benefits to Veterans in recognition of the enduring effects of disabilities,
diseases or injuries incurred or aggravated during active military service. Monthly tax-free benefits are paid to
eligible Veterans with service-related disabilities.
• Services to support military transition and promote connections to educational supports and other social
institutes to facilitate attainment of educational objectives, connection to means for achieving career ambitions
and assistance in translating military-related skills to marketable occupational interests to foster financial security,
connection, purpose, and personal drive:
• VA Solid Start (VASS) provides caring contact to newly separated Veterans at 90-, 180- and 365-day check-in
points, post-separation. VA representatives help to navigate connections to VA and community-care resources.
• Outreach, Transition and Economic Development (OTED) provides transition assistance, Military to Civilian
Ready Framework, economic development initiatives, outreach, and personalized career planning guidance.
This program also provides information and resources to facilitate employment, special hiring authorities,
career support resources and financial tools through collaborations with the Department of Labor,
Department of Defense, and others.
• Services to promote financial independence, stabilizing housing, and assistance to navigate threats to housing and/
or food insecurity:
• VA Home Loan Guaranty helps Service members, Veterans and their families obtain and retain a home
(including supports to augment or refinance an existing home).

76
• Services to facilitate life skills training, employment, and educational opportunities:
• Veteran Readiness and Employment (VR&E) provides Veterans with service-connected disabilities case
management and job counseling to facilitate successful employment (including job training, resume
development, skills for job-seeking and work-readiness assistance).
• VBA offers educational benefits to advance the educational and career aspirations of Veterans, Service
members, family members and survivors.
Reection: Non-Clinical Services
Summary: A number of non-mental health and non-clinical risk factors are present for suicide including homelessness,
nancial instability, unemployment, justice involvement and more. Findings from this year’s report indicate that we
must move beyond the clinical to assist Veterans in services to address these risk factors to reduce Veteran suicide.
What You Can Do: Connect Veterans with job-search and skill-building resources. VA oers career and employment
resources. Consider connecting Veterans with a Health Care for Reentry Veterans Specialist who can provide
resources and direct Veterans to community or legal assistance or with VA’s Veterans Justice Outreach (VJO). VJO
works with local criminal justice partners to connect Veterans with resources. Save this number in your phone for
the National Call Center for Homeless Veterans that can assist any Veteran who is homeless or at imminent risk for
becoming homeless. You can contact the National Call Center for Homeless Veterans at (877)4AID-VET or (877)424-3838.
Increase Access to and Utilization of Mental Health Services Across a Full
Continuum of Care
Mental health and SUD remain a risk factor for suicide in
the Veteran population. As such, advancing access for a
full continuum of mental health care is vital for reducing
suicide for those for whom mental health treatment is
needed. Additionally, increases in mental health staffing
have been associated with decreases in suicide rates for
VHA patients.
183
Investing in expansion of mental health
services for Veterans is an important component of VA’s
National Strategy for Preventing Veteran Suicide (2018).
VA continued, in 2023, growth of SP 2.0 Clinical Telehealth,
reaching all VA health care systems in less than 2 years
of implementation by leveraging 100 highly trained
specialized therapists. Ninety percent of this staff have
been trained in 3 or more EBPs for suicide prevention. As
of August 31, 2023, the program processed over 12,350
Veteran referrals. In August 2023 alone, VA was on track
to exceed another intake volume record, having already
completed over 400 intake appointments. VA is also hearing from Veterans and referring providers about the lifesaving
work of the program (see qualitative feedback in the call-out box). VA also continues to exceed all performance metrics
on the Recovery Engagement and Coordination for Health — Veterans Enhanced Treatment (REACH VET) Program.
183
Katz IR, Kemp JE, Blow FC, McCarthy JF, Bossarte RM. 2013. Changes in Suicide Rates and in Mental Health Staffing in the Veterans Health
Administration, 2005–2009. Psychiatric Services. 64:620–625.
Intensity of Services
Self-Directed Care, Peer Support, Community Partnerships, Crisis Services
Whole Health System of Care
Mental Health Continuum of Care
Primary Care Mental Health Integration (PCMHI)/PACT
General Mental Health (Behavioral Health
Interdisciplinary Program/BHIP)
Specialty Mental Health
Residential
Inpatient

77
Within 2023, in alignment with the White House Strategy on
Reducing Military and Veteran Suicide (2021), VA funded a
National Academies of Sciences, Engineering, and Medicine
(NASEM) public workshop on Improving Access to High-Quality
Mental Health Care for Veterans, to explore methods for
expansion of access to services for Veterans. This included
addressing the need for access across 3 areas:
184
urgent/crisis
access (e.g., need/want an appointment now, crisis services);
engagement access (e.g., when someone is first initiating
treatment); and sustained access (e.g., ongoing access to
treatment — for evidence-based psychotherapy for 12- to
16-weeks of individual therapy with the same provider). All 3
types of access are necessary for continuity of mental health
care. When we provide initial/engagement or emergent/urgent
access, without sustained access, we are not providing quality,
evidence-based care. The NASEM forum provided an
opportunity to discuss the need for both access and quality to
move the needle in mental health treatment as part of suicide
prevention efforts in implementing the full continuum of
mental health care. While not all those who die by suicide have
a mental health or SUD, we know that mental health and SUD
are pertinent risk factors for suicide for many Veterans, and the
delivery of evidence-based treatments for mental health have
demonstrated the ability to reduce suicide.
