
Medicare Claims Processing Manual
Chapter 20 - Durable Medical Equipment, Prosthetics,
Orthotics, and Supplies (DMEPOS)
Table of Contents
(Rev. 12557; Issued: 03-28-24)
Transmittals for Chapter 20
01 - Foreword
10 - Where to Bill DMEPOS and PEN Items and Services
10.1 - Definitions
10.1.1 - Durable Medical Equipment (DME)
10.1.2 - Prosthetic Devices - Coverage Definition
10.1.3 - Prosthetics and Orthotics (Leg, Arm, Back, and Neck Braces,
Trusses, and Artificial Legs, Arms, and Eyes) - Coverage
Definition
10.1.4 - Payment Definition Variances
10.1.4.1 - Prosthetic Devices
10.1.4.2 - Prosthetic and Orthotic Devices (P&O)
10.2 - Coverage Table for DME Claims
10.3 - Beneficiaries Previously Enrolled in Managed Care Who Return to
Traditional Fee for Service (FFS)
20 - Calculation and Update of Payment Rates
20.1 - Update Frequency
20.2 - Locality
20.3 - Elimination of "Kit" Codes and Pricing of Replacement Codes
20.4 - Contents of Fee Schedule File
20.5 - Online Pricing Files for DMEPOS
20.6 - Phase-in For Competitive Bid Rates in Areas Not in a Competitive Bid
Area
30 - General Payment Rules
30.1 - Inexpensive or Other Routinely Purchased DME
30.1.1 - Used Equipment
30.1.1.2 – Used Rental Equipment
30.1.2 - Transcutaneous Electrical Nerve Stimulator (TENS)
30.2 - Items Requiring Frequent and Substantial Servicing
30.2.1 - Daily Payment for Continuous Passive Motion (CPM) Devices
30.3 - Certain Customized Items
30.4 - Other Prosthetic and Orthotic Devices
30.5 - Capped Rental Items
30.5.1- Capped Rental Fee Variation by Month of Rental
30.5.2 - Purchase Option for Capped Rental Items
30.5.3 - Additional Purchase Option for Electric Wheelchairs
30.5.3.1 - Exhibits
30.5.4 - Payments for Capped Rental Items During a Period of Continuous
Use
30.5.5 - Payment for Power-Operated Vehicles that May Be Appropriately
Used as Wheelchair
30.6 - Oxygen and Oxygen Equipment
30.6.1 - Adjustments to Monthly Oxygen Fee
30.6.2 - Purchased Oxygen Equipment
30.6.3 - Contents Only Fee
30.6.4 - DMEPOS Clinical Trials and Demonstrations
30.7 - Payment for Parenteral and Enteral Nutrition (PEN) Items and Services
30.7.1 - Payment for Parenteral and Enteral Pumps
30.7.2 - Payment for PEN Supply Kits
30.8 - Payment for Home Dialysis Supplies and Equipment
30.8.1 - DME MAC and A/B MAC (A) Determination of ESRD
MethodSelection
30.8.2 - Installation and Delivery Charges for ESRD Equipment
30.8.3 - Elimination of Method II Home Dialysis
30.9 - Payment of DMEPOS Items Based on Modifiers
30.9.1 – Processing of Expatriate Beneficiary DMEPOS Claims for
Purchased Items Submitted with the EX Modifier
40 - Payment for Maintenance and Service of Equipment
40.1 - General
40.2 - Maintenance and Service of Capped Rental Items
40.3 - Maintenance and Service of PEN Pumps
50 - Payment for Replacement of Equipment
50.1 - Payment for Replacement of Capped Rental Items
50.2 - A/B MAC (A) or (HHH) Format for Durable Medical Equipment,
Prosthetic, Orthotic and Supply Fee Schedule
50.3 - Payment for Replacement of Parenteral and Enteral Pumps
50.4 - Payment for Replacement of Oxygen Equipment in Bankruptcy Situations
50.5 – Payment of a Part of a DMEPOS Item
60 - Payment for Delivery and Service Charges for Durable Medical Equipment
80 - Penalty Charges for Late Payment Not Included in Reasonable Charges or Fee
Schedule Amounts
90 - Payment for Additional Expenses for Deluxe Features
100 - General Documentation Requirements
100.1 - Written Order Prior to Delivery
100.1.1 - Written Order Prior to Delivery - HHAs
100.2 - Certificates of Medical Necessity (CMN)
100.2.1 - Completion of Certificate of Medical Necessity Forms
100.2.2 - Evidence of Medical Necessity for Parenteral and Enteral
Nutrition (PEN) Therapy
100.2.2.1 - Scheduling and Documenting Certifications and
Recertifications of Medical Necessity for PEN
100.2.2.2 - Completion of the Elements of PEN CMN
100.2.2.3 - DME MAC Review of Initial PEN Certifications
100.2.3.1 - Scheduling and Documenting Recertifications of
Medical Necessity for Oxygen
100.2.3.2 - HHA Recertification for Home Oxygen Therapy
100.2.3.3 - A/B MAC (A) or (HHH) Review of Oxygen
Certifications
100.3 - Limitations on DME MAC Collection of Information
100.4 - Reporting the Ordering/Referring NPI on Claims for DMEPOS Items
Dispensed Without a Physician's Order
110 - General Billing Requirements - for DME, Prosthetics, Orthotic Devices, and
Supplies
110.1 - Billing/Claim Formats
110.1.1 - Requirements for Implementing the NCPDP Standard
110.1.2 - Certificate of Medical Necessity (CMN)
110.1.3 - NCPDP Companion Document
110.2 - Application of DMEPOS Fee Schedule
110.3 - Pre-Discharge Delivery of DMEPOS for Fitting and Training
110.3.1 - Conditions That Must Be Met
110.3.2 - Date of Service for Pre-Discharge Delivery of DMEPOS
110.3.3 - Facility Responsibilities During the Transition Period
110.4 - Frequency of Claims for Repetitive Services (All Providers and
Suppliers)
110.5 - DME MACs Only - Appeals of Duplicate Claims
120 - DME MACs - Billing Procedures Related To Advanced Beneficiary Notice (ABN)
Upgrades
120.1 - Providing Upgrades of DMEPOS Without Any Extra Charge
130 - Billing for Durable Medical Equipment (DME) and Orthotic/Prosthetic Devices
130.1 - Provider Billing for Prosthetic and Orthotic Devices
130.2 - Billing for Inexpensive or Other Routinely Purchased DME
130.3 - Billing for Items Requiring Frequent and Substantial Servicing
130.4 - Billing for Certain Customized Items
130.5 - Billing for Capped Rental Items (Other Items of DME)
130.6 - Billing for Oxygen and Oxygen Equipment
130.6.1 - Oxygen Equipment and Contents Billing Chart
130.7 - Billing for Maintenance and Servicing (Providers and Suppliers)
130.8 - Installment Payments
130.9 - Showing Whether Rented or Purchased
140 - Billing for Supplies
140.1 - Billing for Supplies and Drugs Related to the Effective Use of DME
140.1.1 - Billing of Insulin Furnished through DME
140.2 - Billing for HHA Medical Supplies
140.3 - Billing DME MAC for Home Dialysis Supplies and Equipment
150 - Institutional Provider Reporting of Service Units for DME and Supplies
160 - Billing for Total Parenteral Nutrition and Enteral Nutrition
160.1 - Billing for Total Parenteral Nutrition and Enteral Nutrition Furnished to
Part B Inpatients
160.2 - Special Considerations for SNF Billing for TPN and EN Under Part B
170 - Billing for Splints and Casts
180 - Billing for Home Infusion Therapy Services
181 – Lymphedema Compression Treatment Benefit
181.1 - Payment Policy for Lymphedema Compression Treatment Items
190 - A/B MAC (A), (B), (HHH), or DME MAC Application of Fee Schedule and
Determination of Payments and Patient Liability for DME Claims
200 - Automatic Mailing/Delivery of DMEPOS
210 - CWF Crossover Editing for DMEPOS Claims During an Inpatient Stay
211 -SNF Consolidated Billing and DME Provided by DMEPOS Suppliers
211.1 - General Information
211.2 - Partial Month Stays For Capped Rental Equipment
212 - Home Health Consolidated Billing and Supplies Provided by DMEPOS Suppliers
213- Billing for Home IVIG Items and Services
220 - Appeals
230 - DME MAC Systems
300 - New Systems Requirements

01 - Foreword
(Rev. 12423; Issued: 12-20-23; Effective: 01-01-24; Implementation: 01-02-24)
This chapter provides general instructions on billing and claims processing for durable
medical equipment (DME), prosthetics and orthotics (P&O), parenteral and enteral
nutrition (PEN), and supplies. Coverage requirements are in the Medicare Benefit Policy
Manual and the National Coverage Determinations Manual.
These instructions are applicable to services billed to the A/B MAC (A), (B), and (HHH),
and DME MAC unless otherwise noted.
The DME, prosthetic/orthotic devices (except customized devices in a SNF), supplies and
oxygen used during a Part A covered stay for hospital and skilled nursing facility (SNF)
inpatients are included in the inpatient prospective payment system (PPS) and are not
separately billable.
In this chapter the terms provider and supplier are used as defined in 42 CFR 400.42 CFR
400.202 (Follow the link, choose the applicable year, select Title 42, then open Chapter
IV. You then must choose which part to open. To get to §400.202 you select the first
choice and download the pdf version.).
• Provider means a hospital, a CAH, a skilled nursing facility, a
comprehensive outpatient rehabilitation facility, a home health agency, or a
hospice that has in effect an agreement to participate in Medicare, or a clinic, a
rehabilitation agency, or a public health agency that has in effect a similar
agreement but only to furnish outpatient physical therapy or speech-language
pathology services, or a community mental health center that has in effect a
similar agreement but only to furnish partial hospitalization or intensive outpatient
services.
Of these provider types only hospitals, CAHs, SNFs, and HHAs would be able to bill for
DMEPOS; and for hospitals, CAHs, and SNFs usually only for outpatients. Any
exceptions to this rule are discussed in this chapter.
• Supplier means a physician or other practitioner, or an entity other than a
provider that furnishes health care services under Medicare.
A DMEPOS supplier must meet certain requirements and enroll as described in Chapter
10 of the Program Integrity Manual. A provider that enrolls as a supplier is considered a
supplier for DMEPOS billing. However, separate payment remains restricted to those
items that are not considered included in a PPS rate.

Unless specified otherwise the instructions in this chapter apply to both providers and
suppliers, and to the A/B MACs (A), (B), (HHH), and DME MACs that process their
claims.
10 - Where to Bill DMEPOS and PEN Items and Services
(Rev. 11414; Issued: 05-12-22; Effective: 06-13-22; Implementation: 06-13-22)
NOTE: CMS seeks to reduce burden and modernize processes to ensure a reduction in
improper payments and an increase in customer satisfaction. The Certificate of Medical
Necessity (CMN) form and DME Information Form (DIF) were originally required to
help document the medical necessity and other coverage criteria for selected Durable
Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items. In the past, a
supplier received a signed CMN from the treating physician or created and signed a DIF
to submit with the claim. Due to improvements in claims processing and medical records
management, the information found on CMNs or DIFs is available either on the claim or
in the medical record and is redundant. Therefore, to reduce burden and increase
customer satisfaction, providers and suppliers no longer need to submit these forms for
services rendered after January 1, 2023.
• For claims with dates of service on or after January 1, 2023 – providers and
suppliers no longer need to submit CMNs or DIFs with claims. Due to electronic
filing requirements, claims received with these forms attached will be rejected and
returned to the provider or supplier.
• For claims with dates of service prior to January 1, 2023 – processes will not
change and if the CMN or DIF is required, it will still need to be submitted with
the claim, or be on file with a previous claim.
This statement applies throughout the Program Integrity Manual wherever CMNs and
DIFs are mentioned.
Skilled Nursing Facilities, CORFs, OPTs, and hospitals bill the A/B MAC Part A for
prosthetic/orthotic devices, supplies, and covered outpatient DME and oxygen (refer to
§40). The HHAs should bill Durable Medical Equipment (DME) to the A/B MAC
(HHH), or should meet the requirements of a DME supplier and bill the DME MAC.
This is the HHA's decision. A/B MACs Part A other than A/B MACs (HHH) will
receive claims only for the class "Prosthetic and Orthotic Devices."
Unless billing to the A/B MAC Part A is required as outlined in the preceding paragraph,
claims for implanted DME, implanted prosthetic devices, replacement parts, accessories
and supplies for the implanted DME shall be billed to the A/B MACs Part B and not the
DME MAC.
Suppliers enrolled with the NSC as a DMEPOS supplier should enroll with and bill to the
A/B MAC Part B for replacement parts, accessories and supplies for prosthetic implants
and surgically implanted DME items that are not required to be billed to the A/B MAC
Part A as stated above. Such suppliers should bill the A/B MAC Part B for these items

only, unless the entity separately qualified as a supplier for items and/or services in
another benefit category.
Suppliers that enroll with the NSC as a DMEPOS supplier shall bill the A/B MAC Part B
using their NPI and shall not include their NSC number on the claim.
Under no circumstances should any entity that is enrolled as a DMEPOS supplier with
the NSC, that is not the physician or provider that implants the device, bill the A/B MAC
Part B for an implanted device. However, DMEPOS suppliers should bill for any of the
replacement parts, accessories or supplies for prosthetic implants and surgically
implanted DME.
The claims filing jurisdiction for these items is determined by the supplier’s location, in
accordance with Pub. 100-04, Medicare Claims Processing Manual, chapter 1, section 10.
With respect to payment for these items, contractors are reminded of the longstanding
policy for payment of DMEPOS items, which specifies that payment for DMEPOS is
based on the fee schedule amount for the State where the beneficiary maintains his/her
permanent residence.
The Healthcare Common Procedure Coding System (HCPCS) codes that describe these
categories of service are updated quarterly. All other DMEPOS items are billed to the
DME MAC. See the Medicare Claims Processing Manual, Chapter 23, §20.3 for
additional information. A spreadsheet containing an updated list of HCPCS for which
DME MACs have jurisdiction is updated as needed (typically quarterly) to reflect codes
that have been added or discontinued (deleted). Any new HCPCS not included in this
updated list are A/B MAC jurisdiction only, and not DME MAC jurisdiction. The
spreadsheet is posted at the following website: https://www.cms.gov/Center/Provider-
Type/Durable-Medical-Equipment-DME-Center.html under the heading of Coding.
Parenteral and enteral nutrition, and related accessories and supplies, are covered under
the Medicare program as a prosthetic device. See the Medicare Benefit Policy Manual,
Chapter 15, for a description of the policy. All Parenteral and Enteral (PEN) services
furnished under Part B are billed to the DME MAC. If a provider (see §01) provides
PEN items under Part B it shall qualify for and receive a supplier number and bill as a
supplier. Note that some PEN items furnished to hospital and SNF inpatients are
included in the Part A PPS rate and are not separately billable. (If a service is paid under
Part A it should not also be paid under Part B.)
10.1 - Definitions
(Rev. 1, 10-01-03)
A3-3313.1, B3-2100.1, HHA-220.1, HO-235.1, SNF-264.1
10.1.1 - Durable Medical Equipment (DME)
(Rev. 1, 10-01-03)
DME is covered under Part B as a medical or other health service (§1861(s)(6) of the
Social Security Act [the Act]) and is equipment that:
a. Can withstand repeated use;
b. Is primarily and customarily used to serve a medical purpose;
c. Generally is not useful to a person in the absence of an illness or injury; and
d. Is appropriate for use in the home.
All requirements of the definition must be met before an item can be considered to be
durable medical equipment.
A SNF normally is not considered a beneficiary's home. However, a SNF can be
considered a beneficiary's home for Method II home dialysis purposes. See the Program
Integrity Manual, Chapter 5, for guidelines on when a SNF may be considered a home.
For detailed coverage requirements (including definitions and discussion) associated with
the following DME terms and circumstances see the Medicare Benefit Policy Manual,
Chapter 15:
• "Durability"
• "Medical Equipment"
• "Equipment Presumptively Medical"
• "Equipment Presumptively Nonmedical"
• "Special Exception Items"
• "Necessary and Reasonable"
• "Necessity for the Equipment"
• "Reasonableness of the Equipment"
• "Payment Consistent With What is Necessary and Reasonable"
• "Beneficiary's Home"
• "Establishing the Period of Medical Necessity"

• "Repairs, Maintenance, Replacement and Delivery"
• "Leased Renal Dialysis Equipment"
• "Coverage of Supplies and Accessories"
• "Beneficiary Disposal of Equipment"
• "New Supplier Effective Billing Date"
• "Incurred Expense Date"
• "Partial Months-Monthly Payment"
• "Purchased Equipment Delivered Outside the U.S."
For coverage information on specific situations and items of DME, see the Medicare
National Coverage Determinations Manual.
10.1.2 - Prosthetic Devices - Coverage Definition
(Rev. 1, 10-01-03)
Prosthetic devices (other than dental) are covered under Part B as a medical or other
health service (§1861(s)(8) of the Act) and are devices that replace all or part of an
internal body organ or replace all or part of the function of a permanently inoperative or
malfunctioning internal body organ. Replacements or repairs of such devices are covered
when furnished incident to physicians' services or on a physician's orders.
For detailed coverage requirements (including definitions and discussion) associated with
the following prosthetic device terms and circumstances see the Medicare Benefit Policy
Manual, Chapter 15:
• "Test of Permanence"
• "Prosthetic Lenses"
• "Intraocular Lenses (IOLs)"
• "Supplies, Adjustments, Repairs and Replacements"
For coverage information on specific situations and prosthetic devices, see the Medicare
National Coverage Determinations Manual.
10.1.3 - Prosthetics and Orthotics (Leg, Arm, Back, and Neck Braces,
Trusses, and Artificial Legs, Arms, and Eyes) - Coverage Definition
(Rev. 1, 10-01-03)
These appliances are covered under Part B as a medical or other health service
(§1861(s)(9) of the Act) when furnished incident to physicians' services or on a

physician's order. A brace includes rigid and semi-rigid devices that are used for the
purpose of supporting a weak or deformed body member or restricting or eliminating
motion in a diseased or injured part of the body.
For detailed coverage requirements (including definitions and discussion) associated with
the following terms and circumstances see the Medicare Benefit Policy Manual, Chapter
15:
"Leg, Arm, Back, and Neck Braces, Trusses, and Artificial Legs, Arms, and
Eyes"
"Adjustments and Replacement of Artificial Limbs"
For coverage information on specific situations, braces, trusses, and artificial limbs and
eyes, see the Medicare National Coverage Determinations Manual.
10.1.4 - Payment Definition Variances
(Rev. 1, 10-01-03)
10.1.4.1 - Prosthetic Devices
(Rev. 1, 10-01-03)
§§1834(h)(1)(G) and (H) of the Act, "Replacement of Prosthetic Devices and Parts,"
refers to prosthetic devices that are artificial limbs. (Follow the link, scroll down to
section (h) and look for the above title.) (Section 1861(s) of the Act, which defines
"medical and other health services," does not define artificial limbs as "prosthetic
devices" (§1861(s)(8) follow the link, scroll down to section (s) and look for “(8)
prosthetic devices”). Rather, artificial limbs are included in the §1861(s)(9) category,
"orthotics and prosthetics." When discussing replacement, these instructions will use the
term "prosthetic device" as intended by §1834(h)(1)(G), i.e., artificial limbs.
10.1.4.2 - Prosthetic and Orthotic Devices (P&O)
(Rev. 1, 10-01-03)
Except as specifically noted (e.g., IOLs), when discussing payment and other policies,
instructions in this chapter will use the terms "prosthetic and orthotic devices" and the
abbreviation "P&O" interchangeably to refer to both §1861(s)(8) and (9) (follow the link,
scroll down to section (s) and look for both (8) and (9)) services.
10.2 - Coverage Table for DME Claims
(Rev. 4001, Issued: 03-16-18, Effective: 06-19-18, Implementation: 06-19-18)
B3-2105

Reimbursement may be made for expenses incurred by a patient for the rental or purchase
of durable medical equipment (DME) for use in his/her home provided that all the
conditions in column A below have been met. Column B indicates the action A/B MACs
(A), (B), and (HHH), and DME MACs will take to establish that the conditions have been
met.
A - Conditions
B - Review Action
l. Payment may be made for the
following:
1. Payment may be made for following:
(a) Items of DME that are medically
necessary
(a) The HCPCS file shows coverage status
of items. If item is not listed in the HCPCS
file, the MAC will develop LMRP to
determine whether the item is covered.
(b) Separate charges for repair,
maintenance and delivery
(b) Repairs - only if DME is being
purchased or is already owned by patient
and repair is necessary to make the
equipment serviceable. Medicare pays the
least expensive alternative. (See special
exception in Chapter 15 of the Medicare
Benefit Policy Manual for repair of dialysis
delivery system.)
NOTE: See Chapter 15 of the Medicare
Benefit Policy Manual for handling claims
suggesting deliberate or malicious damage
or destruction.
Maintenance - only if the equipment is
being purchased, or is already owned by the
patient, and if the maintenance is extensive
amounting to repairs, i.e., requiring the
services of skilled technicians. (MACs
deny claims for routine maintenance and
periodic servicing, e.g., testing, cleaning,
checking, oiling, etc.) (See special
exception in Chapter 15 of the Medicare
Benefit Policy Manual for maintenance of
dialysis delivery system.)
Delivery - of rented or purchased equipment
is covered, but the related payment is
included in the fee schedule for the item.
Additional payment may be made at the
discretion of the MAC in special
circumstances (see Chapter 15 of the
Medicare Benefit Policy Manual)
(c) Separate charges for disposable
supplies, e.g., oxygen, if essential to the
effective use of medically necessary
(c) Claim must indicate that:
• The patient has the DME for which the
supply is intended;