185
With the
publication of the NASEM report, VA will move forward in
identifying other access-to-care models from SAMHSA, national
associations, and international health care systems and
statistically test the models using synthetic data to determine
which is best for access, evaluating which models of access
minimize wait times, provide critical access to rapid
engagement and provide optimal episode-of-care access. VA will test the models with movement forward for pilot
implementation across several VISNs to assess for best improvements in mental health access across the continuum of care.
Along these lines, in FY 2024, VA will advance a full hiring initiative for mental health with an expanded focus on growing the
mental health pipeline, including suicide prevention coordinators (SPC). Growth in mental health staffing is particularly
important to suicide prevention as higher levels of mental health staffing have been associated with decreased suicidal
behavior among patients within a health care system.
186,187,188
This continues to build off the expansion of general mental
health interdisciplinary team staff funding from suicide prevention to add 172 staff across the Nation.
184
Known as “tripartite access” in VA.
185
National Institute of Mental Health (2021) Treatment and Therapies for Suicide. Available at: NIMH » Suicide Prevention (nih.gov).
186
Atkinson JA, Page A, Heffernan M, McDonnell G, Prodan A, Campos B, Meadows G, Hickie IB. 2019. The Impact of Strengthening Mental Health
Services to Prevent Suicidal Behavior. Aust N Z J Psychiatry. 53(7):642-650.
187
Katz IR, Kemp JE, Blow FC, McCarthy JF, Bossarte RM. 2013. Changes in Suicide Rates and in Mental Health Staffing in the Veterans Health
Administration, 2005–2009. Psychiatric Services. 64: 620-625. doi: 10.1176/appi.ps.201200253.
188
Feyman, Y, Figueroa, SM, Yuan, Y, Price ME, Kabdiyeva A, Nebeker JR, Ward MC, Shafer PR, Pizer SD, Strombotne KL. 2022. Effect of Mental Health
Staffing Inputs on Suicide-Related Events. Health Services Research. 1-8. doi:10.1111/1475 - 6773.14 064.
Suicide Prevention 2.0 Clinical
Telehealth Feedback
Feedback from Veterans:
• “I would not be alive today if not for
this program.”
• “For the first time in my life, I don’t want
to die anymore. I never thought I would
feel that way.”
• “Suicide wasn’t something that I was
looking forward to talking openly about.
I was surprised at how comfortable I felt
within the first session and appreciated
the ability to meet individually from the
comfort of my home.”
Feedback from Referring Providers:
• “I was skeptical about the program at
first. But after a couple of my Veterans
went through it, I saw the benefit. They
made so much progress in ways that
we hadn’t been able to address in our
regular therapy. This is a great program
and has helped so many Veterans!”

78
Reection: Access to Mental Health Services
Summary: Both mental health and SUDs are risk factors for Veteran suicide. Obtaining prompt access to services is
critical not only during times of crisis, but when rst initiating treatment, and in a sustained manner to complete a
full episode of care.
What You Can Do: Connect Veterans with information on how to obtain same-day mental health services by visiting
this website. Save the VCL number in your phone (Dial 988 then Press 1) and spread the word about VCL through
your community connections. Link Veterans to information about the mental health and SUD services available to
them. If you are not sure about how to talk with a Veteran about available services, reach out to Coaching into Care, a
free service for families and friends of Veterans where you can learn about resources and referrals.
Integrate Suicide Prevention Within Medical Settings to Reach All Veterans
Nearly 40% of Recent Veteran VHA Users who died by suicide in 2021 did not have a mental health or SUD diagnosis.
Many Veterans will also never seek mental health treatment. Further, medical conditions, including those lasting 1 year
or more, can increase an individual’s risk for suicidal behavior.
189,190
For example, individuals diagnosed with cancer have
approximately 1.5 times the general population’s risk for suicide death, while patients with a poor prognosis have 3
times the risk for suicide death than cancer patients overall.
191,192
Likewise, there is a strong association between chronic
pain and suicide.
193
Further, prior research has shown that 45% of individuals who die by suicide have had a primary care
appointment in the prior month.
194
Thus, incorporation of suicide prevention into medical settings is a critical part of VA’s
public-health approach to address Veteran suicide.
VA continues to expand its efforts in suicide prevention in medical settings. As part of SP Now Clinical Interventions, VA
continued implementation of SPED, which is an evidence-based practice shown to reduce suicidal behaviors by 45%.
195
The program promotes safety planning with Veterans who present to the emergency department with suicidal ideation,
providing follow-up contact until treatment engagement occurs. VA is now exceeding the target on the lifesaving efforts
of SPED. Ongoing implementation of population-based suicide risk screening is underway for those with unrecognized
risk (universal), for those who may be at risk (selected) and for those at elevated risk (indicated) through VA’s Suicide
Risk Identification Strategy (Risk ID), founded in the strong evidence outlined in the clinical practice guideline.