A - Conditions
B - Review Action
durable medical equipment. Separate
charges for replacement of essential
accessories such as hoses, tubes,
mouthpieces, etc., only if the beneficiary
owns or is purchasing durable medical
equipment (BPM, Chapter 15, §110).
(Medications used in connection with
durable medical equipment are covered
under certain conditions - see Chapter
15 of the Medicare Benefit Policy
Manual)
•
The DME continues to be medically
necessary; and
• The items are readily identifiable as the
type customarily used with such
equipment.
NOTE: If the quantity of accessories and/or
supplies included in a claim seems
excessive or if claims for such items are
received from the same claimant with undue
frequency, see Chapter 5 of the Medicare
Program Integrity Manual.
2. DME must be for use in patient's
residence other than a health care
institution. (BPM, Chapter 15, §110.1.D
& PIM, Chapter 5, §1)
2. Payment cannot be made for equipment
for use in an institution classified as:
a. A participating hospital,
b. An emergency hospital,
c. Meets §1861(e)(1) of the Act,
d. A participating SNF or
e. Meets §1819(a)(1) of the Act.
If an institution that includes a Medicare-
participating distinct part SNF also has a
nonparticipating portion that does not meet
1819(a)(1), the patient may be considered in
his/her residence if he/she was physically
located in such nonparticipating portion
during the use period.
DMEPOS (DME, P&O, and supplies) items
provided to hospice patients are generally
included in the payment for hospice
services. Items of DMEPOS are covered by
Medicare and paid in addition to the hospice
payment only when those items or supplies
are provided to the patient for treatment of a
condition or illness not related to the
patient's terminal illness.
3. Physician's prescription required.
A supplier must maintain and, upon request,
make available to the MAC, the detailed
written order (or, when required, the
Certificate of Medical Necessity (CMN))
from the treating physician. See the
Medicare Program Integrity Manual,
Chapter 5.
10.3 - Beneficiaries Previously Enrolled in Managed Care Who Return
to Traditional Fee for Service (FFS)
(Rev. 1, 10-01-03)
B3-9051
When a beneficiary who was previously enrolled in a Medicare HMO/Managed Care
program returns to traditional FFS, he or she is subject to all benefits, rules, requirements
and coverage criteria as a beneficiary who has always been enrolled in FFS. When a
beneficiary returns to FFS, it is as though he or she has become eligible for Medicare for
the first time. Therefore, if a beneficiary received any items or services from their HMO
or Managed Care plan, they may continue to receive such items and services only if they
would be entitled to them under Medicare FFS coverage criteria and documentation
requirements.
For example, if a beneficiary received a manual wheelchair under a HMO/Managed Care
plan, he or she would need to meet Medicare coverage criteria and documentation
requirements for manual wheelchairs. He or she would have to obtain a Certificate of
Medical Necessity (CMN), and would begin an entirely new rental period, just as a
beneficiary enrolled in FFS, to obtain a manual wheelchair for the first time.
There is an exception to this rule if a beneficiary was previously enrolled in FFS and
received a capped rental item, then enrolled in an HMO, stayed with the HMO for 60 or
fewer days, then returned to FFS. For purposes of this instruction, CMS has interpreted
an end to medical necessity to include enrollment in an HMO for 60 or more days.
Another partial exception to this rule involves home oxygen claims. If a beneficiary has
been receiving oxygen while under a Medicare HMO, the supplier must obtain an initial
CMN and submit it to the DME MAC at the time that FFS coverage begins. However,
the beneficiary does not have to obtain the blood gas study on the CMN within 30 days
prior to the Initial Certification date on the CMN, but the test must be the most recent
study the patient obtained while in the HMO, under the guidelines specified in DME
MAC policy. It is important to note that, just because a beneficiary qualified for oxygen
under a Medicare HMO, it does not necessarily follow that he/she will qualify for oxygen
under FFS.
Another partial exception to this rule involves home oxygen claims. If a beneficiary has
been receiving oxygen while under a Medicare HMO, the supplier must obtain an initial
CMN and submit it to the DME MAC at the time that FFS coverage begins. However,
the beneficiary does not have to obtain the blood gas study on the CMN within 30 days
prior to the Initial Certification date on the CMN, but the test must be the most recent
study the patient obtained while in the HMO, under the guidelines specified in DME
MAC policy. It is important to note that, just because a beneficiary qualified for oxygen
under a Medicare HMO, it does not necessarily follow that he/she will qualify for oxygen
under FFS.
These instructions apply whether a beneficiary voluntarily returns to FFS, or if he or she
involuntarily returns to FFS because their HMO or Managed Care plan no longer
participates in the Medicare + Choice (HMO) program.
20 - Calculation and Update of Payment Rates
(Rev. 1, 10-01-03)
B3-5017, PM B-01-54, 2002 PEN Fee Schedule
Section1834 of the Act requires the use of fee schedules under Medicare Part B for
reimbursement of durable medical equipment (DME) and for prosthetic and orthotic
devices, beginning January 1 1989. Payment is limited to the lower of the actual charge
for the equipment or the fee established.
Beginning with fee schedule year 1991, CMS calculates the updates for the fee schedules
and national limitation amounts and provides the A/B MACs (A), (B), (HHH), and DME
MACs with the revised payment amounts. The CMS calculates most fee schedule
amounts and provides them to the A/B MACs (A), (B), and (HHH), and DME MACs.
However, for some services CMS asks A/B MACs (B) to calculate local fee amounts and
to provide them to CMS to include in calculation of national amounts. These vary from
update to update, and CMS issues special related instructions to A/B MACs (B) when
appropriate.
Parenteral and enteral nutrition services paid on and after January 1, 2002 are paid on a
fee schedule. This fee schedule also is furnished by CMS. Prior to 2002, payment
amounts for PEN were determined under reasonable charge rules, including the
application of the lowest charge level (LCL) restrictions.
The CMS furnishes fee schedule updates (DMEPOS, PEN, etc.) at least 30 days prior to
the scheduled implementation. A/B MACs (A), and (HHH) use the fee schedules to pay
for covered items, within their claims processing jurisdictions, supplied by hospitals,
home health agencies, and other providers. A/B MACs (A) and (HHH) consult with
DME MACs and, where appropriate with A/B MACs (B), on filling gaps in fee
schedules.
The CMS furnishes the fee amounts annually, or as updated if special updates should
occur during the year, to A/B MACs (A), (B), (HHH), and DME MACs and the Railroad
Retirement Board (RRB), Specialty MAC (SMAC), and to other interested parties
(including the Pricing, Data Analysis and Coding Contractor (PDAC), RRB, Indian
Health Service, and United Mine Workers).
20.1 - Update Frequency
(Rev. 1, 10-01-03)
AB-03-071, AB-03-100, CMS Web Site
The DMEPOS fee schedule is updated annually to apply update factors and quarterly to
include new codes and correct errors.

The current update of the DMEPOS fee schedule is located at:
http://www.cms.gov/Medicare/Medicare-Fee-for-Service-
Payment/DMEPOSFeeSched/DMEPOS-Fee-Schedule.html
The current quarterly update is also located at: http://www.cms.gov/Medicare/Medicare-
Fee-for-Service-Payment/DMEPOSFeeSched/DMEPOS-Fee-Schedule.html
20.2 - Locality
(Rev. 1, 10-01-03)
B3-5017.1
For services furnished on or after January 1, 1987, the U.S. is considered one locality.
The U.S. constitutes a "medical service area comparable to the concept of trade areas,"
for the furnishing of enteral and parenteral therapies. The therapies, nutrients and
associated supplies are available only from nationally recognized manufacturers and a
review of their published price lists displayed no variation based upon individual State or
other localities.
20.3 - Elimination of "Kit" Codes and Pricing of Replacement Codes
(Rev. 1, 10-01-03)
PM B-01-56
Prior to 2002, most suppliers billed for dialysis supplies using codes describing "kits" of
supplies. The use of kit codes allowed suppliers to bill for supply items without
separately identifying the supplies that are being furnished to the patient. Effective
January 1, 2002, these kit codes were deleted and suppliers are required to bill for
dialysis supplies using HCPCS codes for individual dialysis supplies.
20.4 - Contents of Fee Schedule File
(Rev. 1, 10-01-03)
PM A-02-090
The fee schedule file provided by CMS contains HCPCS codes and related prices subject
to the DMEPOS fee schedules, including application of any update factors and any
changes to the national limited payment amounts. The file does not contain fees for
drugs that are necessary for the effective use of DME. It also does not include fees for
items for which fee schedule amounts are not established. See Chapter 23 for a
description of pricing for these. The CMS releases via program issuance, the gap-filled
amounts and the annual update factors for the various DMEPOS payment classes:
Symbol
Payment Class
Category Label
IN
Inexpensive/routinely purchased.
DME
FS
Frequency Service.
DME
CR
Capped Rental.
DME
OX
Oxygen and Oxygen Equipment.
OXY

Symbol
Payment Class
Category Label
OS
Ostomy, Tracheostomy and
Urologicals
P/O
S/D
Surgical Dressings.
S/D
P/O
Prosthetics and Orthotics.
P/O
SU
Supplies.
DME
TE TENS. DME
The A/B MACs (HHH) need to retrieve data from all of the above categories. A/B
MACs (A) need to retrieve data only from categories P/O, S/D and SU. A/B MACs (A)
need to retrieve the SU category in order to be able to price supplies on Part B SNF
claims.
20.5 - Online Pricing Files for DMEPOS
(Rev. 2464, Issued: 05-04-12, Effective: 10-01-11-MCS/10-01-12-VMS,
Implementation: 10-03-11-MCS, VMS Analysis and Design /10-01-12-VMS
implementation)
The CMS provides updates to the DMEPOS fee schedule and related schedules annually or as
otherwise necessary. A/B MACs (B) or DME MACs must maintain at least five full
calendar years of fee schedules and related pricing data (i.e., the current and four prior
calendar years), regardless of the number of updates or pricing periods within those five
years.
20.6 - Phase-in For Competitive Bid Rates in Areas Not in a
Competitive Bid Area
(Rev. 3801, Issued: 06-28-17, Effective: 07-01-16, Implementation: 07-03-17 - For
contractors to retrieve and test the fee schedule and begin the adjustment process;
10-02-17 - For contractors to complete the adjustment process)
Section 1834(a)(1)(F)(ii) of the Act mandates adjustments to the fee schedule amounts
for certain DME items furnished on or after January 1, 2016, in areas that are not
competitive bid areas, based on information from competitive bidding programs for
DME. Regulations at section 414.210(g)(9) phased in these adjusted fees so that from
January 1, 2016 through June 30, 2016, the fee schedule amount in non-bid areas was
based on 50 percent of the adjusted payment amount established using competitive
bidding information and 50 percent of the unadjusted fee schedule amount (i.e., the 2015
fee schedule amount updated by the 2016 covered item update). Beginning July 1, 2016,
the fee schedule amounts for non-bid areas reverted to 100 percent of the adjusted
payment amounts determined using competitive bidding information.
Section 16007 of the 21st Century Cures Act changes the 2016 fee schedule transition
period so that payment based on 50 percent of the adjusted payment amount established
using competitive bidding information and 50 percent of the unadjusted fee schedule
amount extends from June 30, 2016 to December 31, 2016. Section 16007 also changes

from July 1, 2016 to January 1, 2017 the date that payment based on 100 percent of the
adjusted payment amounts in non-bid areas is effective.
Repriced Cures Act claim adjustments for the above mentioned dates of service shall use
the following RARC code: N689 - Alert: This reversal is due to a retroactive rate
change.
30 - General Payment Rules
(Rev. 11414; Issued: 05-12-22; Effective: 06-13-22; Implementation: 06-13-22)
NOTE: CMS seeks to reduce burden and modernize processes to ensure a reduction in
improper payments and an increase in customer satisfaction. The Certificate of Medical
Necessity (CMN) form and DME Information Form (DIF) were originally required to
help document the medical necessity and other coverage criteria for selected Durable
Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items. In the past, a
supplier received a signed CMN from the treating physician or created and signed a DIF
to submit with the claim. Due to improvements in claims processing and medical records
management, the information found on CMNs or DIFs is available either on the claim or
in the medical record and is redundant. Therefore, to reduce burden and increase
customer satisfaction, providers and suppliers no longer need to submit these forms for
services rendered after January 1, 2023.
• For claims with dates of service on or after January 1, 2023 – providers and
suppliers no longer need to submit CMNs or DIFs with claims. Due to electronic
filing requirements, claims received with these forms attached will be rejected and
returned to the provider or supplier.
• For claims with dates of service prior to January 1, 2023 – processes will not
change and if the CMN or DIF is required, it will still need to be submitted with
the claim, or be on file with a previous claim.
This statement applies throughout the Program Integrity Manual wherever CMNs and
DIFs are mentioned.
B3-5102
DMEPOS are categorized into one of the following payment classes:
• Inexpensive or other routinely purchased DME;
• Items requiring frequent and substantial servicing;
• Certain customized items;
• Other prosthetic and orthotic devices;
• Capped rental items; or
• Oxygen and oxygen equipment.
The CMS determines the category that applies to each HCPSC code and issues
instructions when changes are appropriate. See §§130 for billing information for each
payment class.
DME, including DME furnished under the home health benefit and Part B DME benefit,
is paid on the basis of the fee schedule.
Oxygen and oxygen equipment are paid on the basis of a fee schedule.
Any DME or oxygen furnished to inpatients under a Part A covered stay is included in
the SNF or hospital PPS rate. When an inpatient in a hospital or SNF is not entitled to
Part A inpatient benefits, payment may not be made under Part B for DME or oxygen
provided in the hospital or SNF because such facilities do not qualify as a patient's home.
The definition of DME in §1861(n) of the Act provides that DME is covered by Part B
only when intended for use in the home, which explicitly does not include a SNF or
hospital. (See the Medicare Benefit Policy Manual, Chapter 15). This does not preclude
separate billing for DME furnished after discharge.
Payment to providers and suppliers other than Home Health Agencies (HHAs) for
supplies that are necessary for the effective use of DME is made on the basis of a fee
schedule, except that payment for drugs is made under the drug payment methodology
rules (See Chapter 17 for drug payment information.)
Payment for prosthetics and orthotics is made on the basis of a fee schedule whether it is
billed to the A/B MAC (A), (B), or (HHH), or DME MAC.
Payment under Part B for surgical dressings is made on the basis of the fee schedule
except:
• Those applied incident to a physician's professional services;
• Those furnished by an HHA; and
• Those applied while a patient is being treated in an outpatient hospital
department.
30.1 - Inexpensive or Other Routinely Purchased DME
(Rev.4027; Issued: 04-27-18; Effective: 10-01-18; Implementation: 10-01-18)
For this type of equipment, A/B MACs (A), (B), or (HHH), and DME MACs pay
for rentals or lump-sum purchases. However, with the exception of TENS (see
§30.1.2), the total payment amount may not exceed the actual charge or the fee
schedule amount for purchase.
A. Inexpensive DME
This category is defined as equipment whose purchase price does not exceed
$150.
B. Other Routinely Purchased DME
This category is defined as equipment that is acquired at least 75 percent of the
time by purchase and includes equipment that is an accessory used in conjunction
with a nebulizer, aspirator, or ventilators that are either continuous airway
pressure devices or intermittent assist devices with continuous airway pressure
devices. Effective October 1, 2015, this category also includes speech generating
devices and accessories necessary for the effective use of speech generating
devices.
30.1.1 - Used Equipment
(Rev. 1, 10-01-03)
For payment purposes, used equipment is considered routinely purchased equipment and
is any equipment that has been purchased or rented by someone before the current
purchase transaction. Used equipment also includes equipment that has been used under
circumstances where there has been no commercial transaction (e.g., equipment used for
trial periods or as a demonstrator).
However, if a beneficiary rented a piece of brand new equipment and subsequently
purchased it, the payment amount for the purchase should be high enough so that the total
combined rental and purchase amounts at least equal the fee schedule for the purchase of
comparable new equipment. The payment amount may be established in this manner
only to the extent it does not exceed the actual charge made for the purchase.
EXAMPLES: The fee schedule amounts for an item of DME are ordinarily as follows:
$500 for purchase when the item is new.
$375 for purchase when the item is used.
$50 per month for renting the item.
Situation 1: A beneficiary rented the item when it was brand new for one month and then
purchased it for $500. The amount allowed for the purchase is $450 (i.e., $500 minus the
$50 allowed for the one month of rental) rather than $375.
Situation 2: A beneficiary rented the item for one month when it was brand new and then
purchased it for $400. The amount allowed for the purchase is $400 rather than the $450
that is allowable in situation 1 since the payment amount may not exceed the actual
charge for an item.
30.1.1.2 - Used Rental Equipment
(Rev. 3443, Issued: 01-29-16, Effective: 07-01-16, Implementation: 07-05-16)
When a beneficiary elects to purchase previously rented inexpensive and routinely
purchased DME and the service has a UE (purchase of used equipment) modifier the
Medicare allowed amount for used purchased equipment will be calculated at the lower
of the purchase fee schedule amount (UE) minus previous paid rental amounts or the
actual charge for the used purchased equipment.
30.1.2 - Transcutaneous Electrical Nerve Stimulator (TENS)
(Rev. 2605, Issued: 11-30-12, Effective: 06-08-12, Implementation: 01-07-13)
In order to permit an attending physician time to determine whether the purchase of a
TENS is medically appropriate for a particular patient, MACs pay 10 percent of the
purchase price of the item for each of 2 months. The purchase price and payment for
maintenance and servicing are determined under the same rules as any other frequently
purchased item, except that there is no reduction in the allowed amount for purchase due
to the two months rental.
Effective June 8, 2012, CMS will allow coverage for TENS use in the treatment of
chronic low back pain (CLBP) only under specific conditions which are described in the
NCD Manual, Pub. 100-03, chapter 1 Section 160.27.
30.2 - Items Requiring Frequent and Substantial Servicing
(Rev. 1, 10-01-03)
A3-3629
For this type of equipment, MACs pay the fee schedule amounts on a rental basis until
medical necessity ends. MACs cannot pay for purchase of this type of equipment.
30.2.1 - Daily Payment for Continuous Passive Motion (CPM) Devices
(Rev. 1, 10-01-03)
The CPM devices (HCPCS code E0935) are classified as items requiring frequent and
substantial servicing and are covered as DME as follows (see the Medicare National
Coverage Determinations Manual.):
• Continuous passive motion devices are covered for patients who have received a
total knee replacement. To qualify for coverage, use of the device must
commence within 2 days following surgery. In addition, coverage is limited to
that portion of the 3 week period following surgery during which the device is
used in the patient's home.
MACs make payment for each day that the device is used in the patient's home. No
payment can be made for the device when the device is not used in the patient's home or
once the 21 day period has elapsed. Since it is possible for a patient to receive CPM
services in their home on the date that they are discharged from the hospital, this date
counts as the first day of the three week limited coverage period.
30.3 - Certain Customized Items
(Rev. 2687, Issued: 04-19-13, Effective: 01-01-92, Implementation: 07-19-13)
Customized items are rarely necessary and are rarely furnished. In accordance with 42
CFR Section 414.224, in order to be considered a customized item, a covered item
(including a wheelchair) must be uniquely constructed or substantially modified for a
specific beneficiary according to the description and orders of a physician and be so
different from another item used for the same purpose that the two items cannot be
grouped together for pricing purposes. For example, a wheelchair that is custom
fabricated or substantially modified so that it can meet the needs of wheelchair-confined,
conjoined twins facing each other is unique and cannot be grouped with any other
wheelchair used for the same purpose. It is a one-of-a-kind item fabricated to meet
specific needs. Items that are measured, assembled, fitted, or adapted in consideration of
a patient’s body size, weight, disability, period of need, or intended use (i.e., custom
fitted items) or have been assembled by a supplier or ordered from a manufacturer who
makes available customized features, modification or components for wheelchairs that
are intended for an individual patient’s use in accordance with instructions from the
patient’s physician do not meet the definition of customized items. These items are not
uniquely constructed or substantially modified and can be grouped with other items for
pricing purposes. The use of customized options or accessories or custom fitting of
certain parts does not result in a wheelchair or other equipment being considered as
customized. The item must be uniquely constructed using raw materials or there must be
a necessary, substantial modification to the base equipment (e.g., wheelchair frame) for
the item to be considered a customized item.
Section 414.224 (b) provides that payment is made for the lump sum purchase of the item
based on the MAC’s individual consideration and judgment of a reasonable payment
amount for each customized item. The MAC’s individual consideration takes into
account written documentation on the costs (including design, fabrication, and assembly
costs) of the item including at least the cost of labor, to the extent that they are
reasonable, of those actually performing the customization. The MAC’s individual
consideration also takes into account the cost of the types of materials, to the extent that
they are reasonable, used in custom fabricating or substantially modifying an item. The
MAC may need to require a detailed description of each phase of the construction process
and labor skills needed to fabricate or modify the item in order to determine a reasonable
amount.
MACs shall submit quarterly reports to CMS on the items they have determined meet the
definition of customized items and how they reached the conclusion for each item.
MACs shall include in these reports the reasonable payment amount determinations and
factors they considered in determining the reasonable payment amount for each item.
The definition of customized DME set forth in regulations at 42 CFR Section 414.224 is
based on the longstanding definition of customized DME used in making decisions
regarding when to make individual payment determinations outside the normal process
for calculating customary and prevailing charges under the reasonable charge payment
methodology used for DME prior to 1989. Public Law 101-508, Omnibus Budget
Reconciliation Act (OBRA), November 5, 1990 (104 Stat. 1388-79) amended the criteria
for treatment of wheelchair as ‘a customized item at section 1834 (a) (4) of the Social
Security Act by adding a clause that in case of a wheelchair furnished on or after January
1, 1992, the wheelchair shall be treated as a customized item if the wheelchair has been
measured, fitted, or adapted in consideration of the patient’s body size, disability period
of need, or intended use, and has been assembled by a supplier or ordered from a
manufacturer who makes available customized features, modification or components for
wheelchairs that are intended for an individual patient’s use in accordance with
instructions from the patient’s physician. The amendment further noted that this clause
applied only to items furnished on or after January 1, 1992, unless the Secretary
developed specific criteria before that date for the treatment of wheelchairs as customized
items for purposes of section 1834(a) (4) of the Social Security Act (in which case the
amendment made by such clause would not become effective.’ CMS issued an interim
final rule on December 20, 1991 (56 FR 65995) to announce the decision not to use the
optional definition of customized wheelchairs in section 1834 (a) (4) of the Act and add a
new section 414.224 to 42 CFR to provide in regulation criteria that must be met for a
covered item to be considered a customized item for payment purposes. The final rule
(58 FR 34919) was published on June 30, 1993.
NOTE: MACs must observe that the alternative definition of customized wheelchairs
found in section 1834(a)(4) of the Act was never adopted for Medicare payment purposes
and should not be confused with the definition of customized items at 42 CFR 414.224.
30.4 - Other Prosthetic and Orthotic Devices
(Rev. 1, 10-01-03)
A3-3629
For payment purposes, these items consist of all prosthetic and orthotic devices
excluding:

• items requiring frequent and substantial servicing;
• customized items;
• parenteral/enteral nutritional supplies and equipment; and
• intraocular lenses.
Other than these exceptions, A/B MACs (A), (B), (HHH), and DME MACs pay the fee
schedule amounts for prosthetic and orthotic devices on a lump-sum purchase basis.
30.5 - Capped Rental Items
(Rev. 1, 10-01-03)
For these items of DME, A/B MACs (HHH) and DME MACs pay the fee schedule
amounts on a monthly rental basis not to exceed a period of continuous use of 15 months.
In the tenth month of rental, the beneficiary is given a purchase option (see §30.5.2). If
the purchase option is exercised, A/B MACs (HHH) and DME MACs continue to pay
rental fees not to exceed a period of continuous use of 13 months and ownership of the
equipment passes to the beneficiary. If the purchase option is not exercised, A/B MACs
(HHH) and DME MACs continue to pay rental fees until the 15 month cap is reached and
ownership of the equipment remains with the supplier (see §30.5.4). In the case of
electric wheelchairs only, the beneficiary must be given a purchase option at the time the
equipment is first provided (see §30.5.3).
30.5.1 - Capped Rental Fee Variation by Month of Rental
(Rev. 1, 10-01-03)
For the first three rental months, the capped rental fee schedule is calculated so as to limit
the monthly rental to 10 percent of the average of allowed purchase prices on assigned
claims for new equipment during a base period, updated to account for inflation. For
each of the remaining months, the monthly rental is limited to 7.5 percent of the average
allowed purchase price. After paying the rental fee schedule amount for 15 months, no
further payment may be made except for the 6-month maintenance and servicing fee (see
§40.2).
30.5.2 - Purchase Option for Capped Rental Items
(Rev. 1, 10-01-03)
Effective May 1, 1991, suppliers must give beneficiaries the option of converting their
capped rental equipment to purchased equipment during their 10th continuous rental
month. DME MACs and A/B MACs (HHH) make no further rental payments after the
11th rental month for capped rental items until the supplier notifies the DME MAC or
A/B MAC (HHH) that it has contacted the beneficiary and furnished him/her with the
option of either purchase or continued rental. Information contained in Exhibit 1 may be
furnished to beneficiaries by suppliers to help them make a rent/purchase decision. DME
MACs and A/B MACs (HHH) provide copies of Exhibit 1 to suppliers. Beneficiaries
have one month from the date the supplier makes the offer to accept this option. If the

beneficiary declines or fails to respond to the purchase option, the A/B MAC (HHH) or
DME MAC continues to make rental payments until the 15-month rental cap is reached.
If the beneficiary accepts the purchase option, the DME MAC or A/B MAC (HHH)
continues making rental payments until a total of 13 continuous rental months have been
paid. The DME MAC or A/B MAC (HHH) will not make any additional rental payments
beyond the 13th rental month. On the first day after 13 continuous rental months have
been paid, the supplier must transfer title to the equipment to the beneficiary.
30.5.3 - Additional Purchase Option for Electric Wheelchairs
(Rev. 1, 10-01-03)
Effective May 1, 1991, suppliers must give beneficiaries entitled to electric wheelchairs
the option of purchasing them at the time the supplier first furnishes the item. DME
MACs or A/B MACs (HHH) make no rental payment for the first month for electric
wheelchairs until the supplier notifies the MAC that it has given the beneficiary the
option of either purchasing or renting. Information contained in Exhibit 2 may be
furnished to beneficiaries by suppliers to help them make a rent/purchase decision.
MACs provide copies of Exhibit 2 to suppliers. Payment must be on a lump-sum fee
schedule purchase basis where the beneficiary chooses the purchase option. If the
beneficiary declines to purchase the electric wheelchair initially, MACs make rental
payments in the same manner as any other capped rental item, including the instructions
in §30.5.2.
30.5.3.1 - Exhibits
(Rev. 1, 10-01-03)
Exhibit 1 - The Rent/Purchase Option
You have been renting your (specify the item(s) of equipment) for 10 continuous rental
months. Medicare requires (specify name of supplier) to give you the option of
converting your rental agreement to a purchase agreement. This means that if you accept
this option, you would own the medical equipment. If you accept the purchase option,
Medicare continues making rental payments for your equipment for 3 additional rental
months. You are responsible for the 20 percent coinsurance amounts and, for unassigned
claims, the balance between the Medicare allowed amount and the supplier's charge.
After making these additional rental payments, title to the equipment is transferred to
you. You have until (specify the date one month from the date the supplier notifies the
patient of this option) to elect the purchase option. If you decide not to elect the purchase
option, Medicare continues making rental payments for an additional 5 rental months, a
total of 15 months. You are responsible for the 20 percent coinsurance amounts and, for
unassigned claims, the balance between the Medicare allowed amount and the supplier's
charge. After a total of 15 rental months have been paid, title to the equipment remains
with the medical equipment supplier; however, the supplier may not charge you any
additional rental amounts.
In making your decision to rent or purchase the equipment, you should know that for
purchased equipment your supplier may charge you each time your equipment is actually
serviced. You are responsible for the 20 percent coinsurance amounts and, for
unassigned claims, the balance between the Medicare allowed amount and the supplier's
charge. However, for equipment that is rented for 15 months, your responsibility for
such service is limited to 20 percent coinsurance on a maintenance and servicing fee
payable twice per year whether or not the equipment is actually serviced.
Exhibit 2 - How Medicare Pays For Electric Wheelchairs
(Rev. 1, 10-01-03)
If you need an electric wheelchair prescribed by your doctor, you may already know that
Medicare can help pay for it. Medicare requires (specify name of supplier) to give you
the option of either renting or purchasing it. If you decide that purchase is more
economical, for example, because you will need the electric wheelchair for a long time,
Medicare pays 80 percent of the allowed purchase price in a lump sum amount. You are
responsible for the 20 percent coinsurance amounts and, for unassigned claims, the
balance between the Medicare allowed amount and the supplier's charge. However, you
must elect to purchase the electric wheelchair at the time your medical equipment
supplier furnishes you the item. If you elect to rent the electric wheelchair, you are again
given the option of purchasing it during your 10th rental month.
If you continue to rent the electric wheelchair for 10 months, Medicare requires (specify
name of supplier) to give you the option of converting your rental agreement to a
purchase agreement. This means that if you accept this option, you would own the
medical equipment. If you accept the purchase option, Medicare continues making rental
payments for your equipment for 3 additional rental months. You are responsible for the
20 percent coinsurance amounts and, for unassigned claims, the balance between the
Medicare allowed amount and the supplier's charge. After these additional rental
payments are made, title to the equipment is transferred to you. You have until (specify
the date one month from the date the supplier notifies the patient of this option) to elect
the purchase option. If you decide not to elect the purchase option, Medicare continues
making rental payments for an additional 5 rental months, a total of 15 months. After a
total of 15 rental months have been paid, title to the equipment remains with the medical
equipment supplier; however, the supplier may not charge you any additional rental
amounts.
In making your decision to rent or purchase the equipment, you should know that for
purchased equipment, you are responsible for 20 percent of the service charge each time
your equipment is actually serviced and, for unassigned claims, the balance between the
Medicare allowed amount and the supplier's charge. However, for equipment that is
rented for 15 months, your responsibility for such service is limited to 20 percent
coinsurance on a maintenance and servicing fee payable twice per year whether or not the
equipment is actually serviced.

30.5.4 - Payments for Capped Rental Items During a Period of
Continuous Use
(Rev. 1, 10-01-03)
When no purchase options have been exercised, rental payments may not exceed a period
of continuous use of longer than 15 months. For the month of death or discontinuance of
use, DME MACs and A/B MACs (HHH) pay the full month rental. After 15 months of
rental have been paid, the supplier must continue to provide the item without any charge,
other than for the maintenance and servicing fees (see §40.2) until medical necessity ends
or Medicare coverage ceases (e.g., the patient enrolls in an M+C organization). For this
purpose, unless there is a break in need for at least 60 days, medical necessity is
presumed to continue. If a supplier makes any additional rental charges, DME MACs
and A/B MACs (HHH) should report questionable situations to the RO of the Inspector
General.
A period of continuous use allows for temporary interruptions in the use of equipment.
Interruptions may last up to 60 consecutive days plus the days remaining in the rental
month (this does not mean calendar month, but the 30-day rental period) in which use
ceases, regardless of the reason the interruption occurs. Thus, if the interruption is less
than 60 consecutive days plus the days remaining in the rental month in which use ceases,
DME MACs and A/B MACs (HHH) will not begin a new 15-month rental period. Also,
when an interruption continues beyond the end of the rental month in which the use
ceases, MACs will not make payment for additional rental until use of the item resumes.
MACs will establish a new date of service when use resumes. Unpaid months of
interruption do not count toward the 15-month limit.
EXAMPLE: A patient rents an item of equipment for 12 months and is then
institutionalized for 45 days. Upon his discharge from the institution, the patient resumes
use of the equipment and is considered to be in his 13th month of rental (since the period
of institutionalization is not counted) for purposes of calculating the 15-month rental
period. Moreover, for the period he was institutionalized, no payment is made for the
item of equipment. If the supplier desires, it may pick up the item of equipment during
the patient's hospitalization but is required to return the item upon the patient's return
home.
If, however, the interruption is greater than 60 consecutive days (plus the days remaining
in the rental month in which need ceases) and the supplier submits a new prescription,
new medical necessity documentation and a statement describing the reason for the
interruption which shows that medical necessity in the prior episode ended, a new 15-
month period begins. If the supplier does not submit this documentation, a new 15-
month period does not begin.
As a general rule, DME MACs and A/B MACs (HHH) accept written documentation
from suppliers without further development. However, although it is expected that such
circumstances are limited in number, they do represent an opportunity for abuse.
Therefore, if a pattern of frequent interruptions in excess of 60 days occurs, MACs will

institute a thorough medical review of the supplier's claims. MACs should report
questionable situations to the RO of the Inspector General.
If a 15-month rental period has already ended and a greater than 60 consecutive day
interruption occurs, MACs will subject any claims purporting to be a new period of
medical necessity after the interruption to a thorough medical review to ensure that
medical necessity did in fact end after the prior episode.
Additional issues relating to the term "continuous" follow.
Change of Address
If the beneficiary moves during or after the 15-month period, either permanently or
temporarily, it does not result in a new rental episode.
Modifications or Substitutions of Equipment
If the beneficiary changes equipment to different but similar equipment, DME MACs and
A/B MACs (HHH) may refer the claim to their medical review unit. If, after thorough
review, they conclude that the beneficiary's medical needs have substantially changed and
the new equipment is necessary, DME MACs will begin a new 15-month period. The
supplier providing equipment during the 10
th
month must also provide the purchase
option. Otherwise, they will continue to count against the current 15-month limit and
base payment on the least expensive medically appropriate configuration of equipment (if
the 15-month period had already expired, they will make no additional rental payments).
The principles are described in the Medicare Benefit Policy Manual, Chapter 15.
If the new configuration is a modification of existing equipment through the addition of
medically necessary features (e.g., a special purpose back is added to a wheelchair),
DME MACs and A/B MACs will continue the 15-month rental period for the original
equipment and begin a new 15-month rental period for the added equipment.
Change in Suppliers
If the beneficiary changes suppliers during or after the 15-month rental period, this does
not result in a new rental episode. For example, if the beneficiary changes suppliers after
his 8th rental month, the new supplier is entitled to the monthly rental fee for seven
additional months (15 - 8). The supplier that provides the item in the 15th month of the
rental period is responsible for supplying the equipment and for maintenance and
servicing after the 15-month period (see §40.2).
30.5.5 - Payment for Power-Operated Vehicles that May Be
Appropriately Used as Wheelchair
(Rev. 1, 10-01-03)
B3-5107.1

The allowed payment amount for a power-operated vehicle that may be appropriately
used as wheelchair, including all medically necessary accessories, is the lowest of the:
• Actual charge for the power-operated vehicle, or
• Fee schedule amount for the power-operated vehicle.
30.6 - Oxygen and Oxygen Equipment
(Rev. 11429; Issued: 05-23-22; Effective: 09-27-21; Implementation: 01-03-23)
For oxygen and oxygen equipment, A/B MACs (A) and (HHH), and DME MACs pay a
monthly fee schedule amount per beneficiary. Unless otherwise noted below, the fee
covers equipment, contents and supplies. Payment is not made for purchases of this type
of equipment.
When an inpatient is not entitled to Part A, payment may not be made under Part B for
DME or oxygen provided in a hospital or SNF. (See the Medicare Benefit Policy
Manual, Chapter 15) Also, for outpatients using equipment or receiving oxygen in the
hospital or SNF and not taking the equipment or oxygen system home, the fee schedule
does not apply.
There are a number of billing considerations for oxygen claims. The chart in §130.6
indicates what amounts are payable under which situations.
Home Use of Oxygen
Effective for claims with dates of service on or after September 27, 2021, contractors
shall be aware that the Centers for Medicare & Medicaid Services has reconsidered and
revised National Coverage Determination (NCD) for Home Use of Oxygen (240.2).
Claims for home use of oxygen and oxygen equipment must meet the coverage
requirements described under Chapter 1, Section 240.2, Publication 100-03 of the NCD
Manual.
Home Oxygen Use to Treat Cluster Headache
Effective for claims between February 14, 2011 and September 26, 2021, payment for the
home use of oxygen and oxygen equipment when related to the treatment of cluster
headaches is covered under a National Coverage Determination (NCD). For more
information, refer to chapter 1, section 240.2.2, Publication 100-03, of the National
Coverage Determinations Manual.
Effective for claims with dates of service on or after September 27, 2021, contractors
shall be aware that the Centers for Medicare & Medicaid Services removed the
Coverage with Evidence Development (CED) NCD for Home Oxygen Use to Treat
Cluster Headache (240.2.2) in Chapter 1, Section 240.2.2, Publication 100-03 of the
NCD Manual. In the absence of an NCD, coverage determinations will be made by the
Medicare Administrative Contractors under section 1862(a)(1)(A) of the Social
Security Act, as allowed and described in Chapter 1, Section 240.2 (Home Use of
Oxygen), Subsection D, of Publication 100-03 of the NCD Manual.
30.6.1 - Adjustments to Monthly Oxygen Fee
(Rev. 1, 10-01-03)
If the prescribed amount of oxygen is less than 1 liter per minute, the fee schedule
amount for stationary oxygen rental is reduced by 50 percent.
The fee schedule amount for stationary oxygen equipment is increased under the
following conditions. If both conditions apply, A/B MACs (A), (B), (HHH), and DME
MACs use the higher of either of the following add-ons. A/B MACs (A), (B), (HHH),
and DME MACs may not pay both add-ons:
a. Volume Adjustment - If the prescribed amount of oxygen for stationary equipment
exceeds 4 liters per minute, the fee schedule amount for stationary oxygen rental
is increased by 50 percent. If the prescribed liter flow for stationary oxygen is
different than for portable or different for rest and exercise, A/B MACs (A), (B),
(HHH), and DME MACs use the prescribed amount for stationary systems and
for patients at rest. If the prescribed liter flow is different for day and night use,
A/B MACs (A), (B), (HHH), and DME MACs use the average of the two rates.
b. Portable Add-on - If portable oxygen is prescribed, the fee schedule amount for
portable equipment is added to the fee schedule amount for stationary oxygen
rental.
30.6.2 - Purchased Oxygen Equipment
(Rev. 1, 10-01-03)
A/B MACs (A) or (HHH), and DME MACs may not pay for oxygen equipment that is
purchased on or after June 1, 1989.
30.6.3 - Contents Only Fee
(Rev. 1, 10-01-03)
Where the beneficiary owns stationary liquid or gaseous oxygen equipment, the A/B
MAC (A), (B), (HHH), or DME MAC pays the monthly oxygen contents fee. For owned
oxygen concentrators, however, A/B MAC (A), (B), (HHH), or DME MAC do not pay a
contents fee.
Where the beneficiary either owns a concentrator or does not own or rent a stationary
gaseous or liquid oxygen system and has either rented or purchased a portable system,
A/B MAC (A), (B),and (HHH), or DME MAC pay the portable oxygen contents fee.
30.6.4 - DMEPOS Clinical Trials and Demonstrations
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
The definition of the QR modifier is “item or service has been provided in a Medicare
specified study.” When this modifier is attached to a HCPCS code, it generally means
the service is part of a CMS related clinical trial, demonstration or study.
• The DME MACs shall recognize the “QR” modifier when associated with an
oxygen home therapy clinical trial identified by CMS and sponsored by the National
Heart, Lung & Blood Institute. DME MACs shall pay these claims if the patient’s
arterial oxygen partial measurements are from 56 to 65 mmHg, or whose oxygen
saturation is at or above 89%.
The definition of condition code 30 is “qualified clinical trial.” When this condition code
is reported on a claim, it generally means the service is part of a CMS related clinical
trial, demonstration or study.
The A/B MACs (HHH) shall recognize condition code 30, accompanied by ICD-9-CM
diagnosis code V70.7 or ICD-10 diagnosis code Z00.6, as applicable, in the second
diagnosis code position, when associated with an oxygen home therapy clinical trial
identified by CMS and sponsored by the National Heart, Lung & Blood Institute. A/B
MACs (HHH) shall pay these claims if the patient’s arterial oxygen partial measurements
are from 56 to 65 mmHg, or whose oxygen saturation is at or above 89%.
30.7 - Payment for Parenteral and Enteral Nutrition (PEN) Items and
Services
(Rev. 1, 10-01-03)
Payment for PEN items and services is made in a lump sum for nutrients and supplies
that are purchased and on a monthly basis for equipment that is rented.
30.7.1 - Payment for Parenteral and Enteral Pumps
(Rev. 1, 10-01-03)
B3-5017; PM B-01-54
Effective April 1, 1990, claims for rental of parenteral and enteral pumps are limited to
payments for a total of 15 months during a period of medical need. Payment policies for
these pumps generally follow the rules for capped rental items.
A period of medical need ends when enteral or parenteral nutrients are not medically
necessary for 2 consecutive months.
DME MACs do not allow additional rental payments once the 15-month limit is reached
or pump is purchased unless the attending physician changes the prescription between
parenteral and enteral nutrients.
DME MACs do not begin a new 15-month rental period when a patient changes
suppliers. The new supplier is entitled to the balance remaining on the 15-month rental
period.
The supplier that collects the last month of rental (i.e., 15th month) is responsible for
ensuring that the patient has a pump for the duration of medical necessity and for
maintenance and servicing (M/S) of the pump during the duration of therapy.
A period of voluntary non-billing care and institutional care is not counted toward the 15
months. Calculation is resumed when the voluntary care ends or when the patient is
released from institutional care.
An entire month's rent may not be paid when a patient is hospitalized during the month.
The DME MAC will request documentation to verify a break in medical need of two
months or more before approving an additional 15-month rental period.
DME MACs notify the supplier of the last rental payment.
The patient has the option of purchasing or renting the pump from the supplier. DME
MACs must request written authorization from the patient before or after paying for a
pump purchase. If the patient decides to purchase the pump once rentals have been paid,
the purchase allowance will consist of the used purchase allowance less the amount
allowed to date for rentals.
DME MACs provide coverage for one pump for parenteral nutrition. DME MACs do not
allow additional benefits for portable pumps or additional pumps.
30.7.2 - Payment for PEN Supply Kits
(Rev. 1, 10-01-03)
Enteral care kits contain all the necessary supplies for the enteral patient using the
syringe, gravity, or pump method of nutrient administration. Parenteral nutrition care kits
and their components are considered all-inclusive items necessary to administer therapy
during a monthly period.
The DME MAC compares the enteral feeding care kits on the claim with the method of
administration indicated on the CMN.
The allowance for the amount paid for a gravity-fed care kit is paid when a pump feeding
kit is billed in the absence of documentation or unacceptable documentation for a pump.
Payment is denied for additional components included as part of the PEN supply kit.
30.8 - Payment for Home Dialysis Supplies and Equipment
(Rev. 2487, Issued: 06-08-12, Effective: 01-01-11, Implementation: 06-19-12)
B3-4272, B3-4272.1 partial, A3-3644, B3-3045.7
For dates of service prior to January 1, 2011, there are two methods of payment for home
dialysis equipment and supplies: Method I and Method II.
Under Method I, benefits are paid by A/B MAC (A) on the basis of a prospective
payment, the composite rate. (See Chapters 8 and 12. for more information on
establishing the composite rate).
Under Method II, the DME MAC paid for supplies and services other than physician
services. Physician services are paid at a monthly capitation rate by the A/B MAC (B).
See Chapters 8 and 12 for more information on payment under Method II.
For dates of service on and after January 1, 2011, please refer to Section 30.8.3 for
information on the elimination of Method II home dialysis.
30.8.1 - DME MAC and A/B MAC (A) Determination of ESRD Method
Selection
(Rev. 2487, Issued: 06-08-12, Effective: 01-01-11, Implementation: 06-19-12)
AB-01-61
A. Method Selection and Form CMS-382
For services furnished prior to January 1, 2011, the beneficiary was required to complete
Form CMS-382 to choose either Method I or Method II dialysis. Method I dialysis
patients receive their home dialysis equipment and supplies from a dialysis facility.
Method II patients chose to deal with a home dialysis supplier that is not a dialysis
facility. Once a beneficiary made a method selection choice, the beneficiary or dialysis
facility submitted the Form CMS-382 to the appropriate A/B MAC (A). The A/B MAC
(A) then processed information from the form to CWF. Chapter 8 provided the
instructions for completing the form.
For dates of service prior to January 1, 2011, the DME MACs deny Method II claims
where there is no method selection or the method selection has a value of '1' on file at
CWF.
For dates of service on and after January 1, 2011, please refer to Section 30.8.3 for
information on the elimination of Method II home dialysis.
B. Changes in Method Selection
Prior to the implementation of the ESRD PPS, for dates of service prior to January 1,
2011, if a beneficiary decided to change his or her choice of method selection, he or she
filled out a new Form CMS-382 to indicate the change. The beneficiary could have filled
out a new method selection form at any time, but in most circumstances, the change did
not take effect until January 1 of the following calendar year. If a beneficiary requested
an exception to the January 1 implementation date in writing from the A/B MAC (A), the
A/B MAC (A) could have chosen to grant his or her request. See Chapter 8 for related
requirements.
The DME MAC systems must be able to interpret the CWF trailer record that contains
the method effective date.
For dates of service on and after January 1, 2011, please refer to Section 30.8.3 for
information on the elimination of Method II home dialysis.
30.8.2 - Installation and Delivery Charges for ESRD Equipment
(Rev. 2487, Issued: 06-08-12, Effective: 01-01-11, Implementation: 06-19-12)
3-5105.1
ESRD facilities are responsible for all reasonable and necessary expenses incurred in the
initial installation of home dialysis equipment, but not those expenses attributable to
items that are basically for the purpose of improving the patient's home, e.g., plumbing or
electrical work beyond that necessary to tie in with existing power or water lines.
The delivery and installation of renal dialysis equipment, unlike that involved when a
hospital bed is delivered and set up, requires testing and assurance of equipment
performance. Therefore, if the supplier of home dialysis equipment customarily charges
for delivery and service, and this is a common practice among other suppliers as well,
this is payable.
30.8.3 - Elimination of Method II Home Dialysis
(Rev. 2487, Issued: 06-08-12, Effective: 01-01-11, Implementation: 06-19-12)
Effective for dates of service on and after January 1, 2011, Section 153b of the Medicare
Improvements for Patients and Providers Act (MIPPA) eliminated Method II home
dialysis claims. Specifically, Method II home dialysis is no longer recognized as a
beneficiary option for dates of services beginning January 1, 2011, therefore, all ESRD
patients that previously selected Method II are covered under Method I. All home
dialysis claims must be billed by an ESRD facility and paid under the ESRD PPS. As a
result, the submission of the CMS-382 form to the A/B MACs (A) or DME MACs is no
longer required for home dialysis patients on or after January 1, 2011.
Method II claims will not be accepted for dates of service on or after January 1, 2011.
Method II claims for dates of service prior to January 1, 2011 will continue to be
processed within normal timely filing limitations. For more information on timely filing,
see Pub. 100-04, Chapter 1, Sections 70 through 70.8.6.