196
Risk ID
isimplemented across settings, including ambulatory care and emergency departments, which is assisting in identifying
189
Zhu J, Xu L, Sun L, et al. 2018. Chronic Disease, Disability, Psychological Distress and Suicide Ideation among Rural Elderly: Results from a
Population Survey in Shandong. International Journal of Environmental Research and Public Health 15, no. 8:1604.
190
Wei MY, Mukamal KJ. 2019. Multimorbidity and Mental Health‐Related Quality of Life and Risk of Completed Suicide. Journal of the American
Geriatrics Society. 67(3):511–519.
191
Amiri S, Behnezhad S. 2019. Cancer Diagnosis and Suicide Mortality: A Systematic Review and Meta-Analysis. Archives of Suicide Research. 0:1-19.
192
Dent KR, Szymanski BR, Kelley MJ, Katz IR, McCarthy JF. 2023. Suicide Risk following a New Cancer Diagnosis among Veterans in Veterans Health
Administration Care. Cancer Medicine.12(3):3520-3531.
193
Ilgen, M. 2018. Pain, Opioids, and Suicide Mortality in the United States. Annals of Internal Medicine 167(7):498-499.
194
Luoma JB, Martin CE, Pearson JL. 2002. Contact with Mental Health and Primary Care Providers Before Suicide: A Review of the Evidence. American
Journal of Psychiatry. 159:909-916. doi: 10.1176/appi.ajp.159.6.909.
195
Stanley B, Brown GK, Brenner LA, Galfalvy HC, Currier GW, Knox KL, Chaudhury SR, Bush AL, Green KL. 2018. Comparison of the Safety Planning
Intervention with Follow-Up vs Usual Care of Suicidal Patients Treated in the Emergency Department. JAMA Psychiatry. 75(9):894-900.
196
Department of Veterans Affairs and Department of Defense. 2019. VA/DoD Clinical Practice Guideline for the Assessment and Management of
Patients at Risk for Suicide.
https://www.healthquality.va.gov/guidelines/MH/srb/VADoDSuicideRiskFullCPGFinal5088212019.pdf

79
individuals at risk for suicide not receiving mental health treatment.
197
The identification of suicide risk as part of RISK ID
was associated with increased mental health treatment follow-up, particularly for those Veterans not previously engaged
in mental health services in the prior year.
198
Suicide risk screening continues to improve in medical settings, including
a 7% improvement in primary care, 13% improvement in specialty medicine, 31% improvement in audiology, 15%
improvement in Primary Care - Mental Health Integration (PCMHI) and 10% improvement in women’s health clinic from
October 2021 to July 2023. Related to advancement of naloxone for Opioid Use Disorder, VA expanded this effort in FY
2022 to also include Veterans diagnosed with Stimulant Use Disorder. This effort resulted in a 12% increase in naloxone
prescriptions dispensed to Veterans diagnosed with Opioid Use Disorder (from 61.5% of Veterans to 69%) and a 56%
increase in naloxone prescriptions for Veterans with Stimulant Use Disorder diagnoses (from 29% of Veterans to 45%).
Reection: Suicide Prevention in Medical Settings
Summary: Nearly 40% of Veterans who died by suicide had no mental health or substance use disorder diagnoses.
Other medical conditions are also associated with higher risk for suicide (e.g., chronic pain, cancer, insomnia and more).
What You Can Do: Check in with Veterans who are struggling with medical conditions, including those who are
dealing with a newly diagnosed condition. Encourage connection to additional methods of support including VA’s
Whole Health Program, and VA mobile apps and online tools. If you work in community-care settings, promote
discussion about secure rearm storage with patients, encourage community-care providers to take training in lethal
means safety with these courses with free continuing education (e.g., an hour long version and a briefer 25-minute
version and promote gun lock distribution in clinic waiting areas.
SP Now efforts grew to specifically target methods to expand access to support services within other medical clinics,
particularly reviewing options for expansion in oncology clinics, pain clinics and primary care settings. VA’s focus on
PCMHI, embedding mental health providers directly into primary care, has been particularly successful in increasing odds
of engagement in mental health treatment, reducing wait times for services and decreasing no-show rates for mental
health appointments.
199,200,201,202
VA Suicide Prevention supported expansion of PCMHI with the addition of 129 PCMHI
staff across the Nation to support ongoing suicide prevention efforts. In addition to PCMHI, integrated services have been
extended to Pain and Oncology clinics to proactively identify risk and engage supports and resources same-day through
funding by VA Suicide Prevention, as part of FY 2022 funding. Through August 2023, this has included expansion of 58
mental health integration providers in Pain Clinics in 44 unique VA facilities and 32 mental health integration providers
in Oncology Clinics in 27 unique VA facilities. Additionally, Suicide Prevention worked with Primary Care to pilot a Lethal
Means Safety competency-based training to primary care team members in 1 VISN, to support discussions about secure
197
Bahraini N, Brenner LA, Barry C, Hostetter T, Keusch J, Post EP, Kessler C, Smith C, Matarazzo BB. 2020. Assessment of Rates of Suicide Risk Screening
and Prevalence of Positive Screening Results Among US Veterans After Implementation of the Veterans Affairs Suicide Risk Identification Strategy.
JAMA Network Open. 2020;3(10):e2022531. doi:10.1001/jamanetworkopen.2020.22531.
198
Bahraini N, Reis DJ, Matarazzo BB, Hostetter T, Wade C, Brenner LA. 2022. Mental Health Follow-Up and Treatment Engagement Following Suicide
Risk Screening in the Veterans Health Administration. PloS One. 17(3):e0265474.
199
Brawer PA, Martielli R, Pye PL, Manwaring J, Tierney A. 2010. St. Louis Initiative for Integrated Care Excellence (SLI2CE): Integrated-Collaborative
Care on a Large Scale Model. Families Systems Health. 28:175–87. doi: 10.1037/a0020342.
200
Pomerantz A, Cole BH, Watts BV, Weeks WB. 2008. Improving Efficiency and Access to Mental Health Care: Combining Integrated Care and
Advanced Access. General Hospital Psychiatry. 30:546–51. doi: 10.1016/j.genhosppsych.2008.09.004.
201
Pomerantz A, Shiner B, Watts BV, Detzer MJ, Kutter C, Street B, et al. 2010. The White River Model of collocated collaborative care: a platform for
mental and behavioral health care in the medical home. Families Systems Health. 28:114–29. doi: 10.1037/a0020261.
202
Wray LO, Szymanski BR, Kearney LK, McCarthy JF. 2012. Implementation of Primary Care-Mental Health Integration Services in the Veterans Health
Administration: Program Activity and Associations with Engagement in Specialty Mental Health Services. J Clin Psychol Med Settings. 19:105–16.
doi: 10.1007/s10880-011-9285-9.

80
firearm storage within their daily work. Further, VA funded 300 virtual reality headsets for chronic pain intervention with
a customizable chronic pain environment for a 60-site pilot in 2022, to provide a method for Veterans to apply evidence-
based interventions for pain treatment based in Veterans’ homes. Finally, VA’s Outreach to Facilitate Return to Care pilot
program identifies and targets outreach to Veterans who were previously engaged in VHA care but had not been seen in the
last 2 years and as of their last VHA encounter were at high risk for suicide per the REACH VET algorithm. Program evaluation
analyses indicate that eligible patients in current or former pilot facilities were more likely to engage in VHA mental health
services than those at other facilities. VA is working to expand the ongoing pilot program.

81
Conclusion
As we look back at 2021, we continue to be guided by our 3 core tenets of suicide prevention. 2021 humbled the Nation
as we faced significant challenges, reminding us again that suicide is a complex interweaving of issues and concerns.
Suicide has no 1 cause and, because of this, has no 1 solution. From all our research efforts with you across the Nation, we
know there are some interventions that reduce suicide, suicidal thoughts and/or suicide attempts: evidence-based
psychotherapies like Cognitive Behavioral Therapy for Suicide Prevention, Problem Solving Therapy for Suicide
Prevention, Dialectical Behavioral Therapy for Suicide Prevention,
203
safety planning in the emergency department,
204
REACH VET,
205
secure storage of firearms,
206
crisis line interventions
207,208
and more. Yet, the majority of these interventions
are still clinical in nature and primarily in mental health settings, leaving untouched the problems fueling suicide at a
broader scale outside of mental health (e.g., medical concerns like chronic pain and cancer, economic worries,
homelessness, relationship issues). Further, suicide is not just a mental health problem, as evidenced by the fact that
nearly 40% of Recent VHA Users who died by suicide in 2021 had no mental health or substance use disorder diagnosis.
This leaves us with 2 critical pathways forward: 1) continue full
force implementation of what we know from the research to
save lives and 2) encourage ongoing innovation/research paired
with strong program evaluation to assess for new effective
interventions (e.g., SP 2.0 CBI-SP, Mission Daybreak). These
2 pathways are guided by the 7 core themes revealed in the
data from 2021 focused on secure firearm storage, community
prevention, expanding crisis intervention, adaptation efforts
for diverse subpopulations, addressing broader sociocultural
suicide risk factors, improving mental health access across a
continuum of care and moving suicide prevention into all clinical
settings. To reach all Veterans, we need all of you across all levels
of government, Veterans Service Organizations, community organizations, and the Nation. We have outlined with each of
the 7 themes, potential ways anyone can help support Veterans and we invite your participation in all the outlined efforts
we at VA will be taking in 2023 and beyond. Anchored in hope, we move forward together with each of you, knowing we
have much yet to learn, but fueled by the knowledge that we can make a difference in the lives of Veterans around us.
203
Department of Veterans Affairs and Department of Defense. (2019). VA/DoD Clinical Practice Guideline for the Assessment and Management of
Patients at Risk for Suicide. https://www.healthquality.va.gov/guidelines/MH/srb/VADoDSuicideRiskFullCPGFinal5088212019.pdf
204
Stanley B, Brown GK, Brenner LA, Galfalvy HC, Currier GW, Knox KL, Chaudhury SR, Bush AL, Green KL. 2018. Comparison of the Safety Planning
Intervention with Follow-Up Vs Usual Care of Suicidal Patients Treated in the Emergency Department. JAMA Psychiatry. 75(9):894-900.