For dates of service on or after January 1, 2011, MACs shall continue to allow separate
billing for certain ESRD supply HCPCS codes subject to the ESRD PPS consolidated
billing requirements when submitted by suppliers for services not related to the
beneficiary’s ESRD dialysis treatment and billed with the modifier AY. MACs shall pay
for ESRD supplies subject to ESRD CB when billed on a CMS-1500 or electronic
equivalent if the ESRD supply claims contain modifier AY. A list of equipment and
supplies eligible for separate payment when billed with modifier AY can be found in the
first table (DME ESRD Supply HCPCS for ESRD PPS Consolidated Billing Edits) of the
document titled “Items and Services Subject to Consolidated Billing for the ESRD PPS”
located at the ESRD Payment website:
http://www.cms.gov/ESRDPayment/50_Consolidated_Billing.asp#TopOfPage.
Some equipment and supplies are ESRD-related but are not used in other provider
settings and will, therefore, never be used for reasons other than for the treatment of
ESRD. These equipment and supplies can be found listed in the second table (DME
ESRD Supply HCPCS Not Payable to DME Suppliers) of the document titled “Items and
Services Subject to Consolidated Billing for the ESRD PPS” located at the ESRD
Payment website:
http://www.cms.gov/ESRDPayment/50_Consolidated_Billing.asp#TopOfPage. DME
suppliers will not be capable of billing and being paid for any of the supplies on this list
using the AY modifier.
30.9 – Payment of DMEPOS Items Based on Modifiers
(Rev. 3824, Issued: 08-02-17; Effective: 07-01-17, Implementation: 07-03-17)
The following modifiers were added to the HCPCS to identify supplies and equipment
that may be covered under more than one DMEPOS benefit category:
• AU Item furnished in conjunction with a urological, ostomy, or tracheostomy
supply;
• AV Item furnished in conjunction with a prosthetic device, prosthetic or
orthotic; and
• AW Item furnished in conjunction with a surgical dressing.
Codes A4450 and A4452 are the only codes that have been identified at this time that
would require use of all three of the above listed modifiers. Providers must report these
modifiers on claims for items identified by codes A4450 and A4452 that are furnished
on or after January 1, 2005. Modifier AU may also be applicable to code A4217.
Providers must report modifier AU on claims for items identified by code A4217 that
are furnished in conjunction with a urological, ostomy, or tracheostomy supply on or
after January 1, 2005. Items identified by code A4217 that are furnished in conjunction
with durable medical equipment are reported without a modifier. In the future, other
codes may be identified as codes that must be submitted with these modifiers. Medicare
contractors base payment for the codes A4217, A4450, and A4452 on the presence or

absence of these modifiers.
Codes L8040 thru L8047 describe facial prostheses. Providers must report the
following modifiers on claims for replacement of these items:
• KM Replacement of facial prosthesis including
• g new impression/moulage; and
• KN Replacement of facial prosthesis using previous master model.
Providers must report these modifiers on claims for replacement of items identified by
codes L8040 thru L8047 that are furnished on or after January 1, 2005. Medicare
contractors base payment for the codes L8040 thru L8047 on the presence of these
modifiers. These modifiers are only used when the prostheses is being replaced.
In accordance with section 302(c) of the Medicare Prescription Drug, Improvement,
and Modernization Act of 2003 (MMA), the fee schedule update factors for 2004 thru
2008 for durable medical equipment (DME), other than items designated as class III
devices by the Food and Drug Administration (FDA), are equal to 0 percent. The
HCPCS codes for DME designated as class III devices by the FDA are identified on
the DMEPOS fee schedule available on the above mentioned web site by presence of
the KF modifier.
Elevating/stair climbing power wheelchairs are class III devices. Suppliers billing the
DMERCs must submit claims for the base power wheelchair portion of this device
using HCPCS code K0011 (programmable power wheelchair base) with modifier KF
for claims submitted on or after April 1, 2004, with dates of service on or after January
1, 2004. For claims with dates of service on or after January 1, 2004, the elevation
feature for this device should be billed using HCPCS code E2300 and the stair
climbing feature for this device should be billed using HCPCS code A9270.
Regional home health intermediaries (RHHIs) will not be able to implement the KF
modifier until January 1, 2005. Therefore, for claims with dates of service prior to
January 1, 2005, HHAs must submit claims for the base power wheelchair portion of
stair climbing wheelchairs with HCPCS code E1399. For claims with dates of service
on or after January 1, 2005, HHAs must submit claims for the base power wheelchair
portion of stair climbing wheelchairs with HCPCS code K0011 with modifier KF.
The fee schedule amounts for K0011 with and without the KF modifier appear on the
fee schedule file referenced at
www.cms.hhs.gov/providers/pufdownload/default.asp#dme. For claims with dates of
service prior to January 1, 2005, RHHIs should pay claims for stair climbing
wheelchair bases billed with code E1399 using the fee schedule amounts for K0011
with the KF modifier. All other claims for programmable power wheelchair bases
should be paid using the fee schedule amounts for K0011 without the KF modifier.
Effective for claims with dates of service on or after January 1, 2005, HHAs must
submit modifier KF along with the applicable HCPCS code for all DME items
classified by the FDA as class III devices.
The following modifier was added to the HCPCS in 2007 as a placeholder modifier:
• KU DMEPOS Item Subject to DMEPOS Competitive Bidding Program
Number 3
The DMEPOS fee schedules are updated on an annual basis in accordance with the
statute and regulations. The update process for the DMEPOS fee schedule is located
in Pub.100-04, Medicare Claims Processing Manual, chapter 23, section 60. Payment
on a fee schedule basis is required for certain durable medical equipment (DME) by
§1834(a) of the Social Security Act. Section1834(a)(1)(F)(ii) of the Act mandates
adjustments to the fee schedule amounts for certain DME items furnished on or after
January 1, 2016, including wheelchair accessories and seat and back cushions, in
areas that are not competitive bid areas, based on information from competitive
bidding programs (CBPs) for DME.
Section 2 of the Patient Access and Medicare Protection Act (PAMPA) mandates that
the adjusted fee schedule amounts for 2016 described above are not be applied to
wheelchair accessories and seat and back cushions furnished in connection with
Group 3 complex rehabilitative power wheelchairs described by codes K0848 through
K0864 of the Healthcare Common Procedure Coding System (HCPCS). Although this
change is effective January 1, 2016, it is not being implemented until July 1, 2016.
Until these changes are implemented, payment for these items will be based on the
adjusted fee schedule amounts.
Providers/suppliers can submit claims for these items with dates of service on or after
January 1, 2016, prior to July 1, 2016, but payment will be based on the adjusted fee
schedule amounts. On or after July 1, 2016, providers/suppliers can adjust previously
paid claims with dates of service on or after January 1, 2016, for the corrected fee
payment.
Providers/suppliers must use modifier “KU” for claims submitted on or after July
1, 2016, with dates of service on or after January 1, 2016, and before January 1,
2017, for any HCPCS code describing a wheelchair accessory or seat or back
cushion when furnished in connection with a Group 3 complex rehabilitative
power wheelchair.
Section 16005 of the 21
st
Century Cures Act modifies section 2(a) of the PAMPA to
require that the adjusted fee schedule amounts for 2017, described in section
1834(a)(1(F)(ii) of the Act, are not to be applied to wheelchair accessories and seat and
back cushions furnished in connection with Group 3 complex rehabilitative power
wheelchairs (described by HCPCS codes K0848 through K0864) prior to July 1, 2017.
Therefore, providers/suppliers should continue the use of the KU modifier on claim line
items for these accessories with dates of service after June 30, 2017. Effective July 1,
2017, CMS has taken into consideration the exclusion at section 1847(a)(2)(A) of the
Act to revise the policy. As a result, payment for these items furnished in connection
with a Group 3 complex rehabilitative power wheelchair and billed with the KU
modifier will be based on the unadjusted fee schedule amounts updated in accordance
with section 1834(a)(14) of the Act.
30.9.1 – Processing of Expatriate Beneficiary DMEPOS Claims for
Purchased Items Submitted with the EX Modifier
(Rev. 3491, Issued: 04-05-16, Effective: 07-01-16, Implementation: 07-05-16)
In accordance with section 1862(a)(4) of the Social Security Act, claims for DMEPOS
provided to Medicare beneficiaries living outside of the U.S. are payable as long as the
delivery occurred while the beneficiary was in the U.S. and the item is delivered to a U.S.
address.
Effective July 1, 2016, the modifier EX was developed to allow suppliers to bill Medicare
for purchased only DMEPOS items that are furnished to expatriate beneficiaries.
Suppliers should submit these claims based on their supplier locality, not based on the
beneficiary address. By attaching the EX modifier, the supplier is attesting that the
beneficiary is an expatriate beneficiary, and that the item was delivered/furnished while
the beneficiary is present in the U.S., and all other billing criteria has been met.
For purchased items only furnished on or after July 1, 2016, contractors shall accept the
EX modifier for processing. Contractors shall pay claims with the EX modifier for
Expatriate beneficiaries based on supplier locality.
Suppliers shall append modifier EX on all lines with a line item date of service.
Contractors shall automatically deny the claim(s), when all line(s) items have not been
submitted with an EX modifier.
If a beneficiary-submitted claim (1490S) is received, written attestation from the supplier
must also be included. Contractors shall deny the 1490S claim form with or without an
EX modifier if a supplier 1500 claim form including the EX modifier or a written
supplier attestation that the beneficiary was in the U.S. when the service was rendered is
not included with the 1490S.
The following items for expatriate beneficiary claims are not payable and should be
denied:
Oxygen Equipment and Supplies
Parenteral and Enteral Nutrition Equipment and Supplies
Rentals - capped or inexpensive, routinely purchased (IRP)
Contractors will apply National Mail Order (NMO) rules to expatriate claims.

NOTE: P.O. Boxes and Lock Boxes are not allowed for NMO or any delivery of
supplies for expatriate claims, and must be delivered to the beneficiary residence.
National Competitive Bid Program (CBP) rules shall apply to expatriate claims.
NOTE: An exception for the submission of paper claims for CBP is being granted for
expatriate claims.
The supplier must send paper claims to the supplier's jurisdiction for processing. If this
attestation is determined to be inaccurate, the supplier is subject to sanctions resulting
from providing inaccurate information on a claim.
40 - Payment for Maintenance and Service of Equipment
(Rev. 3196, Issued: 02-13-15, Effective: 07-01-15, Implementation: 07-06-15)
40.1 - General
(Rev. 3196, Issued: 02-13-15, Effective: 07-01-15, Implementation: 07-06-15)
A/B MACs (HHH), and DME MACs pay for reasonable and necessary maintenance and
servicing of purchased equipment in the following classes:
• inexpensive or frequently purchased,
• customized items, other prosthetic and orthotic devices, and
• capped rental items purchased in accordance with §30.5.2 and §30.5.3, or in
situations where rental claims have been paid but title to the equipment is
transferred to the beneficiary during a period of continuous use of less than 13
months.
Do not pay for maintenance and servicing of purchased items that require frequent and
substantial servicing, or purchased oxygen equipment. (Maintenance and servicing may
be paid for purchased items in these two classes if they were purchased prior to June 1,
1989). Reasonable and necessary charges include only those made for parts and labor
that are not otherwise covered under a manufacturer's or supplier's warranty. A/B MACs
(A), (B), (HHH), and DME MACs pay on a lump-sum, as needed basis based on their
individual consideration for each item. Payment may not be made for maintenance and
servicing of rented equipment other than maintenance and servicing for PEN pumps
(under the conditions of §40.3), the maintenance and servicing fee established for capped
rental items in §40.2, or the maintenance and servicing fee established for certain oxygen
equipment in 42 CFR 414.210(e)(2).
Servicing of equipment that a beneficiary is purchasing or already owns is covered when
necessary to make the equipment serviceable. The service charge may include the use of
"loaner" equipment where this is required. If the expense for servicing exceeds the
estimated expense of purchasing or renting another item of equipment for the remaining
period of medical need, no payment can be made for the amount of the excess. A/B
MACs (HHH), and DME MACs investigate and deny cases suggesting malicious
damage, culpable neglect or wrongful disposition of equipment as discussed in Pub.100-
02, Medicare Benefit Policy Manual, chapter 15 where they determine that it is
unreasonable to make program payment under the circumstances. Such cases are referred
to the program integrity specialist in the RO.
40.2 - Maintenance and Service of Capped Rental Items
(Rev. 3196, Issued: 02-13-15, Effective: 07-01-15, Implementation: 07-06-15)
For capped rental items furnished before January 1, 2006, which have reached the 13-
month rental cap, A/B MACs (HHH) and DME MACs pay claims for maintenance and
servicing fees after 6 months have passed from the end of the final paid rental month or
from the end of the period the item is no longer covered under the supplier's or
manufacturer's warranty, whichever is later.
The maintenance and servicing fee for capped rental items furnished before January 1,
2006, may be paid only once every 6 months. However, in the event the beneficiary
elected to purchase the equipment, maintenance and servicing are paid in accordance
with the instructions in §40.1.
For capped rental items furnished on or after January 1, 2006, A/B MACs (HHH) and
DME MACs shall pay for reasonable and necessary maintenance and servicing of
beneficiary-owned equipment following 13 months of continuous use or, in the case of
complex rehabilitative power wheelchairs, are acquired on a lump sum purchase basis. In
addition, in cases where one or more rental payments have been made for a capped rental
item, and the supplier transfers title to the equipment prior to the end of a 13 month
period of continuous use, A/B MACs (HHH) and DME MACs can pay for reasonable
and necessary maintenance and servicing of the beneficiary-owned equipment.
40.3 - Maintenance and Service of PEN Pumps
(Rev. 1, 10-01-03)
B3-5017.4
Effective October 1, 1990, necessary maintenance and servicing of pumps after the 15-
month rental limit is reached may include repairs and extensive maintenance that
involves the breaking down of sealed components, or performing tests that require
specialized testing equipment not available to the beneficiary or nursing home. The
DME MAC will pay only for actual incidents of maintenance, servicing, or replacement.
For enteral pumps, no more than one-half rental payment may be paid every six months,
beginning six months after the last rental payment. For parenteral pumps, no more than
one-half the rental payment may be paid every three months, beginning three months
after the last rental payment for the pump. The DME MAC requests written proof from
the supplier of maintenance and servicing of the pump.

50 - Payment for Replacement of Equipment
(Rev. 11414; Issued: 05-12-22; Effective: 06-13-22; Implementation: 06-13-22)
NOTE: CMS seeks to reduce burden and modernize processes to ensure a reduction in
improper payments and an increase in customer satisfaction. The Certificate of Medical
Necessity (CMN) form and DME Information Form (DIF) were originally required to
help document the medical necessity and other coverage criteria for selected Durable
Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items. In the past, a
supplier received a signed CMN from the treating physician or created and signed a DIF
to submit with the claim. Due to improvements in claims processing and medical records
management, the information found on CMNs or DIFs is available either on the claim or
in the medical record and is redundant. Therefore, to reduce burden and increase
customer satisfaction, providers and suppliers no longer need to submit these forms for
services rendered after January 1, 2023.
• For claims with dates of service on or after January 1, 2023 – providers and
suppliers no longer need to submit CMNs or DIFs with claims. Due to electronic
filing requirements, claims received with these forms attached will be rejected and
returned to the provider or supplier.
• For claims with dates of service prior to January 1, 2023 – processes will not
change and if the CMN or DIF is required, it will still need to be submitted with
the claim, or be on file with a previous claim.
This statement applies throughout the Program Integrity Manual wherever CMNs and
DIFs are mentioned.
B3-5102.2.B
Replacement of equipment which the beneficiary owns or is purchasing or is a capped
rental item is covered in cases of loss, or irreparable damage or wear, and when required
because of a change in the patient's condition subject to the following provisions.
Expenses for replacement required because of loss or irreparable damage may be
reimbursed without a physician's order when, in the DME MAC’s judgment, the
equipment as originally ordered, considering the age of the order, still fills the patient's
medical needs. However, claims involving replacement equipment necessitated because
of wear or a change in the patient's condition must be supported by a current physician's
order. (See the Medicare Benefit Policy Manual, Chapter 16, for payment for equipment
replaced under a warranty.)
DME MACs investigate and deny cases suggesting malicious damage, culpable neglect
or wrongful disposition of equipment as discussed in the Benefit Policy Manual, Chapter
15, where it is determined that it is unreasonable to make program payment under the
circumstances. They refer such cases to the program integrity specialist in the RO.
DME MACs do not pay for replacement of rented equipment except capped rental items.
(See §50.1) However, they pay for replacement of purchased equipment in the following
classes: inexpensive or routinely purchased, customized items, capped rental (where the
beneficiary has elected to purchase the item), and other prosthetic and orthotic devices.
They do not pay for purchase or replacement of items that require frequent and
substantial servicing or oxygen equipment.
50.1 - Payment for Replacement of Capped Rental Items
(Rev. 1, 10-01-03)
A3-3629
Effective May 1, 1991, if a capped rental item of equipment has been in continuous use
by the patient, on either a rental or purchase basis, for the equipment's useful lifetime or
if the item is lost or irreparably damaged, the patient may elect to obtain a new piece of
equipment. The MAC determines the reasonable useful lifetime for capped rental
equipment but in no case can it be less than five years. This is a different requirement
from that in the following section about prosthetic devices that are not capped rental.
Computation of the useful lifetime is based on when the equipment is delivered to the
beneficiary, not the age of the equipment. If the patient elects to obtain a new piece of
equipment, payment is made on a rental or purchase basis.
50.3 - Payment for Replacement of Parenteral and Enteral Pumps
(Rev. 1, 10-01-03)
B3-3324
Payment for replacement of PEN pumps purchased more than eight years prior to the
current date may be considered, with documentation that indicates proof of purchase date.
Medicare will consider payment for either a replacement by purchase or 15 months of
rental.
50.4 - Payment for Replacement of Oxygen Equipment in Bankruptcy
Situations
(Rev. 1961, Issued: 04-30-10, Effective: 10-01-10, Implementation: 10-04-10)
When a supplier files for Chapter 7 or 11 bankruptcy under Title 11 of the United
States Code and cannot continue to furnish oxygen to its Medicare beneficiaries, the
oxygen equipment is considered lost in these situations and payment may be made
for replacement equipment. For replacement oxygen equipment, a new reasonable
useful lifetime period and a new 36 month rental payment period begins on the date
of delivery of the replacement oxygen equipment.
In advance of payment, A/B MACs (HHH), and DME MACs must review supporting
documentation to verify that the supplier declared bankruptcy to assure that payment for
replacement of oxygen equipment can legitimately be made to a successor supplier.
• For a Chapter 7 bankruptcy, supporting documentation must include court records
documenting that the previous supplier filed a petition for a Chapter 7 bankruptcy
in a United States Bankruptcy Court,
• For a Chapter 11 bankruptcy, supporting documentation must include Court
records documenting that the previous supplier filed a petition for a Chapter 11
bankruptcy in a United States Bankruptcy Court; and documents filed in the
bankruptcy case confirming that the equipment was sold or is scheduled to be sold
as evidenced by one of the following:
o The Court order authorizing and/or approving the sale; or
o Supporting documentation that the sale is scheduled to occur or has occurred,
e.g., a bill of sale, or an asset purchase agreement signed by the seller and the
buyer; or
o A Court order authorizing abandonment of the equipment.
Similar to other situations where oxygen equipment is lost, stolen, or irreparably
damaged, the A/B MAC (HHH) or DME MAC must verify the following information is
included and valid with the claim: blood gas testing results, Oxygen Certificate of
Medical Necessity (CMN), the Healthcare Common Procedure Coding System (HCPCS)
code for the replacement oxygen equipment, the HCPCS modifier RA Replacement of a
DME Item, and a narrative note on why the equipment was replaced.
Under no circumstances may payment be made for replacement equipment when the
original supplier divests business and equipment outside of the court bankruptcy
process.
50.5 – Payment of a Part of a DMEPOS Item
(Rev. 3593, Issued: 08-17-16, Effective: 10-01-16, Implementation: 10-03-16)
The RB modifier is used on a DMEPOS claim to denote the replacement of a part of a
DMEPOS item (base equipment/device) furnished as part of the service of repairing the
DMEPOS item (base equipment/device). All repair part claims billed with the RB
modifier, whether within or outside a competitive bidding area, shall be paid on a lump
sum purchase basis.
Payment for repair parts that are described by HCPCS codes for competitive bidding
items and are furnished in competitive bidding areas for use in repairing base equipment
that are competitive bid items is made based on the single payment amount established
for the HCPCS code. Payment for such repair parts that are furnished for use in repairing
base equipment that are not competitive bidding items in the area is made in accordance
with 42 CFR 414.408(k)(1)(ii), which provides that payment for the part is made based
on the contractor’s consideration of the item under 42 CFR 414.210(e). When making
payment determinations for parts described by HCPCS codes for competitive bidding
items furnished for use in repairing base equipment that are not competitive bidding
items, contractors have discretion to use the single payment amounts for the item in
establishing the Medicare allowed amount for the repair part.

60 - Payment for Delivery and Service Charges for Durable Medical
Equipment
(Rev. 1, 10-01-03)
B3-5105
Delivery and service are an integral part of oxygen and durable medical equipment
(DME) suppliers' costs of doing business. Such costs are ordinarily assumed to have
been taken into account by suppliers (along with all other overhead expenses) in setting
the prices they charge for covered items and services. As such, these costs have already
been accounted for in the calculation of the fee schedules. Also, most beneficiaries reside
in the normal area of business activity of one or more DME supplier(s) and have
reasonable access to them.
Therefore, DME MACs may not allow separate delivery and service charges for oxygen
or DME except as specifically indicated in §§90 or in rare and unusual circumstances
when the delivery is not typical of the particular supplier's operation.
For example, there may be situations in which it is necessary for a DME dealer to incur
extraordinary delivery expenses in order to meet the needs of beneficiaries living in
remote areas that are not served by a local dealer or when a local dealer is temporarily out
of stock of required oxygen or equipment. For example, DME MACs may recognize a
reasonable separate delivery charge when the supplier must deliver an item of DME
outside its normal area of business activity and the beneficiary does not have access to a
supplier whose location is nearer.
When a supplier delivers oxygen or DME outside the area in which he/she normally does
business, but the item could have been obtained locally, DME MACs may allow any
separate additional delivery charge only to the extent that it does not raise the total
payment for the oxygen or DME above the local fee schedule.
When a separate charge can be allowed for delivery/service, DME MACs base the
amount (based on mileage or a flat rate) on all of the relevant circumstances, including:
• The time and distance traveled;
• The actual additional expenses incurred by the supplier;
• The type and quantity of equipment or oxygen delivered;
• The supplier's customary charge under such circumstances;
• The prevailing charges in the locality under such circumstances; and
• Delivery charges made elsewhere in similar localities. Any separate delivery
charges recognized because of unusual circumstances may, of course, be paid for
only for deliveries that have actually been made.
Suppliers must be advised in the DME MAC service areas to bill a separate delivery
charge only in those rare situations in which "unusual circumstances" were encountered.
Information issuances should be used to advise DME suppliers of the need to fully
document unusual circumstances on claims/bills for separate delivery charges. If a
supplier, nevertheless, routinely itemizes delivery charges, DME MACs may consider
payment for the charges to be included in the fee for the equipment.
80 - Penalty Charges for Late Payment Not Included in Reasonable
Charges or Fee Schedule Amounts
(Rev. 1, 10-01-03)
B3-5106.1
Penalty charges imposed on a beneficiary by a physician or supplier because of failure to
make timely payment on a bill are not covered under Medicare.
NOTE: The Judicial Council of the American Medical Association has ruled that, "It is
not in the best interest of the public or the profession to charge a penalty if fees for
professional services are not paid within a prescribed period of time, nor is it proper to
charge a patient a flat collection fee if it becomes necessary to refer the amount to an
agency for collection."
90 - Payment for Additional Expenses for Deluxe Features
(Rev. 1, 10-01-03)
B3-5107, PM AB-02-114
The payment amount for a given service or item, whether rented or purchased, must be
consistent with what is reasonable and medically necessary to serve the intended purpose
(See the Medicare Benefit Policy Manual, Chapter 15). Additional expenses for "deluxe"
features, or items that are rented or purchased for aesthetic reasons or added convenience,
do not meet the reasonableness test. Thus, where a service or item is medically necessary
and covered under the Medicare program, and the patient wishes to obtain such deluxe
features, the payment is based upon the payment amount for the kind of service or item
normally used to meet the intended purpose (i.e., the standard item.) Usually this is the
least costly item. DME MACs may, of course, determine that the payment amount for a
more expensive service or item is reasonable when the additional expense is for an added
feature that is medically necessary in a given case. For example, a more expensive item
may be medically necessary where a patient in a weakened condition needs a power-
operated wheelchair or a power-operated vehicle that may be appropriately used as a
wheelchair since the patient is not strong enough to operate a manual wheelchair.
Finally the provider may not charge the beneficiary for features not medically required by
his/her condition and which cannot be considered in determining the provider's allowable
costs unless the beneficiary or her/his representative has specifically requested the
excessive or deluxe items or services with knowledge of the amount s/he is to be charged.
An Advance Beneficiary Notification (ABN) is required as documentation that the
beneficiary has made such an informed request. See Chapter 30 for ABN requirements.
The acceptance of an assignment binds the supplier-assignee to accept the allowed charge
for the medically required equipment or service as the full charge and he cannot charge
the beneficiary the differential attributable to the equipment actually furnished.

Only if a more expensive item or model with special features is medically necessary for
the beneficiary will the allowed charge be based on the more expensive model. If the
patient purchases or rents an item of durable medical equipment having more expensive
features than his condition requires, the supplier accepting assignment on such an item
cannot charge or collect any amount in excess of the allowed charge for the appliance
adequate for the patient's needs. Acceptance of assignment binds the supplier to accept
the allowed charge determined by the DME MAC, as the full charge for the item. A
supplier who wishes to charge and collect the full price for equipment more expensive
than medically required by the patient need not accept assignment. In assignment cases,
the beneficiary is responsible for paying the supplier the unpaid balance of the allowed
charge when payments stop because his condition has changed and the equipment is no
longer medically necessary. Similarly, when payments stop because the beneficiary dies,
his/her estate is responsible to the supplier for such unpaid balance.
100 - General Documentation Requirements
(Rev. 11414; Issued: 05-12-22; Effective: 06-13-22; Implementation: 06-13-22)
NOTE: CMS seeks to reduce burden and modernize processes to ensure a reduction in
improper payments and an increase in customer satisfaction. The Certificate of Medical
Necessity (CMN) form and DME Information Form (DIF) were originally required to
help document the medical necessity and other coverage criteria for selected Durable
Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items. In the past, a
supplier received a signed CMN from the treating physician or created and signed a DIF
to submit with the claim. Due to improvements in claims processing and medical records
management, the information found on CMNs or DIFs is available either on the claim or
in the medical record and is redundant. Therefore, to reduce burden and increase
customer satisfaction, providers and suppliers no longer need to submit these forms for
services rendered after January 1, 2023.
• For claims with dates of service on or after January 1, 2023 – providers and
suppliers no longer need to submit CMNs or DIFs with claims. Due to electronic
filing requirements, claims received with these forms attached will be rejected and
returned to the provider or supplier.
• For claims with dates of service prior to January 1, 2023 – processes will not
change and if the CMN or DIF is required, it will still need to be submitted with
the claim, or be on file with a previous claim.
This statement applies throughout the Program Integrity Manual wherever CMNs and
DIFs are mentioned.
B3-4107.1, B3-4107.8, HHA-463, Medicare Handbook for New Suppliers: Getting
Started, B-02-31
Benefit policies are set forth in the Medicare Benefit Policy Manual, Chapter 15, §§110-
130.

Program integrity policies for DMEPOS are set forth in the Medicare Program Integrity
Manual, Chapter 5.
See Chapter 21 for applicable MSN messages.
See Chapter 22 for Remittance Advice coding.
100.1 - Written Order Prior to Delivery
(Rev. 1, 10-01-03)
See the Medicare Program Integrity Manual, Chapter 5, for requirements for written
orders for suppliers, including providers billing the DME MAC or A/B MAC (B) as
suppliers.
See §01 for definitions of provider and supplier.
100.1.1 - Written Order Prior to Delivery - HHAs
(Rev. 1, 10-01-03)
See the Medicare Program Integrity Manual, Chapter 6. These instructions apply to bill
types 32x, 33x and 34x.
100.2 - Certificates of Medical Necessity (CMN)
(Rev. 1, 10-01-03)
B3-3312
For certain items or services billed to the DME MAC, the supplier must receive a signed
Certificate of Medical Necessity (CMN) from the treating physician. CMNs are not
required for the same items when billed by HHAs to A/B MACs (HHH). Instead, the
items must be included in the physician's signed orders on the home health plan of care.
See the Medicare Program Integrity Manual, Chapter 6.
The A/B MAC (A) will inform other providers (see §01 for definition pf provider) of
documentation requirements.
DME MACs may ask for supporting documentation beyond a CMN.
Refer to the DME MAC Web site described in §10 for downloadable copies of CMN
forms.
See the Medicare Program Integrity Manual, Chapter 5, for specific Medicare policies
and instructions on the following topics:
• Requirements for supplier retention of original CMNs
• CMN formats, paper and electronic
• List of currently approved CMNs and items requiring CMNs
• Supplier requirements for submitting CMNs
• Requirements for CMNs to also serve as a physician's order
• Civil monetary penalties for violation of CMN requirements
• Supplier requirements for completing portions of CMNs
• Physician requirements for completing portions of CMNs
100.2.1 - Completion of Certificate of Medical Necessity Forms
(Rev. 4202, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a
beneficiary’s Medicare identification number. For purposes of this manual, Medicare
beneficiary identifier references both the Health Insurance Claim Number (HICN) and
the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
period and after for certain business areas that will continue to use the HICN as part of
their processes.
1. SECTION A: (This may be completed by supplier.)
a. Certification Type/Date - If this is an initial certification for this patient, the date
(MM/DD/YY) is indicated in the space marked "INITIAL". If this is a revised
certification (to be completed when the physician changes the order, based on the
patient's changing clinical needs), the initial date is indicated in the space marked
"INITIAL", and the revision date is indicated in the space marked "REVISED".
If this is a recertification, the initial date is indicated in the space marked
"INITIAL", and the recertification date is indicated in the space marked
"RECERTIFICATION". Whether a REVISED or RECERTIFIED CMN is
submitted, the INITIAL date as well as the REVISED or RECERTIFICATION
date is always furnished.
b. Patient Information - This indicates the patient's name, permanent legal address,
telephone number, and his/her Medicare beneficiary identifier as it appears on
his/her Medicare card and on the claim form.
c. Supplier Information - This indicates the name of the company (supplier name),
address, telephone number, and the Medicare supplier number assigned by the
National Supplier Clearinghouse (NSC).
d. Place of Service - This indicates the place in which the item is being used, i.e.,
patient's home is 12, skilled nursing facility (SNF) is 31, or end stage renal
disease (ESRD) facility is 65. See chapter 23 for place of service codes.
e. Facility Name - This indicates the name and complete address of the facility, if
the place of service is a facility.