205
McCarthy JF, Cooper SA, Dent KR, Eagan AE, Matarazzo BB, Hannemann CM, Reger MA, Landes SJ, Trafton JA, Schoenbaum M, Katz IR. 2021.
Evaluation of the Recovery Engagement and Coordination for Health - Veterans Enhanced Treatment Suicide Risk Modeling Clinical Program in the
Veterans Health Administration. JAMA Network Open. 4(10), e2129900.
206
Mann JJ, Michel CA, Auerbach RP. 2021. Improving suicide prevention through evidence-based strategies: A systematic review. The American
Journal of Psychiatry
, 178(7), 611–624.
207
Johnson LL, Muehler T, Stacy MA. 2021. Veterans’ satisfaction and perspectives on helpfulness of the Veterans Crisis Line. Suicide and Life-
Threatening Behavior, 51(2), 263–273. ht t ps ://doi.org /10.1111/sltb.12702
208
Britton PC, Karras E, Stecker T, Klein J, Crasta D, Brenner LA, Pigeon WR. 2022. Veterans Crisis Line Call Outcomes: Distress, Suicidal Ideation, and
Suicidal Urgency. American Journal of Preventive Medicine, 62(5), 745–751. https://doi.org/10.1016/j.amepre.2021.11.013
Core Tenets
1. Suicide is preventable.
2. Suicide prevention requires a public
health approach combining clinical
and community-based approaches.
3. Everyone has a role to play in
suicide prevention.

82
To refer to this report, please use the following citation:
U.S. Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. 2023 National Veteran Suicide
Prevention Annual Report. 2023. Retrieved {date} from <<location>>.

83
Appendix A: Brief Summary of 2021 VA Suicide
Prevention Initiatives
1. Veterans Crisis Line (VCL) 988 Preparation: Within 2021, significant preparations were underway by the
Substance Abuse and Mental Health Services Administration (SAMHSA) and VA to ensure readiness for 988
implementation, including extensive hiring, technology infrastructure modernization and expansion of quality
assurance and training. Within FY 2021, demand for VCL services grew (e.g., a 2.3% increase in calls offered, a 27.9%
increase in texts, and a 25.4% increase in chat compared to FY 2020 daily averages). Simultaneously, VCL saw a
23.3% reduction in abandonment rate and a 6.6% reduction in average time to answer (average speed of answer 9
seconds). VCL further expanded services with the launch of its Peer Support Outreach Center (PSOC), In alignment
with growing peer specialist suicide prevention efforts.
209
2. VA’s Suicide Prevention 2.0 (SP 2.0) Clinical Telehealth: The SP 2.0 Clinical Telehealth Program is the first and
only enterprise-wide fully virtual program offering evidence-based therapy for suicide prevention
210
for Veterans
with a recent history of suicidal self-directed violence. The earlier decision to launch the SP 2.0 clinical program
in a telehealth model aided the expansion of evidence-based therapies for suicide prevention across the Nation,
especially during a time when Veterans were less likely to come to in-person visits.
211
During 2021, VA continued to
move forward on its hiring goal of 100 providers to serve Veterans.
3. SP 2.0’s Community-Based Intervention for Suicide Prevention (CBI-SP) Growth: The majority of Veterans
who died by suicide in 2021 were not recently engaged in VHA services or VBA benefits. To reach all Veterans, VA
expanded SP 2.0 CBI-SP, growing community coalitions focused on ending Veteran suicide, including through
the joint VA and SAMHSA Governor’s Challenge initiatives and work by regional Community Engagement and
Partnerships Coordinators (CEPC). These community-based strategies are supported by prior work in community
prevention science and programs, combining health promotion, upstream approaches and a focus on improved
clinical and crisis-care delivery through collaboration.
212,213,214
By the end of 2021, 35 states and territories were active
members in the Governor’s Challenge and a total of 184 coalitions were developed.
4. Staff Sergeant Parker Gordon Fox Suicide Prevention Grant Program (SSG Fox SPGP) and Mission Daybreak
Development: The SSG Fox SPGP enables VA to provide resources toward community-based suicide prevention
efforts to meet the needs of Veterans and their families through outreach, suicide prevention services and connection
to VA and community resources. After the Commander John Scott Hannon Veterans Mental Health Care Improvement
Act of 2019 was signed into law on October 17, 2020, VA began the active implementation of the development of the
209
Pfeiffer PN,King C,Ilgen M,Ganoczy D,Clive R,Garlick J,Abraham K,Kim HM,Vega E,Ahmedani B, Valenstein M.2019.Development and Pilot
Study of a Suicide Prevention Intervention Delivered by Peer Support Specialists.Psychological Services. 16(3):360–371.https://doi.org/10.1037/
ser0000257
210
The treatments include Cognitive Behavioral Therapy for Suicide Prevention, Problem Solving Therapy for Suicide Prevention, Dialectical
Behavioral Therapy, and Advanced Safety Planning.