f. HCPCS Codes - This is a list of all HCPCS procedure codes for items ordered
that require a CMN. Procedure codes that do not require certification are not
listed on the CMN.
g. Patient Date of Birth (DOB), Height, Weight, and Sex - This indicates patient's
DOB (MM/DD/YY), height in inches, weight in pounds, and sex (male or
female).
h. Physician Name and Address - This indicates the treating physician's name and
complete mailing address.
i. UPIN - This indicates the treating physician's unique physician identification
number (UPIN).
j. Physician's Telephone Number - This indicates the telephone number where the
treating physician can be contacted (preferably where records would be accessible
pertaining to this patient) if additional information is needed.
2. SECTION B: (This may not be completed by the supplier. While this section may
be completed by a non-physician clinician, or a physician employee, it must be reviewed
by the treating physician. A/B MACs (B) and (HHH) and DME MACs publish this
requirement about section B in their bulletins at least annually.)
a. Estimated Length of Need - This indicates the estimated length of need (the
length of time (in months) the physician expects the patient to require use of the
ordered item). If the treating physician expects that the patient will require the
item for the duration of his/her life, 99 is entered. For recertification and revision
CMNs, the cumulative length of need (the total length of time in months from the
initial date of need) is entered.
k. Diagnosis Codes - Listed in the first space is the diagnosis code that represents the
primary reason for ordering this item. Additional diagnosis codes that would
further describe the medical need for the item (up to 3 codes) are also listed. A
given CMN may have more than one item billed, and for each item, the primary
reason for ordering may be different. For example, a CMN is submitted for a
manual wheelchair (K0001) and elevating leg rests (K0195). The primary reason
for K0001 is stroke, and the primary reason for K0195 is edema.
l. Question Section - This section is used to gather clinical information regarding
the patient's condition, the need for the DME, and supplies.
m. Name of Person Answering Section B Questions - If a clinical professional other
than the treating physician (e.g., home health nurse, physical therapist, dietician,
or a physician employee) answers the questions in section B, he/she must print
his/her name, give his/her professional title, and the name of his/her employer,
where indicated. If the treating physician answered the questions, this space may
be left blank.
3. SECTION C: (This is completed by the supplier.)
a. Narrative Description of Equipment and Cost - The supplier indicates (1) a
narrative description of the item(s) ordered, as well as all options, accessories,
supplies, and drugs; (2) the supplier's charge for each item, option, accessory,
supply, and drug; and (3) the Medicare fee schedule allowance for each item,
option, accessory, supply, or drug, if applicable.
4. SECTION D: (This is completed by the treating physician.)
a. Physician Attestation - The treating physician's signature certifies the CMN that
he/she is reviewing includes sections A, B, C, and D, the answers in section B are
correct, and the self-identifying information in section A is correct.
b. Physician Signature and Date - After completion and/or review by the treating
physician of sections A, B, and C, the treating physician must sign and date the
CMN in section D, verifying the attestation appearing in this section. The treating
physician's signature also certifies the items ordered are medically necessary for
this patient. Signature and date stamps are not acceptable.
Certifications and recertifications may not be altered by "whiting out" or "pasting over"
and entering new data. Such claims are denied and suppliers that show a pattern of
altering CMNs are identified for educational contact and/or audit.
Also suppliers who have questionable utilization or billing practices or who are under
sanction are considered for audit.
100.2.2 - Evidence of Medical Necessity for Parenteral and Enteral
Nutrition (PEN) Therapy
(Rev. 1, 10-01-03)
B3-3324, B3-4450
The PEN coverage is determined by information provided by the treating physician and
the PEN supplier. A completed certification of medical necessity (CMN) must
accompany and support initial claims for PEN to establish whether coverage criteria are
met and to ensure that the PEN therapy provided is consistent with the attending or
ordering physician's prescription. DME MACs ensure that the CMN contains pertinent
information from the treating physician. Uniform specific medical data facilitate the
review and promote consistency in coverage determinations and timelier claims
processing.
The medical and prescription information on a PEN CMN can be most appropriately
completed by the treating physician or from information in the patient's records by an
employee of the physician for the physician's review and signature. Although PEN
suppliers sometimes may assist in providing the PEN services, they cannot complete the
CMN since they do not have the same access to patient information needed to properly
enter medical or prescription information. A/B MACs (B) and DME MACs use
appropriate professional relations issuances, training sessions, and meetings to ensure that
all persons and PEN suppliers are aware of this limitation of their role.
When properly completed, the PEN CMN includes the elements of a prescription as well
as other data needed to determine whether Medicare coverage is possible. This practice
will facilitate prompt delivery of PEN services and timely submittal of the related claim.
100.2.2.1 - Scheduling and Documenting Certifications and
Recertifications of Medical Necessity for PEN
(Rev. 1, 10-01-03)
A certification for PEN therapy must accompany the initial claim submitted. The initial
certification is valid for six months. DME MACs establish the schedule on a case-by-
case basis for recertifying the need for PEN therapy. A change in prescription for a
beneficiary past the initial certification period does not restart the certification process.
A period of medical necessity ends when PEN services are not medically required for 2
consecutive months. The entire certification process, if required, begins after 2
consecutive months have elapsed.
A revised certification or a change in prescription may impact on the payment levels of
PEN services. A revised certification is appropriate when there is a change:
• In the treating physician's orders in the category of nutrients and/or calories
prescribed;
• By more than one liter in the daily volume of parenteral solutions;
• From home-mix to pre-mix or pre-mix to home-mix parenteral solutions;
• From enteral to parenteral or parenteral to enteral therapy; or
• In the method of infusion (e.g., from gravity-fed to pump-fed).
100.2.2.2 - Completion of the Elements of PEN CMN
(Rev. 4202, Issued: 01-18-19, Effective: 02-19-19, Implementation: 02-19-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a
beneficiary’s Medicare identification number. For purposes of this manual, Medicare
beneficiary identifier references both the Health Insurance Claim Number (HICN) and
the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
period and after for certain business areas that will continue to use the HICN as part of
their processes.
The patient's name, address, and Medicare beneficiary identifier and the nature of the
certification (i.e., initial, renewed, or revised) must be entered on all certifications by the
supplier, physician, or physician's designated employees. The supplier identifying
information is required on all PEN certifications.
All medical and prescription information must be completed from the patient's records by
the attending/ordering physician, or an employee of the physician authorized to act on the
physician's behalf, and reviewed and signed by the physician.
1. Place of Service - The CMN must identify the site where the patient is receiving
PEN services. A patient may receive services at home, in a nursing home setting
(e.g., skilled nursing facility), or another site that must be indicated by the
supplier/physician.
2. Patient's General Condition - The attending physician must complete information
about the patient's age, height, and weight. The general condition of the patient
also includes an estimated duration of therapy (i.e., in months, years, or for life),
the ambulatory status, and whether the patient is conscious. The physician should
also indicate food allergies/sensitivities, other medical treatments, therapies,
and/or medical conditions that may affect the patient's nutritional needs.
3. Patient's Clinical Assessment - The attending physician must indicate all the
diagnoses related to the PEN therapy and describe the patient's functional
impairment of the digestive tract that precludes the enteral patient from
swallowing and the parenteral patient from absorbing nutrients. The physician
must certify that PEN therapy meets the requirement that a patient is not able to
maintain weight and strength due to pathology or nonfunction of the ingestion
system and that the enteral therapy serves as the source of nutrition for the patient
who has a functioning digestive tract, but whose disability prevents ingestion of
sufficient nutrients to the alimentary tract for metabolism. Nutritional
supplements for patients capable of ingesting normally, even if required to
maintain weight and strength, cannot be covered under the prosthetic device
benefit. The physician must have a basis for certifying or recertifying the need
for PEN services. The physician is expected to see the patient within 30 days
prior to certifying or recertifying PEN services. However, if the physician did not
see the patient, he/she must explain why and describe what other monitoring
methods were used to evaluate the patient's PEN needs.
4. Patient's Nutritional Prescription - Subsequent to an examination of the patient
and/or a review of the patient's medical information, the attending physician must
complete the patient's nutritional requirements (prescription) to certify the PEN
therapy provided.
For the parenteral patient, the CMN must contain the following information:
• The infusion frequency per week,
• The route of administration,
• A reason for the use of pre-mixed parenteral formulas,
• An explanation for the use of special formulas such as hepatic, renal, or stress
• formulas, and
• The amino acid/dextrose formula components of the parenteral solution mix.
Amino acids serve as a source of protein. Adult parenteral nutrition patients generally
need 1 to 1.5 grams of protein per day for each kilogram (2.2 pounds) of body weight.
Dextrose concentrations less than 10 percent must be explained by the physician. The
physician must document the reason for using more than 12 units (@ 500ml per unit) of
lipids per month.
Parenteral nutrition may be either "self-mixed" (i.e., the patient is taught to prepare the
nutrient solution aseptically) or "pre-mixed" (i.e., the nutrient solution is prepared by
trained professionals employed or contracted by the PEN supplier). The attending
physician must provide information to justify the reason for "pre-mixed" parenteral
nutrient solutions.
Renal dialysis patients sometimes undergo parenteral therapy to replace fluids and
nutrients lost during dialysis. Patients are usually infused less than daily and parenteral
feeding is often supplemental and, therefore, not covered as a PEN benefit. The renal
dialysis patient must meet all the requirements for PEN coverage. The attending
physician must document that the patient, despite the need for renal dialysis, suffers from
a permanently impaired functional impairment that precludes swallowing or absorption of
nutrients.
For the enteral patient, the attending physician must include the following information on
the CMN:
• The name of the nutrient product or nutrient category,
• The number of calories per day (100 calories = 1 unit),
• The frequency per day,
• The method of administration (i.e., syringe, gravity, or pump),
• The route of administration (i.e., nasogastric tube, gastrostomy tube, jejunostomy
tube, percutaneous enteral gastrostomy tube, or naso-intestinal tube), and
• The reason for the use of a pump.
Categories of enteral nutrition are based on the composition and source of ingredients in
each enteral nutrient product. Category IB of enteral nutrients contains products that are
natural intact protein/protein isolates commonly known as blenderized nutrients.
Additional documentation is required to justify the necessity of Category IB nutrients.
The attending physician must provide sufficient information to indicate that the patient:
• Has an intolerance to nutritionally equivalent (semi-synthetic) products;
• Had a severe allergic reaction to a nutritionally equivalent (semi-synthetic)
product; or
• Was changed to a blenderized nutrient to alleviate adverse symptoms expected to
be of permanent duration with continued use of semi-synthetic products.
Enteral nutrient categories III through VI require additional medical justification for
coverage. These categories represent formulas for special needs or use.
• Category III (code B4153): hydrolyzed protein/amino acids. These products
contain a high nitrogen availability as a result of chemical treatment to reduce
high molecular protein compounds into smaller molecules and amino acids that
are easier to digest.
• Category IV (code B4154): defined formulas for special metabolic needs and
conditions such as abnormal glucose tolerance, renal disease, liver disease, HIV,
respiratory insufficiency, and malnutrition.
• Category V (code B4155): modular components (proteins, carbohydrates, fats).
• Category VI (code B4156): standardized nutrients. These products contain low
residue ingredients.
If the patient exhibits a problem with any particular formula in Nutrient Category I
(HCPCS B4150) or II (HCPCS B4152), the physician must document the unfavorable
events that resulted in prescribing a higher category formula.
Generally, daily enteral intake of 750 to 2,000 calories is considered sufficient to
maintain body weight. Patients with medical complications may require an intake
outside the range. The attending physician must document the reason for prescribing less
than 750 calories per day or more than 2000 calories per day.
Enteral nutrition may be administered by syringe, gravity, or pump. The attending
physician must specify the reason that necessitates the use of an enteral feeding pump.
Some enteral patients may experience complications associated with syringe or gravity
method of administration. DME MACs provide coverage for enteral pumps if the
medical necessity is documented by the attending physician on the CMN. Examples of
circumstances that indicate the need for a pump include, but are not limited to:
• Aspiration or Dumping Syndrome;
• Severe diarrhea remedied by regulated feeding;
• Insulin-dependent diabetics who require a flow rate of less than 100cc's per hour
for proper regulation of nutrients;
• Patients with congestive heart failure who require a pump to prevent circulatory
overload; or
• Patients with a jejunostomy tube for feeding.
The DME MAC reviews the claims to ensure that the equipment for which payment is
claimed is consistent with that prescribed (e.g., expect a claim for an I.V. pole, if a pump
is used).
5. Attending Physician's Signature and Identification - A handwritten, original
signature and date must be on each certification. The form must be dated to show
reasonable association to the dates of active PEN therapy. The full name, address,
telephone number (including area code), and Unique Physician Identification
Number (UPIN) allows the DME MAC to determine if the prescriber is
authorized to order Medicare services and facilitate claims development.
6. PEN Supplier's Identification - The PEN supplier's name, address, telephone
number, and PEN identification number must be on each certification. This
information allows the DME MAC to determine if the supplier is authorized to
provide PEN supplies and facilitate claims development.
100.2.2.3 - DME MAC Review of Initial PEN Certifications
(Rev. 1, 10-01-03)
B3-4450
In reviewing the claim and the supporting data on the CMN, the DME MAC compares
certain items, especially pertinent dates of treatment. For example, the start date of PEN
coverage cannot precede the date of physician certification. The estimated duration of
therapy must be contained on the CMN. This information is used to verify that the test of
permanence is met. Once coverage is established, the estimated length of need at the
start of PEN services will determine the recertification schedule.
The information shown on the certification must support the need for PEN supplies as
billed. A diagnosis must show a functional impairment that precludes the enteral patient
from swallowing and the parenteral patient from absorbing nutrients.
Initial assigned claims with the following conditions are denied without development:
• Inappropriate or missing diagnosis or functional impairment;
• Estimated duration of therapy is less than 90 consecutive days;
• Duration of therapy is not listed;
• Supplies have not been provided;
• Supplies were provided prior to onset date of therapy; and
• Stamped physician's signature.
Unassigned claims are developed for missing or incomplete information.
A. Revised Certifications/Change in Prescription
A revised certification is required when:
• There is a change in the attending physician's orders in the category of nutrients
and/or calories prescribed;
• There is a change by more than one liter in the daily volume of parenteral
solutions;
• There is a change from home-mix to pre-mix or pre-mix to home-mix parenteral
solutions;
• There is a change from enteral to parenteral or parenteral to enteral therapy; or
• There is a change in the method of infusion (e.g., from gravity-fed to pump-fed).
The PEN payments are not adjusted unless a revised or renewed certification documents
the necessity for the change. Payment levels for the most current certification or
recertification may not be changed unless a prescription change is documented by a new
recertification.
The DME MAC may adjust the recertification schedule as needed.
100.2.3.1 - Scheduling and Documenting Recertifications of Medical
Necessity for Oxygen
(Rev. 1, 10-01-03)
Recertification scheduling and documentation requirements depend on the date when
home oxygen therapy began. DME MACs request the following information on all
recertifications:
• Date and results of the most recent arterial blood gas or oximetry tests prior to the
recertification date;
• Name of the provider conducting the most recent arterial blood gas or oximetry
tests performed prior to the recertification date and the conditions under which
this test were conducted; and
• Estimated length of need for oxygen (Section B on the Form CMS-484).
DME MAC establish the schedule for recertifying the need for oxygen for patients
beginning home oxygen therapy in accordance with the requirements below:

1. Recertifications
Group I: Recertification requirements are to be determined by the DME MAC.
Group II: If oxygen test results on the initial certification were in Group II, according to
§1834(a)(5) of the Act, recertification of all oxygen patients must be performed within 90
days after initial certification for all patients who begin coverage after January 1, 1991,
with an arterial blood gas result at or above a partial pressure of 55 mm Hg or an arterial
oxygen saturation percentage at or above 89. Repeat blood gas study must be performed
between the 61
st
- 90
th
day of home oxygen therapy. Retesting is required only if a claim
for oxygen therapy will be filed for the fourth or later months.
If recertification is due, DME MACs do not pay the next month's claim if the test was not
performed during the required time frame. If a qualifying test is not obtained between the
61st and 90th day of home oxygen therapy, but the patient continues to use oxygen and a
test is obtained at a later date, DME MAC instruct suppliers to use the date of the repeat
test as the date of service on a subsequent claim, and if that test meets Group II criteria,
they resume payments from that point of time.
2. New Orders - In the following situations, a new order must be obtained and kept
on file by the supplier, but neither a new CMN nor a repeat blood gas study are
required:
• If the prescribed maximum flow rate changes but remains within one of the
following categories: (a) less than 1 LPM, (b) 1-4 LPM, (c) greater than 4 LPM
• If the physician has initially specified a delivery system, and a change is made
from one type of stationary system to another (i.e., concentrator, liquid,
gaseous).
100.2.3.2 - HHA Recertification for Home Oxygen Therapy
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
Section 1834(a)(5) of the Act requires patients who receive home oxygen therapy and
who at the time such services are initiated have an initial arterial blood gas value of 56 or
higher or an initial oxygen saturation at or above 89 percent to be retested between 60
and 90 days after the start of oxygen therapy in order to continue to receive payment.
HHAs must initiate the request for the retesting as promptly as possible because the
recertification at three months must reflect the results of an arterial blood gas or oxygen
saturation test conducted between the 61st and 90th day of home oxygen therapy.
Payment for the fourth month of home oxygen therapy is possible only if the patient's
attending physician certifies that retesting results establish the continuing medical
necessity for the services. The physician must certify based on the test of the patient's
arterial blood gas value or oxygen saturation that there is a medical need for the patient to
continue to receive oxygen therapy.
Value codes have been assigned for HHA reporting of the arterial blood gas and oxygen
saturation. HHAs report value code 58 or 59 on every initial bill for home oxygen
therapy and on the fourth month's bill. Information regarding the form locator numbers
that correspond to value codes is found in Chapter 25.
For patients receiving oxygen therapy, who are not under a plan of care (bill type 34X),
HHAs obtain a physician’s recertification of the retesting and maintain a copy in their
files for verification.
For patients receiving oxygen therapy, who are under a plan of care (bill types 32X and
33X), HHAs obtain a physician's recertification of the retesting and reflect this on Form
CMS-485 or CMS-486 for verification.
A/B MACs (HHH) do not continue to make payment where the HHA fails to have the
patient retested to determine continuing need of oxygen therapy within the specified time
frames.
100.2.3.3 - A/B MAC (HHH) or DME MAC Review of Oxygen
Certifications
(Rev. 1, 10-01-03)
All claims with initial certifications calling for oxygen flow rates of more than 4 liters per
minute must be reviewed before payment is authorized.
Items Requiring Special Attention –
a. Oxygen Delivery or Supply Prescribed - If the treating physician has specified the
oxygen equipment to be supplied, A/B MACs (A) and (HHH) and DME MACs
ensure that the equipment furnished is consistent with that prescribed.
b. Treating Physician Identification - A/B MACs (A) and (HHH) and DME MACs
must ensure that the CMN or Form CMS-484 has been signed by the treating
physician. A stamped signature is unacceptable. The physician's identification
number must be the Unique Physician Identification Number (UPIN).
100.3 - Limitations on DME MAC Collection of Information
(Rev. 1, 10-01-03)
B-02-031
The Paperwork Reduction Act (PRA) of 1995 §44 USC 3500, et seq. requires that the
Director of the Office of Management and Budget approve any collections of information
performed by or for the Federal Government unless the collection fits within exceptions
for audits and investigations. Absent such approval, the collection violates the PRA and
agencies may not hold the public to the requirement. Therefore, DME MACs must
adhere to the following:
1. Power operated vehicles additional documentation requirements
A Certificate of Medical Necessity (CMN) must accompany initial claims for power
operated vehicles (POV). Except during the course of audits and investigations, DME
MACs must not require that additional documentation accompany all POV claims. DME
MACs may continue requesting information during the course of audits and
investigations and when developing individual claims on either a pre- or a post-payment
basis. If DME MACs choose to conduct such investigations, they must follow the
guidelines in the Program Integrity Manual, Chapter 3.
2. Power wheelchair additional documentation requirements re: make and model
name/number
There must be no requirement that all claims for power wheelchairs include the make and
model name/number of the wheelchair separate from the claim or the CMN.
The CMN, an OMB approved information collection form, can be used to collect this
information. Specifically, DME MACs can require that the make and model name/
number of the power wheelchair be included in Section C of the CMN. Section C
requires the supplier to include a narrative description of the items, options and
accessories ordered.
3. Power wheelchair additional documentation requirements re: functional abilities
There must be no requirement for suppliers to submit additional documentation to
describe a beneficiary's medical condition and functional abilities when the supplier bills
for a higher level of equipment than previously supplied.
While it is appropriate to avoid paying for duplicate equipment, it is inappropriate to
require this documentation for all claims for "higher level equipment." DME MACs may
choose to perform pre- or post- payment probe samples to review these types of claims
individually in order to determine medical necessity. If DME MACs choose to conduct
such investigations, they must follow the guidelines in the Program Integrity Manual,
Chapter 3.
100.4 - Reporting the Ordering/Referring NPI on Claims for DMEPOS
Items Dispensed Without a Physician’s Order
(Rev. 1368: Issued: 11-02-07; Effective: 05-23-08; Implementation: 04-07-08)
Chapter 5, section 5.2.1 of the Medicare Program Integrity Manual (PIM) states that, in
order for Medicare to make payment for an item of Durable Medical Equipment
Prosthetic, and Orthotic Supplies (DMEPOS), the DMEPOS supplier must obtain a
prescription from the
For Coordination of Benefit purposes, DMEPOS suppliers shall use the modifier EY (no
physician or other licensed health care provider order for this item or service) and report
their own name and National Provider Identifier (NPI) in the “Ordering/Referring
Provider Name” fields on claims submitted on or after May 23, 2008 to secure a
Medicare denial.
If the supplier has obtained a physician order for some, but not all, of the items provided
to a particular beneficiary, the supplier must submit a separate claim for the items with no
physician order.
110 - General Billing Requirements - for DME, Prosthetics, Orthotic
Devices, and Supplies
(Rev. 330, Issued: 10-22-04, Effective: 01-01-05, Implementation: 04-04-05)
Part B suppliers and providers other than Home Health Agencies (HHAs) must bill
DMEPOS to the DME MAC, except claims for implanted DME. Implanted DME and
supplies for the implanted equipment are billed to the A/B MAC (B).
Suppliers and providers must have a supplier billing number issued by the National
Supplier Clearinghouse (NSC) prior to billing the DME MAC.
Institutional providers bill their A/B MAC (A) for prosthetics and orthotics devices and
supplies. Generally, Medicare does not pay for DME in a facility. For hospital
outpatient DME, bills go to the appropriate DME MAC.
DMEPOS provided under a home health plan of care may be billed either by the HHA or
by the supplier (including the HHA with a supplier number if the HHA prefers to bill that
way) to the DME MAC. If the HHA chooses to bill to the A/B MAC (HHH), the HHA
includes the DME on the PPS claim (32x or 33x). If the beneficiary is not under a plan of
care and receives DMEPOS from a HHA, the agency uses bill type 34x.
Beneficiary Submitted Claims must contain an enrolled Medicare Supplier Number.
110.1 - Billing/Claim Formats
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
The DME MAC and the A/B MAC (B) are billed on the ASC X12 837 professional claim
format or if permissible Form CMS-1500.
The A/B MAC (A) (including the A/B MAC (HHH)) is billed on the ASC X12 837
institutional claim format or if permissible Form CMS-1450.
Note that the ASC X12 formats support reporting of the CMNs in the FRM segment

The National Council for Prescription Drug Programs (NCPDP) Telecommunications
Standard Version D0 and Batch Standard 1.2 is the HIPAA standard for electronic retail
pharmacy drug claims and related coordination of benefits (COB).
This standard will be used by all DME MACs that process retail pharmacy drug
transactions. All other claims submitted to the DME MAC by pharmacies, other than
retail pharmacy drug claims, must be sent in the ASC X12 837 professional claim format.
110.1.1 - Requirements for Implementing the NCPDP Standard
(Rev. 1, 10-01-03)
Retail pharmacies will be identified by a value of A5 in the specialty code as received by
the National Supplier Clearinghouse. Only DME MAC suppliers with an A5 specialty
code may use the NCPDP standard. The DME MACs, their EDI submitters, and their
other trading partners are required to transmit the NDCs in the NCPDP standards for
identification of prescription drugs dispensed through a retail pharmacy. NDCs replace
the drug HCPCS codes for retail pharmacy drug transactions billed to DME MACs via
the NCPDP standards.
110.1.2 - Certificate of Medical Necessity (CMN)
(Rev. 867, Issued: 02-17-06, Effective: 04-01-06, Implementation: 04-03-06)
The CMN for Parenteral Nutrition (Form CMS-852) is required. The DME MAC
Information Form for Immunosuppressive Drugs (Form DMERC-08.02) is not required
when billing for immunosuppressive drugs with dates of service on or after April 1, 2006.
As with other electronic formats, CMN data must be submitted within the valid
transaction.
For claims submitted on the Form CMS-1500, retail pharmacies will continue to supply
hard copy CMNs when required.
110.1.3 - NCPDP Companion Document
(Rev. 1, 10-01-03)
The DME MACs are to provide the NCPDP companion document, found at:
http://www.cms.gov/Medicare/Billing/ElectronicBillingEDITrans/Downloads/NCPDPD0
CG.pdf to retail pharmacy drug claim submitters (either provider, billing agent, or
clearinghouse) that will submit retail pharmacy drug claims to Medicare electronically.
110.2 - Application of DMEPOS Fee Schedule
(Rev. 1, 10-01-03)
Services that are paid under the DME fee schedule are identified in the DMEPOS fee
schedule file available free on the CMS Web Site at:
http://www.cms.gov/Medicare/Medicare-Fee-for-Service-
Payment/DMEPOSFeeSched/DMEPOS-Fee-Schedule.html