211
Department of Veterans Affairs and Department of Defense. 2019. VA/DoD Clinical Practice Guideline for the Assessment and Management of
Patients at Risk for Suicide. https://www.healthquality.va.gov/guidelines/MH/srb/VADoDSuicideRiskFullCPGFinal5088212019.pdf
212
Frieden TR. 2014. Six Components Necessary for Effective Public Health Program Implementation. American Journal of Public Health. 104(1):17-22.
213
Lai C, Law YW, Shum AK, Ip FW, Yip PS. 2020. A Community-Based Response to a Suicide Cluster: A Hong Kong Experience. Crisis: The Journal of
Crisis Intervention and Suicide Prevention. 41(3):163-171.
214
Oyama H, Watanabe N, Ono Y, Sakashita T, Takenoshita Y, Taguchi M, Takizawa T, Miura R, Kumagai K. 2005. Community‐Based Suicide
Prevention Through Group Activity for the Elderly Successfully Reduced the High Suicide Rate for Females. Psychiatry and Clinical Neurosciences.
59(3):337-344.

84
program, laying the foundation for its awarding of grants in FY 2022. Additionally, in 2021, VA began planning the FY
2022 launch of Mission Daybreak, a $20 million grand challenge to reduce Veteran suicides. This effort included a call
to innovators to develop suicide prevention solutions that meet the diverse needs of Veterans. Both of these programs
were critical for engaging the community in bringing solutions to Veteran suicide prevention.
5. Expansion of Special Population Suicide Prevention Efforts: Attending to the needs of age-specific, gender-
specific and race and ethnicity-specific populations with communication, outreach and intervention is critical for
Veteran suicide prevention efforts. Within 2021, VA worked to expand communication campaigns for targeted
diverse populations through 3 of its campaigns, Don’t wait. Reach out., Keep It Secure and VCL. Campaigns were
designed to reach the most diverse populations with a significant investment in purchasing airtime slots and
channels that demonstrate higher market shares representative of Black, Hispanic, Native American, Asian/Pacific
Islander, female populations, younger Veterans, transitioning Veterans and Veterans aged 55 and older utilizing
a data-driven approach and awide variety of advertising platforms.
215
In 2021, VA focused extensively on the
development of DEI consideration in its local community coalition development, including implementation of a
toolkit for CEPCs to integrate DEI in all aspects of community work and in educating Governor’s Challenge state
teams and local coalitions on how to successfully engage with Tribal Partners as part of their landscape analysis
and action planning.
216
Research and innovation are critical parts of addressing the needs of diverse Veteran
subpopulations. VA Health Services Research & Development (HSR&D) has led the effort to include and expand
research on women Veterans. The VA Women’s Health Research Network (WHRN) has significantly expanded
research in suicide prevention, particularly through its Women Veterans Suicide Prevention Research Work Group.
In February 2021, HSR&D and WHRN facilitated the publication of a supplement within the journal, Medical Care,
focused on “Advancing Knowledge of Suicide Risk and Prevention among Adult Women.”
217
In 2021, VA Suicide
Prevention also expanded funding of demonstration projects focused on diverse populations. One example is
the joint effort between the Rocky Mountain Mental Illness Research Education and Clinical Center (MIRECC) and
the Office of Rural Health (ORH) to address Native Veteran Suicide Prevention focused on developing effective
collaboration with tribal communities in creating a learning community of VA and tribal partners, adapting suicide
prevention training and developing processes and tools for enhancing culturally appropriate engagement.
Additionally, VA Suicide Prevention launched funding for Rocky Mountain MIRECC efforts in “Understanding Suicide
Risk and Enhancing Suicide Prevention among Asian American and Pacific Islander Veterans.” This project seeks to
obtain novel information to prevent suicide among Asian American and Pacific Islander (AAPI) Veterans, including
initial research on needs within the population with culmination of the development of culturally relevant suicide
prevention resources and interventions for implementation.
215
Advertising assets were tailored with photography and messaging aligned to each subpopulation with input directly from Veterans, as well as
experts from the Center for Minority Veterans, Women Veterans Health Program Office, LGBTQ+ Office, Veterans Experience Office, and Veterans
Service Organization liaisons, which assist with reflecting the diverse populations of Veterans served. Examples of more age-specific targeted
outreach, reflective of a racially and ethnically diverse population, include the Don’t wait. Reach out. “Battle Buddy” video or Keep It Secure “Space
Between Thought and Trigger” targeting older Veteran populations, or the Don’t wait. Reach out. “Women Veterans” video or Keep It Secure “Space
Between Thought and Trigger” targeting younger 18–34 Veterans. The Don’t wait. Reach out. campaign’s website, VA.gov/reach, also was created
with a diversity of topics and representative of diverse population, including application to younger Veterans (e.g., Career, financial, relationships).