The DMEPOS fee schedule applies to claims to A/B MACs (A) and (HHH) as follows.
BILL TYPE/
DEFINITION
ORTHOTICS/
PROSTHETICS
DME/
OXYGEN
12X (Hospital inpatient
Part B)
Subject to fee schedule Not covered, therefore, not
subject to fee schedule
13X (Hospital Outpatient) Subject to fee schedule Subject to fee schedule
22X (SNF inpatient Part B) Subject to fee schedule Not covered, therefore, not
subject to fee schedule
23X (SNF outpatient) Subject to fee schedule Subject to fee schedule
*32X (HHA visits under
Part B Plan of Care)
Subject to fee schedule Subject to fee schedule
*33X (HHA visits under
Part A Plan of Care)
Subject to fee schedule Subject to fee schedule
34X (HHA visits not under
a Plan of Care)
Subject to fee schedule Subject to fee schedule
71X Rural health clinics
(Provider-based only)
Subject to fee schedule Subject to fee schedule
74X (Outpatient PT) Subject to fee schedule Subject to fee schedule
75X (CORF) Subject to fee schedule Subject to fee schedule
**83X ASC Subject to fee schedule Subject to fee schedule
85X RPCH Subject to fee schedule Subject to fee schedule
* HCPCS codes A4214, A4310 through A4455, A4481, A4622, A4623, A4625,
A4626, A4629, and A5051 through A5149 are excluded from the fee schedule when
billed by a HHA to its A/B MAC (HHH) under these bill types. Also, when billed
on type of bill 32x or 33, catheter and ostomy supplies are considered non-routine
supplies and are billed with revenue code 027x.
** HCPCS codes A4214, A4310 through A4330, A4338 through A4359, and A5102
through A5114 are excluded from the fee schedule when billed by a non-OPPS
hospital with an ASC service under this bill type. In addition, HCPCS codes A5119
through A5131 can be excluded or included in the fee schedule depending on the
procedure in which they are associated.
NOTE: Bill types not listed are not subject to the fee schedule for either orthotics/-
prosthetics or DME/oxygen with the exception of provider-based Federally Qualified
Health Centers (FQHCs). Orthotics/prosthetics and DME/oxygen furnished by provider-
based FQHCs are subject to the fee schedule. However, bill type 73X is not reflected in
the above chart since FQHCs use the bill type for the parent provider (usually 13x).
Bill types listed above are billed to the A/B MAC (A) or (HHH) for orthotics/prosthetics.
Providers other than HHAs bill the DME MAC for DME/oxygen. HHAs bill their A/B
MAC (HHH) for DME/oxygen.
DME billing is not required on Home Health PPS claims. Home Health Agencies retain
the option to bill services to A/B MAC (HHH) or have services provided under
arrangements with a supplier that bills the DME MAC.
110.3 - Pre-Discharge Delivery of DMEPOS for Fitting and Training
(Rev. 1, 10-01-03)
B3-3011
The following are CMS policy and billing procedures regarding the circumstances under
which a supplier may deliver durable medical equipment, prosthetics, and orthotics - but
not supplies - to a beneficiary who is in an inpatient facility that does not qualify as the
beneficiary's home.
110.3.1 - Conditions That Must Be Met
(Rev. 1, 10-01-03)
In some cases, it would be appropriate for a supplier to deliver a medically necessary
item of durable medical equipment (DME), a prosthetic, or an orthotic - but not supplies -
to a beneficiary who is an inpatient in a facility that does not qualify as the beneficiary's
home. The CMS will presume that the pre-discharge delivery of DME, a prosthetic, or an
orthotic (hereafter "item") is appropriate when all the following conditions are met:
1. The item is medically necessary for use by the beneficiary in the beneficiary's home.
2. The item is medically necessary on the date of discharge, i.e., there is a physician's
order with a stated initial date of need that is no later than the date of discharge for home
use.
3. The supplier delivers the item to the beneficiary in the facility solely for the purpose of
fitting the beneficiary for the item, or training the beneficiary in the use of the item, and
the item is for subsequent use in the beneficiary's home.
4. The supplier delivers the item to the beneficiary no earlier than two days before the
day the facility discharges the beneficiary.
5. The supplier ensures that the beneficiary takes the item home, or the supplier picks up
the item at the facility and delivers it to the beneficiary's home on the date of discharge.
6. The reason the supplier furnishes the item is not for the purpose of eliminating the
facility's responsibility to provide an item that is medically necessary for the beneficiary's
use or treatment while the beneficiary is in the facility. Such items are included in the
Diagnostic Related Group (DRG) or Prospective Payment System (PPS) rates.
7. The supplier does not claim payment for the item for any day prior to the date of
discharge.
8. The supplier does not claim payment for additional costs that the supplier incurs in
ensuring that the item is delivered to the beneficiary's home on the date of discharge. The
supplier cannot bill the beneficiary for redelivery.
9. The beneficiary's discharge must be to a qualified place of service (e.g., home,
custodial facility), but not to another facility (e.g., inpatient or skilled nursing) that does
not qualify as the beneficiary's home.
110.3.2 - Date of Service for Pre-Discharge Delivery of DMEPOS
(Rev. 1, 10-01-03)
For DMEPOS, the general rule is that the date of service is equal to the date of delivery.
However pre-discharge delivery of items intended for use upon discharge are considered
provided on the date of discharge. The following three scenarios demonstrate both the
latter rule (when the date of service is the date of discharge) and related exceptions.
1. If the supplier leaves the item with the beneficiary two days prior to the date of
discharge, and if the supplier, as a practical matter, need do nothing further to effect the
delivery of the item to the beneficiary's home (because the beneficiary or a caregiver
takes it home), then the date of discharge is deemed to be the date of delivery of the item.
Such date must be the date of service for purposes of claims submission. (This is not an
exception to the general DMEPOS rule that the date of service must be the date of
delivery. Rather, it recognizes the supplier's responsibility - per condition five above - to
ensure that the item is actually delivered to the beneficiary's home on the date of
discharge.) No one may bill for the days prior to the date of discharge.
2. If the supplier fits the item to the beneficiary, or trains the beneficiary in its use while
the beneficiary is in the facility, but thereafter removes the item and subsequently
delivers it to the beneficiary's home, then the date of service must be the date of actual
delivery of the item, provided such date is not earlier than the date of discharge.
3. If the supplier leaves the item at the facility and the beneficiary does not take the item
home, or a third party does not send it to the beneficiary's home, or the supplier does not
otherwise (re)deliver the item to the beneficiary's home on or before the date of
discharge, the date of service must not be earlier than the actual date of delivery of the
item, i.e., the actual date the item arrives, by whatever means, at the beneficiary's home.
110.3.3 - Facility Responsibilities During the Transition Period
(Rev. 1, 10-01-03)
1. A facility remains responsible for furnishing medically necessary items to a
beneficiary for the full duration of a beneficiary's stay. The DRG and PPS rates cover
such items.
2. A facility may not delay furnishing a medically necessary item for the beneficiary's use
or treatment while the beneficiary is in the facility. A facility may not prematurely
remove a medically necessary item from the beneficiary's use or treatment on the basis
that a supplier delivered a similar or identical item to the beneficiary for the purpose of
fitting or training.
3. A facility may not, through a stratagem of relying upon a supplier to furnish such
items, improperly shift its costs for furnishing medically necessary items to a beneficiary
who is a resident in the facility to Medicare Part B.
Nevertheless, beginning two days before the beneficiary's discharge, a facility may take
reasonable actions to permit a supplier to fit or train the beneficiary with the medically
necessary item that is for subsequent use in the beneficiary's home. These actions may
include the substitution of the supplier-furnished item, in whole or in part, for the facility-
furnished item during the beneficiary's last two inpatient days provided the substitution is
both reasonable and necessary for fitting or training and the item is intended for
subsequent use at the beneficiary's home.
4. For prosthetic and orthotic (P&O) items, the above restrictions apply to residents in a
covered Part A stay. For DME, the above restrictions apply in a covered Part A or a Part
B stay.
110.4 - Frequency of Claims for Repetitive Services (All Providers and
Suppliers)
(Rev. 1, 10-01-03)
HHAs include DMEPOS on bill types 32x or33x with home health visits bill at the
freqency required for the home health. See Chapter 10 for home health billing
requirements.
Other providers and suppliers, including home health agencies billing the A/B MAC
(HHH) on bill type 34x, submit claims on a monthly basis unless another policy that
allows billing at a different frequency applies. For example suppliers may bill for more
than one month's diabetic test strips.
Claims are submitted in sequence where there are cases of known continuous periods of
service over an extended period (e.g., capped rental equipment or therapies). When there
is a break in service (e.g. interruption of capped rental as the result of an extensive
inpatient stay), suppliers should continue sequential billing when the services resume.
The purpose of these requirements is to avoid CMS operational expenditures, and at the
same time simplify the review process
110.5 - DME MACs Only - Appeals of Duplicate Claims
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
The Durable Medical Equipment Medicare Administrative Contractors (DME MACs)
must afford appeal rights for the initial determination of an item or service only, unless
the supplier is appealing whether or not the denied item is actually a duplicate. If a claim
is denied as a duplicate, the DME MACs must not afford appeal rights based on
coverage, medical necessity, pricing, or any basis on which the supplier can otherwise
appeal. The DME MAC may only afford appeal rights on claims denied as duplicates if
the supplier is appealing because the claim is not, in fact, a duplicate. If a supplier
appeals a denied duplicate claim on the basis that the claim is not, in fact a duplicate, the
DME MAC shall adjudicate the claim in accordance with all other Medicare rules and
regulations.
The DME MACs must use the following Medicare Summary Notice (MSN) and ASC
X12 835 remittance messages when denying duplicate claims:
• MSN 7.3 - This service/item is a duplicate of a previously processed service. No
appeal rights are attached to the denial of this service except for the issue as to
whether the service is a duplicate. Disregard the appeals information on this
notice unless you are appealing whether the service is a duplicate.
• Spanish - Este servicio/artículo es un duplicado de otro servicio procesado
previamente. No tiene derechos de apelación de este servicio, excepto si
cuestiona que este servicio es un duplicado. Haga casa omiso a la información
sobre apelaciones en esta notification, en relación a sus derechos de apelación, a
menos que este apelando si el servicio fue duplicado.
• Claim adjustment reason code 18:- Duplicate claim/service
Remittance advice remark code N111 - This service was included in a claim that was
previously billed and adjudicated. No appeal rights attached except with regard to
whether the service/item is a duplicate.

120 - DME MACs - Billing Procedures Related To Advanced
Beneficiary Notice (ABN) Upgrades
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
This section provides the DME MACs billing instructions regarding the use of ABNs and
claims modifiers for upgrades for items of DMEPOS.
Federal Regulations at 42 CFR 411.408 and Chapter 30 of this manual establishes the
basis for a supplier to issue an ABN to a beneficiary. The purpose of the ABN is to
inform a Medicare beneficiary, before he or she receives an item that Medicare will
probably not pay for that particular item on that particular occasion. The ABN allows the
beneficiary to make an informed consumer decision on whether to accept an item for
which he or she may have to pay out of pocket or through supplementary insurance.
Under existing policy, suppliers may collect from a beneficiary a payment amount greater
than Medicare’s allowed payment amount if the beneficiary, by signing an ABN, agrees
to pay extra for a DMEPOS item because the beneficiary prefers an item with features or
upgrades that are not medically necessary. This policy applies to both assigned and
unassigned claims. When a beneficiary does not sign an ABN, a supplier that accepts
assignment cannot hold the beneficiary liable for the cost of medically unnecessary
equipment or upgrades unless there is other acceptable evidence that the beneficiary
knew or could reasonably have been expected to know that Medicare would not pay for
the medically unnecessary equipment or upgrades. With respect to unassigned claims, a
signed ABN is necessary to hold the beneficiary liable.
The instructions in this section apply to situations where the ABN is being used for
upgrades and applies to both assigned and unassigned claims. An upgrade is an item with
features that go beyond what is medically necessary. An upgrade may include an excess
component. An excess component may be an item feature or service, which is in addition
to, or is more extensive and/or more expensive than the item that is reasonable and
necessary under Medicare’s coverage requirements. When a DMEPOS supplier knows
or believes that the DMEPOS item does or may not meet Medicare’s reasonable and
necessary rules under specific circumstances, it is the responsibility of the supplier to
notify the beneficiary in writing via an ABN if the supplier wants to collect money from a
beneficiary if an item is denied.
When a supplier furnishes an upgraded item of DMEPOS and the supplier expects
Medicare to reduce the level of payment based on a medical necessity partial denial of
coverage for additional expenses attributable to the upgrade, the supplier must give an
ABN to the beneficiary for signature for holding the beneficiary liable for the additional
expense. Optional ABN forms are available at:
http://www.cms.gov/Medicare/Medicare-General-Information/BNI/ABN.html.
A. General Instructions for the Use of ABNs for Upgrading DMEPOS Items
Instruction Description
1.
An upgrade may be from one item to another within a single Heath
Insurance Common Procedure Coding System (HCPCS) code, or may be
from one HCPCS code to another. When an upgrade is within a single
code the upgraded item must include features that exceed the official code
descriptor for that item.
2.
The upgrade must be within the range of items or services that are
medically appropriate for the beneficiary’s medical condition and the
purpose of the physician’s order. ABNs may not be used to substitute a
different item or service that is not medically appropriate for the
beneficiary’s medical condition for the original item or service. The
upgraded item must still meet the intended medical purpose of the item
the physician ordered.
3.
Use of an ABN to furnish an upgraded item or service, with the
beneficiary being personally responsible for the difference between the
costs of the standard and upgraded item or service, does not change
coverage or payment rules, statutory provisions, or manual instructions for
the particular benefit involved.
4.
In cases where the DME MACs would make payment for the item the
physician ordered on a rental basis, the supplier must furnish the upgrade
on a rental basis.
5.
A supplier furnishing an upgrade and using an ABN must submit a claim
and include information on the claim that identifies the upgrade features.
Suppliers must submit a claim for upgraded items and services using the
GA modifier on the upgraded line item to indicate that the beneficiary
signed an ABN. Suppliers must list upgrade features using the ASC X12
837 professional claim format or on the paper Form CMS-1500 in Item 19
or as an attachment to the claim for paper claims.
6.
Denials should be based on medical necessity.
B. Billing Instructions:
Suppliers must bill 2 line items for upgraded DMEPOS items where the beneficiary
requests an upgrade. Suppliers must bill both lines on the same claim in the following
order:
Line
Instruction
Line 1:
Bill the appropriate HCPCS code for the upgraded item the supplier actually
provided to the beneficiary with the dollar amount of the upgraded item. If
the supplier has a properly obtained ABN on file signed by the beneficiary,
use the GA modifier. If the supplier did not properly obtain an ABN signed
by the beneficiary, use the GZ modifier.
Line 2:
Bill the appropriate HCPCS code for the reasonable and necessary item with
the actual charge for the item. Use the GK modifier.
Suppliers should bill their full submitted charge on the claim line for the upgraded item
(Line 1) and the full amount for the reasonable and necessary item (Line 2). If the
upgrade is within a code, suppliers still bill 2 line items, using the same code on both
lines, but Line 1 would have the higher dollar amount.
Suppliers must bill both lines on the same claim in sequential order. Line 1 and the
associated Line 2 should follow each other.
DME MACs must return/reject applicable assigned claims that have invalid ABN
upgrade information using appropriate messages. If the claim is unassigned, DME
MACs must issue a denial.
C. Definitions of Modifiers that May be Associated with ABNs
Modifier Description
GA -
Waiver of Liability (expected to be denied as not reasonable and necessary,
ABN on file)
GZ -
Item or Service not Reasonable and Necessary (expected to be denied as not
reasonable and necessary, no ABN on file)
GK -
Reasonable and necessary item/service associated with GA or GZ modifier
D. Medicare Summary Notice (MSN) and Remittance Advice (RA)
MSN Detailed text
36.01:
Our records show that you were informed in writing, before receiving
the service that Medicare would not pay. You are liable for this charge.
If you do not agree with this statement, you may ask for a review. ASC
X12 835, remittance advice remark code M38
36.02:
It appears that you did not know that we would not pay for this service
so you are not liable. Do not pay your provider for this service. If you
have paid your provider for this service, you should submit to this
office three things 1) A copy of this notice, 2) Your provider’s bill, and
3) A receipt or proof that you have paid the bill. You must file your
written request for payment within 6 months of the date of this notice.
Future services of this type provided to you will be your responsibility.
ASC X12 835 remittance advice remark code M25)
8.51:
You signed an Advanced Beneficiary Notice (ABN). You are
responsible for the difference between the upgrade amount and the
Medicare payment.
Use the following messages when denying claims due to invalid ABN upgrade
information:
MSN Detailed text
8.53:
This item or service was denied because the upgrade information was
invalid.
N108:
This item/service was denied because the upgrade information was
invalid.
120.1 - Providing Upgrades of DMEPOS Without Any Extra Charge
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
Instead of using ABNs and charging beneficiaries for upgraded items, suppliers in certain
circumstances may decide to furnish beneficiaries with upgraded equipment but charge
the Medicare program and the beneficiary the same price they would charge for a non-
upgraded item. The reason for this may be that a supplier prefers to carry only higher
level models of medical equipment in order to reduce the costs of maintaining an
inventory that includes a wide variety of different models and products. Also, a supplier
may be able to reduce its costs for replacement parts and repairs if it includes in its
inventory only certain product lines. The supplier may also be accommodating a
physician order for an upgrade.
Policy
Suppliers are permitted to furnish upgraded DMEPOS items and to charge the same price
to Medicare and the beneficiary that they would charge for a non-upgraded item. This
policy allows suppliers to furnish to beneficiaries, at no extra costs to the Medicare
program or the beneficiary, a DMEPOS item that exceeds what the non-upgraded item
that Medicare considers to be medically necessary. Therefore, even though the
beneficiary received an upgraded DMEPOS item, Medicare’s payment and the
beneficiary’s coinsurance would be based on the Medicare allowed amount for a non-
upgraded item that does not include features that exceed the beneficiary’s medical needs.
Billing Instructions
When a supplier decides to furnish an upgraded DMEPOS item but to charge Medicare
and the beneficiary for the non-upgraded item, the supplier must bill for the non-
upgraded item rather than the item the supplier actually furnished. The claim must
include only the charge and HCPCS code for the non-upgraded item. The HCPCS code
for the non-upgraded item must be accompanied by the following modifier:
Modifier Detailed Text
GL
Medically Unnecessary Upgrade Provided Instead of Non-upgraded Item,
No Charge, No ABN

Suppliers must show the upgrade using the ASC X12 837 professional claim format, or in
Item 19 of a paper Form CMS-1500 claim, or as an attachment. The supplier must
specify the make and model of the item actually furnished, that is, the upgraded item, and
describe why this item is an upgrade
DME MACs are to pay based on Medicare’s payment amount for the non-upgraded item
if it meets Medicare’s coverage and payment requirements. A certificate of medical
necessity, if applicable, must be completed for the HCPCS code that identifies the non-
upgraded item but not for the upgraded item.
MSN Message:
For items accompanied with a GL modifier, use:
MSN Detailed Text
8.51:
You are not liable for any additional charge as a result of receiving an
upgraded item.
130 - Billing for Durable Medical Equipment (DME) and Orthotic/
Prosthetic Devices
(Rev. 2629, Issued: 01-04-13, Effective: -02-05-13, Implementation: 02-05-13)
See §01 of this chapter for definition of provider and supplier.
130.1 - Provider Billing for Prosthetic and Orthotic Devices
(Rev. 2629, Issued: 01-04-13, Effective: -02-05-13, Implementation: 02-05-13)
See § 01 of this chapter for definition of provider.
These items consist of all prosthetic and orthotic devices excluding parenteral/enteral
nutritional supplies and equipment and intraocular lenses.
Prosthetics and orthotic devices when provided during inpatient care are included in the
Part A PPS rate unless specified as being outside the rate. The link for information on
services included and excluded from the SNF PPS is
http://www.cms.gov/Medicare/Billing/SNFConsolidatedBilling/index.html
. The DME
MAC will not separately pay for items of DME provided to a beneficiary in a SNF.
Prosthetics, orthotics and supplies that are considered outside the PPS rate may be billed
by the supplier in the case of a SNF or hospital to the A/B MAC (A), or if furnished by a
qualified outside entity, that entity may bill its normal contractor.
The SNFs, hospitals, or other entities that furnish prosthetic and/or orthotic devices to
their patients for whom Part A benefits are not payable (i.e., no Part A entitlement or
benefits exhausted) may bill for such items, assuming other billing requirements are met.
NOTE: Items such as catheters and ostomy supplies are excluded from the fee schedule
when billed by HHAs for patients under a plan of care. In this situation, HHAs
bill for these items as supplies under revenue code 0270. Effective with items
furnished on or after January 1, 1994, the fee schedules for ostomy,
tracheostomy, and urological supplies are calculated using the same method
used to calculate the purchase fee schedules for inexpensive or other routinely
purchased DME.
HCPCS codes A4214, A4310 through A4330, A4338 through A4359, and A5102
through A5114 are excluded from the fee schedule when billed by hospitals along with an
ASC service. Hospitals bill for these items as supplies, under revenue code 0272. In
addition, HCPCS codes A5119 through A5131 are excluded from the fee schedule unless
they are submitted with ostomy related ASC procedure codes 44340 through 44346,
44380, 44382, 44388 through 44392, or 50953 through 50961.
In all other circumstances, including HHAs billing for patients not under a plan of care,
SNFs, CORFs, OPTs, and hospitals bill these items as prosthetics and orthotics under
code 0274, along with the relevant HCPCS code.
DME MACs only - For all states that have licensure/certification requirements for
provision of prosthetics and/or orthotics, DME MACs shall process claims for Prosthetics
and Certain Custom-Fabricated Orthotics only when the following specialty codes are
forwarded to the DME MACs from the NSC. The specialty codes are:
• Medical Supply Company with Orthotics Personnel - Specialty Code 51;
• Medical Supply Company with Prosthetics Personnel - Specialty Code 52;
• Medical Supply Company with Orthotics and Prosthetics Personnel - Specialty
Code 53;
• Orthotics Personnel - Specialty Code 55;
• Prosthetics Personnel - Specialty Code 56;
• Orthotics Personnel, Prosthetics Personnel and Pedorthists - Specialty Code 57,
• Physical Therapist - Specialty Code 65;
• Occupational Therapist - Specialty Code 67;
• Ocularist - Specialty Code B5; and
• All Physician Specialty Codes listed in this manual [IOM] Chapter 26, §10.8.2
These specialties shall be licensed or certified by the state when applicable. These
specialties shall bill for Medicare services when State law permits such entity to furnish a
prosthetic or orthotic.
Claims billed by other specialty codes for prosthetics and certain custom-fabricated
orthotics shall be denied.
130.2 - Billing for Inexpensive or Other Routinely Purchased DME
(Rev.4027; Issued: 04-27-18; Effective: 10-01-18; Implementation: 10-01-18)
This is equipment with a purchase price not exceeding $150, or equipment that
the Secretary determines is acquired by purchase at least 75 percent of the time, or
equipment that is an accessory used in conjunction with a nebulizer, aspirator, or
ventilators that are either continuous airway pressure devices or intermittent assist
devices with continuous airway pressure devices. Effective October 1, 2015, this
category also includes speech generating devices and accessories necessary for
the effective use of speech generating devices. Suppliers and providers other than
HHAs bill the DME MAC or, in the case of implanted DME only, the A/B MAC
(B). HHAs bill the A/B MAC (HHH) or the DME MAC.
Effective for items and services furnished after January 1, 1991, Medicare DME
does not include seat lift chairs. Only the seat lift mechanism is defined under
Medicare as DME. Therefore, seat lift coverage is limited to the seat lift
mechanism. If a seat lift chair is provided to a beneficiary, A/B MACs (A), and
(HHH), and DME MACs pay only for the lift mechanism portion of the chair.
Some lift mechanisms are equipped with a seat that is considered an integral part
of the lift mechanism. A/B MACs (A) and (HHH), and DME MACs do not pay
for chairs (HCPCS code E0620) furnished on or after January 1, 1991. The
appropriate HCPCS codes for seat lift mechanisms are E0627, E0628, and E0629.
For TENS, suppliers and providers other than HHAs bill the DME MAC. HHAs
bill the A/B MAC (HHH) using revenue code 0291 for the 2-month rental
period (see §30.1.2), billing each month as a separate line item and revenue code
0292 for the actual purchase along with the appropriate HCPCS code.
130.3 - Billing for Items Requiring Frequent and Substantial Servicing
(Rev. 1, 10-01-03)
A3-3629, B3-4107.8
These are items such as intermittent positive pressure breathing (IPPB) machines and
ventilators, excluding ventilators that are either continuous airway pressure devices or
intermittent assist devices with continuous airway pressure devices.