216
VA’s efforts through Governor’s Challenge includes efforts to guide states to inviting tribal leaders to join planning teams as members,
incorporating culturally competent panels that allow for tribal representatives to share directly with our audiences at conferences and events
and reminding ourselves that we have access to subject matter experts from the AI/AN communities that we can seek support and guidance
from. Leveraging the interdepartmental relationship with SAMHSA, VA utilized tools such as the National Tribal Behavioral Health Agenda, a tool
designed to improve the way agencies address and improve behavioral health for American Indian and Alaska Native populations.
217
This special supplement published new research addressing suicide risk, resilience, surveillance, and prevention among adult women, with a
special emphasis on women Veterans and active-duty Service women.

85
6. Firearm Lethal Means Safety (LMS) Efforts: In 2021, VA significantly expanded its focus in LMS focused on secure
firearm storage through LMS training, enhancement of gun lock distribution, expansion of partnership efforts
in LMS and launching of the first national-level suicide prevention campaign focused on secure firearm storage.
A critical piece of this effort was mandating lethal means safety training for all providers in VHA, which was later
extended to all new providers.
218,219
The SP Now program also launched LMS training for the newly created VCL Peer
Support Outreach Center (PSOC) employees and 100% of VCL responders. VA also continued an extensive focus on
gun lock distribution, distributing 276,900 gun locks in 2021, and launching a pilot within VCL on distributing gun
locks via mail for those Veterans who desired one after calling VCL. As 1 of the 3 major goals of CBI-SP is focused
on lethal means safety, Governor’s Challenge state teams received training in lethal means safety and assist in
distributing gun locks and promoting discussions about secure firearm storage within their local communities.
VA also continued partnerships with organizations like NSSF and American Foundation for Suicide Prevention, to
create and disseminate messages on secure storage with shared branding (e.g., A Toolkit for Safe Firearm Storage in
Your Community), which laid a foundation for broader work in coming years. Along with NSSF, VA began designing
a series of short videos focused on secure firearm storage. In 2021, VA also launched the Keep It Secure campaign
(focused specifically on Lethal Means Safety and firearms) promoting awareness of Veteran-specific drivers of risk
and the steps Veterans and their support networks can take to increase safety through secure storage of firearms. In
FY 2021, these efforts resulted in 1.2 billion engagements (impressions), 726 million completed video views and 3.8
million website visits.
218
VHA Assistant Under Secretary for Health for Operations, Lethal Means Safety (LMS) Education and Counseling memo, November 2, 2020.
219
Assistant under Secretary for Health for Clinical Services/Chief Medical Officer (CMO), Lethal Means Safety (LMS) Education and Counseling memo,
March 17, 2022.

86
Appendix B: Suicide Prevention Demonstration
(Pilot) Projects, FY 2024
Suicide Prevention demonstration (pilot) projects for FY 2024 are listed below:
• Asian American Pacific Islander (AAPI) Project: Multi-method project designed to further clarify the unique
needs and drivers of suicide risk among AAPI Veterans and gain new knowledge essential to understanding suicide
risk and prevention among AAPI Veterans.
• Acceptance and Commitment Training for Health Care Providers (ACT-HCP): Online, self-guided application
based on health care providers needs and will test the acceptability and feasibility of the intervention among VA
medical and mental health providers.
• Artificial Intelligence (AI) Firearms SUD Project: This project is developing AI methods to identify firearm and
substance use risk factors and provides VHA automated methods to efficiently measure which Veterans have
access to firearms, and which Veterans, among those with substance use disorders (SUD), are in a state of ongoing
substance misuse, versus in early rehabilitation or long-term maintenance.
• American Indian/Alaska Native (AI/AN) Suicide Prevention Project: This project is using existing VA data to
increase understanding of social determinants and Veterans health care use-related factors that may contribute to
the high suicide risk for AI/AN Veterans.
• The Brief Intervention and Contact (BIC) Pilot: This pilot is a brief, personalized intervention prior to discharge
from an acute inpatient hospitalization and continues with regular contact after discharge by a BIC coach to reduce
suicide risk and expand resources.
• Coaching Into Care (CIC) Suicide Prevention Project: This project is a post-hospitalization risk-reduction project
focused on lethal means safety (LMS) conversations with Veterans and their concerned supporters when a Veteran
has recently discharged from inpatient psychiatric hospitalization.
• Community Coalition Functioning Evaluation Project: This project will support VA’s Community-Based
Interventions for Suicide Prevention by assessing the strengths, weaknesses and opportunities that inform
community coalition successes in providing Veteran suicide prevention services.
• Co-Occurring Homelessness and Suicide Risk Clinical Processes Project: This project will focus on the
refinement of methods and procedures across VA to screen and identify homelessness in Veterans at risk for suicide.
• Establishing and Sustaining a National Suicide Prevention Program for LGBTQ+ Veterans Project: This
project will focus on the expansion and sustainability of “PRIDE in All Who Served,” a manualized, evidence-based
intervention to ensure at-risk LGBTQ+ Veterans have access to an effective, tailored health promotion program that
reduces suicide risk regardless of where they access care.
• Improving Safe Firearm Storage in Veterans through Involving a Concerned Significant Other Project: This
project will develop and test LMS interventions with concerned supporters, providing resources and education on
how to discuss lethal means safety with their Veteran loved ones.

87
• Leveraging Digital Platforms for Communicating Lethal Means Safety (LMS) Messages to Younger Veterans:
This is a project that seeks to address gaps in effective messaging and evidence-based recommendations to
younger Veterans via digital platforms by proposing to apply more rigorous methods to evaluate the use of LMS
messaging and the impact of digital platforms to inform subsequent campaign development and deployment.
• Leveraging Social Media to Reach LGBTQ+ Veterans at Risk of Suicide Project: This project is engaging Non-
Engaged Veterans and examines optimal methods for engagement of LGBTQ+ Veterans at risk of suicide, to identify
barriers to engaging in care and to understand the needs and key targets for interventions.
• Optimizing the Use and Dissemination of brief Cognitive Behavioral Therapy for Insomnia for the Purpose
of Suicide Prevention (bCBTI-SP) Project: This project translates the online training package for bCBTI-SP to
community providers to reach Veterans outside of VHA care with this evidence-based intervention.
• Partnering with Firearm Retailers to Promote and Provide Out-of-Home Firearm Storage Project:
This project will support the sustainability and scalability of The Armory Project (TAP), a community-engaged
approach to develop and maintain networks to promote and provide temporary out-of-home firearm storage for
suicide prevention.
• Postvention Project: This project will implement enhancements to the United for Postvention resource hub,
including the development of an enterprise-wide infrastructure available to all VHA staff, consultation, and
resources for postvention care.
• Project Life Force (PLF) Project: This project delivers suicide prevention clinical intervention via clinical telehealth
hubs that includes providing safety planning, lethal means counseling and other emotional regulation and
interpersonal skills that is delivered by VA providers for Veterans at risk for suicide, including those in rural settings.
• Social Determinants and Mortality Study: Study of patterns and trends project incorporates all-cause mortality
and “deaths of despair” (overdose, substance use and suicide) to improve visibility of disproportionately affected
areas to inform and evaluate VA’s suicide prevention efforts.
• Suicide Risk Identification and Prevention in Reproductive Healthcare Settings (SP-RHC) Project: This project
is a mixed-methods study that seeks to address the critical knowledge gap and generate findings and products that
can be leveraged to tailor suicide prevention practices for, and facilitate implementation in, reproductive health
care (RHC) settings serving women Veterans.
• Suicide Prevention through Whole Health for VA Police and VA Police Peer Support National Initiatives:
This project focuses on VA Police Veteran suicide prevention through Whole Health wellness/empowerment and
Peer Support for VA Police.
• Suicide Prevention Among Older Veterans Project: This project addressing Firearm Safety will support the
completion and distribution of a 20-minute video training for clinicians across VHA on how to conduct firearm
safety discussions with older Veterans and family members.
• Surveillance and Reporting of Suicidal Ideation Assessment in Post Traumatic Stress Disorder (PTSD)
Specialty Care Clinical Notes Project: This project will use Natural Language Processing to surveil and monitor
the conduct and quality of suicide ideation assessment during treatment in PTSD specialty care.
• VHA Service Use Proximal to Firearm Suicide Among U.S. Veterans: This project will describe the frequency
and settings of VHA health care service use prior to Veterans’ deaths by firearm suicide among all Veterans who
used VHA services and develop dissemination tools to clinical care settings to inform VHA setting specific LMS
counseling initiatives.

88
• Veteran Sponsorship Initiative+ (VSI): This initiative provides expansion to support High-Risk Transitioning Service
members (TSM) and Veterans and will use a precision medicine approach to identify TSMs at high risk for suicide, for
targeted enhanced care and management, to reduce suicide risks during this vulnerable transition period.
• Integrated Mental Health Providers Project: This project will provide prevention, early intervention, education,
and access for at-risk Veterans in non-mental health clinic settings, to include neurology, sleep and oncology clinics.
• Center of Excellence Hub for the Study of Younger Veterans Pilot: This will pilot outreach (18- to 34-year-old
outreach and engagement), care coordination and continuity projects focused on 18- to 34-year-old at-risk Veterans.
• The National Center for Veteran Financial Well-being (NCVFW): The NCVFW ensures Veterans have ready-
access to education, tools and resources necessary for the successful navigation of barriers to financial wellness and,
thereby, reduce risk of suicide in those circumstances where financial stressors are the primary driver of risk.
• VA Risk ID Universal Suicide Screening: This is an evidence-informed population-based approach designed to
detect and manage suicide risk among Veterans presenting to a wide range of health care settings.
• Safety Planning in the Emergency Department (SPED): SPED is an evidence-based intervention required in
VA after research demonstrated that safety planning and structured outreach was associated with a reduction in
suicidal behavior in the 6 months following an emergency department visit.
• Suicide Risk Management (SRM) Consultation Program: This program supports all providers (VA or the
community) by disseminating evidence-informed suicide prevention strategies, training and resources offering case
consultation at no cost.
• United for Postvention Program: This program establishes guidelines and resources specific to suicide
postvention, to achieve VHA’s goal to address the care of bereaved survivors, caregivers, and health care providers.
Department of Veterans Affairs
November 2023