Suppliers and providers other than HHAs bill the DME MAC. HHAs bill the A/B MAC
(HHH).
130.4 - Billing for Certain Customized Items
(Rev. 1, 10-01-03)
A3-3629, B3-4107.8
Due to their unique nature (custom fabrication, etc.), certain customized DME cannot be
grouped together for profiling purposes. Claims for customized items that do not have
specific HCPCS codes are coded as E1399 (miscellaneous DME). This includes
circumstances where an item that has a HCPCS code is modified to the extent that neither
the original terminology nor the terminology of another HCPCS code accurately
describes the modified item.
Suppliers and providers other than HHAs bill the A/B MAC (B) or DME MAC. HHAs
bill their A/B MAC (HHH), using revenue code 0292 along with the HCPCS.
130.5 - Billing for Capped Rental Items (Other Items of DME)
(Rev. 1, 10-01-03)
A3-3629, B3-4107.8
These are DME items, other than oxygen and oxygen equipment, not covered by the
above categories. Suppliers and providers other than HHAs bill the DME MAC. HHAs
bill the A/B MACs (HHH).
130.6 - Billing for Oxygen and Oxygen Equipment
(Rev. 3895, Issued: 10-27-17, Effective: 04-01-18, Implementation: 04- 02-18)
The following instructions apply to all claims from providers and suppliers to whom
payment may be made for oxygen. The chart in §130.6.1 indicates what is payable under
which situation.
A. Monthly Billing
Fee schedule payments for stationary oxygen system rentals are all inclusive and
represent a monthly allowance per beneficiary. Accordingly, a supplier must bill on a
monthly basis for stationary oxygen equipment and contents furnished during a rental
month.
A portable equipment add-on is also payable when portable oxygen is prescribed and it is
determined to be medically necessary in accordance with Medicare coverage
requirements. The portable add-on must be claimed in order to be paid. (See §30.6.)
B. HCPCS Codes

The HCPCS codes must be used to report the service. One month of service equals one
unit.
C. Use of Payment Modifiers and Revenue Codes for Payment Adjustments
The monthly payment amount for stationary oxygen is subject to adjustment depending
on the amount of oxygen prescribed (liters per minute (LPM)), and whether or not
portable oxygen is also prescribed. (See §30.6.) HHAs billing the A/B MAC (HHH) for
stationary equipment, supplies, or contents, which are not eligible for payment
adjustment, bill under revenue code 0601. Claims must indicate the appropriate HCPCS
modifier described below, if applicable.
• If the prescribed amount of oxygen is less than 1 LPM, suppliers use the
modifier "QE"; HHAs use revenue code 0602. The monthly payment amount
for stationary oxygen is reduced by 50 percent.
• If the prescribed amount of oxygen is greater than 4 LPM, suppliers use the
modifier "QG"; HHAs use revenue code 0603. The monthly payment amount
for stationary oxygen is increased by 50 percent.
• If the prescribed amount of oxygen exceeds 4 LPM and portable oxygen is
prescribed, suppliers use the modifier "QF"; HHAs use revenue code 0604. The
monthly payment for stationary oxygen is increased by the higher of 50 percent
of the monthly stationary oxygen payment amount, or, the fee schedule amount
for the portable oxygen add-on. (A separate monthly payment is not allowed
for the portable equipment.) Effective April 1, 2017, the modifier “QF” must be
used with both the stationary and portable oxygen equipment codes.
Effective April 1, 2017, portable oxygen “QF” modifier fee schedule amounts will be
added to the DMEPOS fee schedule file. The portable oxygen “QF” fee schedule
amounts will represent the higher of 1) 50 percent of the monthly stationary oxygen
payment amount or 2) the fee schedule amount for the portable oxygen add-on.
There are three claims processing scenarios:
Scenario 1 – A claim for stationary oxygen equipment is submitted with the QG modifier.
The history is reviewed and it is discovered that portable oxygen equipment was billed
AND paid within the last 30 days prior to the stationary oxygen equipment’s date of
service. Since we have already paid the portable add-on, we can’t pay the volume
adjustment add-on, therefore billing with QG modifier is inappropriate and the claim
should be returned as unprocessable.
Scenario 2 – A claim for stationary oxygen equipment is submitted with the QG modifier
and within 30 days, a claim for portable oxygen equipment is received. In this case we
have already paid the volume add-on so the portable equipment add –on is returned as
unprocessable.
Scenario 3 – A claim for stationary oxygen equipment is submitted with the QG modifier
AND the portable oxygen equipment comes in with the same date of service. In this case
EVERYTHING is returned as unprocessable due to the incorrect use of the modifier and
neither is valid.
NOTE: All these claims are being returned as unprocessable since there is no way for
Medicare to know whether the first claim submitted was billed incorrectly or if the
subsequent claim was billed incorrectly.
Contractors shall use the following messages for claims that are returned as
unprocessable:
Group Code: CO (Contractual Obligation)
CARC 4 - The procedure code is inconsistent with the modifier used or a required
modifier is missing. Note: Refer to the 835 Healthcare Policy Identification Segment
(loop 2110 Service Payment Information REF), if present.
RARC MA130 - Your claim contains incomplete and/or invalid information, and no
appeal rights are afforded because the claim is unprocessable. Please submit a new claim
with the complete/correct information.
The following three new pricing modifiers are added to the HCPCS file effective April 1,
2018:
QA PRESCRIBED AMOUNTS OF STATIONARY OXYGEN FOR DAYTIME
USE WHILE AT REST AND NIGHTTIME USE DIFFER AND THE
AVERAGE OF THE TWO AMOUNTS IS LESS THAN 1 LITER PER
MINUTE (LPM)
QB PRESCRIBED AMOUNTS OF STATIONARY OXYGEN FOR DAYTIME
USE WHILE AT REST AND NIGHTTIME USE DIFFER AND THE
AVERAGE OF THE TWO AMOUNTS EXCEEDS 4 LITERS PER MINUTE
(LPM) AND PORTABLE OXYGEN IS PRESCRIBED
QR PRESCRIBED AMOUNTS OF STATIONARY OXYGEN FOR DAYTIME
USE WHILE AT REST AND NIGHTTIME USE DIFFER AND THE
AVERAGE OF THE TWO AMOUNTS IS GREATER THAN 4 LITERS PER
MINUTE (LPM)
Additionally, the existing QE, QF, and QG modifiers are revised to clarify that the
prescribed flow rate at rest is used in accordance with regulations at 42 CFR
414.226(e)(3). This section instructs that if the prescribed flow rate is different for the
patient at rest than for the patient at exercise, the flow rate for the patient at rest is used.
Effective April 1, 2018, the modifiers are revised to read:
QE PRESCRIBED AMOUNT OF STATIONARY OXYGEN WHILE AT REST
IS LESS THAN 1 LITER PER MINUTE (LPM)
QF PRESCRIBED AMOUNT OF STATIONARY OXYGEN WHILE AT REST
EXCEEDS 4 LITERS PER MINUTE (LPM) AND PORTABLE OXYGEN IS
PRESCRIBED
QG PRESCRIBED AMOUNT OF STATIONARY OXYGEN WHILE AT REST
IS GREATER THAN 4 LITERS PER MINUTE (LPM)
Beginning April 1, 2018, claims for monthly oxygen volume adjustments must indicate
the appropriate HCPCS modifier described below as applicable. Oxygen fee schedule
amounts are adjusted as follows:
If the prescribed amount of oxygen is less than 1 LPM, suppliers use either of the
following modifiers with the stationary oxygen HCPCS code:
• The modifier “QE” PRESCRIBED AMOUNT OF STATIONARY OXYGEN
WHILE AT REST IS LESS THAN 1 LITER PER MINUTE (LPM); HHAs use
revenue code 0602. The monthly payment amount for stationary oxygen is
reduced by 50 percent.
• The modifier “QA” PRESCRIBED AMOUNTS OF STATIONARY OXYGEN
FOR DAYTIME USE WHILE AT REST AND NIGHTIME USE DIFFER AND
THE AVERAGE OF THE TWO AMOUNTS IS LESS THAN 1 LITER PER
MINUTE (LPM); The monthly payment amount for stationary oxygen is reduced
by 50 percent. This modifier is used when the prescribed flow rate is different for
nighttime use and daytime use and the average of the two flow rates is used in
determining the volume adjustment.
If the prescribed amount of oxygen is greater than 4 LPM, suppliers use either of the
following modifiers with the stationary oxygen HCPCS code:
• The modifier “QG” PRESCRIBED AMOUNT OF STATIONARY OXYGEN
WHILE AT REST IS GREATER THAN 4 LITERS PER MINUTE (LPM);
HHAs use revenue code 0603. The monthly payment amount for stationary
oxygen is increased by 50 percent.
• The modifier “QR” PRESCRIBED AMOUNTS OF STATIONARY OXYGEN
FOR DAYTIME USE WHILE AT REST AND NIGHTIME USE DIFFER AND
THE AVERAGE OF THE TWO AMOUNTS IS GREATER THAN 4 LITERS
PER MINUTE (LPM); HHAs use revenue code 0603. The monthly payment
amount for stationary oxygen is increased by 50 percent.
If the prescribed amount of oxygen is greater than 4 LPM and portable oxygen is
prescribed, suppliers use either of the following modifiers with both the stationary and
portable oxygen HCPCS code:
• The modifier “QF” PRESCRIBED AMOUNT OF STATIONAY OXYGEN
WHILE AT REST EXCEEDS 4 LITERS PER MINUTE (LPM) AND
PORTABLE OXYGEN IS PRESCRIBED; HHAs use revenue code 0604. If the
prescribed flow rate differs between stationary and portable oxygen equipment,
the flow rate for the stationary equipment is used. The monthly payment for
stationary oxygen is increased by the higher of 50 percent of the monthly
stationary oxygen payment amount, or the fee schedule amount for the portable
oxygen add-on. A separate monthly payment is not allowed for the portable
equipment. Effective April 1, 2017, the modifier “QF” must be used with both the
stationary and portable oxygen equipment codes.
• The modifier “QB” PRESCRIBED AMOUNTS OF STATIONARY OXYGEN
FOR DAYTIME USE WHILE AT REST AND NIGHTTIME USE DIFFER
AND THE AVERAGE OF THE TWO AMOUNTS EXCEEDS 4 LITERS PER
MINUTE (LPM) AND PORTABLE OXYGEN IS PRESCRIBED; HHAs use
revenue code 0604. If the prescribed flow rate differs between stationary and
portable oxygen equipment, the flow rate for the stationary equipment is used.
The monthly payment for stationary oxygen is increased by the higher of 50
percent of the monthly stationary payment amount, or the fee schedule amount for
the portable oxygen add-on. A separate monthly payment is not allowed for the
portable equipment. Effective April 1, 2018, the modifier “Q??” must be used
with both the stationary and portable oxygen equipment codes. The stationary and
portable oxygen equipment QB fee schedule amounts will be added to the
DMEPOS fee schedule file effective 4/1/2018.
The stationary oxygen QF and QB fee schedule amounts on the DMEPOS fee schedule
file represent 100 percent of the stationary oxygen allowed fee schedule amount. The
portable oxygen equipment add-on QF and QB fee schedule amount on the file by state
represent the higher of:

1. 50 percent of the monthly stationary oxygen payment amount (codes E0424,
E0439, E1390 or E1391); or
2. The fee schedule amount for the portable oxygen add-on (codes E0431, E0433,
E0434, E1392 or K0738).
D. Conserving Device Modifier
The HHA's and suppliers must indicate if an oxygen conserving device is being used with
an oxygen delivery system by using HCPCS modifier “QH”.
E. DME MACs Only
For all States that have licensure/certification requirements for the provision of oxygen
and/or oxygen related products, DME MACs shall process claims for oxygen and oxygen
related products only when an oxygen specialty code is assigned to the DMEPOS
supplier by the NSC and is forwarded to the DME MACs from the NSC.
This specialty shall be licensed and/or certified by the State when applicable. This
specialty shall bill for Medicare-covered services and/or products when State law permits
such entity to furnish oxygen and/or oxygen related products.
130.6.1 - Oxygen Equipment and Contents Billing Chart
(Rev. 1, 10-01-03)
The following chart indicates what oxygen fee schedule component is billable/payable
under various transaction scenarios for providers and suppliers:
1. Situation: Beneficiary Uses a Stationary System Only
a. Rental Cases (Beneficiary Uses a Stationary System Only)
Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Concentrator Yes No No No

Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
E1377
E1378
E1379
E1380
E1381
E1382
E1383
E1384
E1385
E1400
E1401
E1402
E1403
E1404
E1405
E1406

Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Gaseous Yes No No No
E0424
Liquid Yes No No No
E0439
b. Purchase Cases (Beneficiary Uses a Stationary System Only)
Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Concentrator No No No No
Gaseous No Yes No No
E0441
Liquid No Yes No No
E0442
2. Situation: Beneficiary Uses Both a Stationary and Portable System

a. Rents Stationary/Rents Portable
Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Concentrator Yes No Yes No
E1377
E1378
E1379
E1380
E1381
E1382
E1383
E1384
E1385
E1400
E1401
E1402
E1403
E1404
E1405
E1406
E0431
E0434
Gaseous Yes No Yes No
E0424 E0431
Liquid Yes No Yes No
E0439 E0434

b. Rents Stationary/Owns Portable
Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Concentrator Yes No No No
E1377
E1378
E1379
E1380
E1381
E1382
E1383
E1384
E1385
E1400
E1401
E1402
E1403
E1404
E1405
E1406
Gaseous Yes No No No
E0424
Liquid Yes No No No
E0439

c. Owns Stationary/Owns Portable
Type of System
Stationary
Monthly
Payment
Oxygen
Content Fee
Portable Add-
On
Portable
Contents Fee
Concentrator No No No Yes
E0443
E0444
Gaseous No Yes No No
E0441
Liquid No Yes No No
E0442
d. Owns Stationary/Rents Portable
Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable Add-
On
Portable
Contents Fee
Concentrator No No Yes Yes
E0431
E0434
E0443
E0444
Gaseous No Yes Yes No
E0441 E0431
Liquid No Yes Yes No
E0442 E0434
3. Situation: Beneficiary Uses a Portable System Only
a. Rents Portable System (Beneficiary Uses a Portable System Only)
Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Gaseous No No Yes Yes
E0431 E0443

Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Liquid No No Yes Yes
E0434 E0444
b. Owns Portable System (Beneficiary Uses a Portable System Only)
Type of System Stationary
Monthly
Payment
Oxygen
Content Fee
Portable
Add-On
Portable
Contents Fee
Gaseous No No No Yes
E0443
Liquid No No No Yes
E0444
NOTE: For HHAs revenue codes 0601, 0602, 0603, and 0604 may apply when billing
for oxygen under the situations in this chart.
130.7 - Billing for Maintenance and Servicing (Providers and Suppliers)
(Rev. 1, 10-01-03)
A3-3629
General
Payment is not made for maintenance and servicing if the beneficiary rents the equipment
since payment for maintenance and servicing are included in the rental payments. An
exception to this is the 6-month service fee for capped rental items that the beneficiary
has elected not to purchase (see §40.2 and 130.5).
Where purchase is permitted (including "Capped Rental Items" and where the beneficiary
elects to purchase), payment for reasonable and necessary maintenance and servicing is
made for such purchased equipment.
Coding to Identify Maintenance and Servicing
Capped Rental

If the service is capped rental, suppliers that bill the DME MAC for the maintenance and
servicing fee (see §40.2) use modifier -MS with the HCPCS code for the equipment to
show that parts and labor which are not covered under any manufacturer or supplier
warranty.
The HHAs that bill the A/B MAC (HHH) for maintenance and servicing of capped rental
items use revenue code 0299 along with the appropriate HCPCS code for the equipment.
Not Capped Rental
Suppliers that bill the DME MACs for maintenance and servicing indicate the HCPCS
code of the item serviced and the modifier -RP, replacement or repair.
The HHAs that bill A/B MACs (HHH) for maintenance and servicing use revenue code
0299 and the appropriate HCPCS code for the equipment serviced.
Hospitals report revenue code 0274 along with one of the following HCPCS codes:
L4205, L4210, L7500, L7510, or L7520 when billing the A/B MAC (A) for maintenance
and servicing of prosthetics and orthotics.
130.8 - Installment Payments
(Rev. 1, 10-01-03)
A3-3629
Where a beneficiary is purchasing an item through installments, the total price of the
equipment item is reported on the first bill. Monthly payments are made (by the A/B
MAC (A), (B), (HHH), or DME MAC). The monthly amount is equivalent to the rental
fee schedule amount and is paid until the fee schedule purchase price or actual charge has
been reached, whichever comes first.
130.9 - Showing Whether Rented or Purchased
(Rev. 4052, Issued: 05-17-18, Effective: 10-01-18, Implementation: 10-01-18)
Claims must specify whether equipment is rented or
purchased. For purchased equipment, the itemized bill or
claim must also indicate whether equipment is new or
used. If the provider or supplier fails to indicate on an
assigned claim whether equipment was new or used, the
MAC processing the claims assumes purchased equipment
is used and process the claim accordingly, i.e., they pay on
the basis of the used purchase fee. If an unassigned
purchase claim does not specify whether the item was new
or used, MACs develop the claim with the supplier. The
following table indicates the HCPCS modifiers which are
added to the equipment code to indicate its status: Modifier
Status
-BP
The beneficiary has been
informed of the purchase and
rental options and has elected
to purchase the item
-BR
The beneficiary has been
informed of the purchase and
rental options and has elected
to rent the item
-BU
The beneficiary has been
informed of the purchase and
rental options and after 30
days has not informed the
supplier of his/her decision
-KH
DMEPOS item, initial claim,
purchase or first month rental
(no longer required for
purchased (NU modifier
claims) on or after 10/1/18)
-KI
DMEPOS item, second or
third month rental
-KJ
DMEPOS item, PEN pump or
capped rental months four to
fifteen
-NR
New when rented (use the
'NR' modifier when an item
that was new at the time of
rental is subsequently
purchased)
-NU
New equipment
-RR
Rental (use the 'RR' modifier
when DME is to be rented)
-UE
Used durable medical
equipment (no longer requires
the KH modifier for claims
submitted on or after 10/1/18)
HHAs report the appropriate modifier using the ASC X12 837 institutional claim format,
or Form CMS-1450 following the appropriate HCPCS code. A/B MACs (HHH) accept 7
positions in this field for data entry purposes.
140 - Billing for Supplies
(Rev. 1, 10-01-03)
140.1 - Billing for Supplies and Drugs Related to the Effective Use of
DME
(Rev. 10236, Issued: 07-31-2020, Effective: 08-31-2020, Implementation: 08-31-2020)
Suppliers and providers bill supplies that are necessary for the effective use of DME,
including drugs, with the appropriate HCPCS code identifying the supply. HHAs must
also report revenue code 0294, "Supplies/Drugs for DME Effectiveness."
Suppliers and providers, other than HHAs, bill supplies and drugs (not including drugs
that are necessary for the effective use of implanted DME) that are necessary for the
effective use of DME to the DME MACs. HHAs bill the A/B MACs (HHH).
Suppliers and providers, other than HHAs, bill for drugs that are necessary for the
effective use of implanted DME (HCPCS codes E0751, E0753, E0782, and E0783) to the
A/B MAC (B). HHAs bill the A/B MAC (HHH).
The A/B MACs (HHH) contact the DME MAC or A/B MAC (B) as necessary to
determine drug prices.
The DME MACs must:
• accept NDC codes for all drugs billed in the NCPDP format;
• accept NDC codes for oral anti-cancer drugs billed in the ASC X12 837
professional claim format, NCPDP format, and paper Form CMS-1500;
• accept HCPCS for all other drugs billed in the ASC X12 837 professional claim
format and paper Form CMS-1500 and
• return as unprocessable claims submitted with an invalid NDC using the
appropriate Remittance Advice Remark Code..
See the official Washington Publishing Company website for a current list of the
Remittance Advice Remark Codes.
140.1.1 - Supplier Payment Under Medicare Part B for Insulin
Furnished Through Durable Medical Equipment
(Rev. 12013; Issued: 05-02-23; Effective: 07-01-23; Implementation: 07-03-23)
Section 1833(b) of the Social Security Act (the Act) is amended by Section 11407 of the
Inflation Reduction Act, which waives the Medicare Part B deductible beginning July 1,
2023 for insulin furnished through an item of durable medical equipment covered under
section 1861(n) of the Act. Also, Section 1833(a) of the Act is amended by Section
11407 of the Inflation Reduction Act, which requires that beneficiary coinsurance for a
month’s supply of insulin furnished through an item of durable medical equipment is not
to exceed $35 beginning July 1, 2023. The supplier payment is to be adjusted as
necessary so that Medicare pays for the rest of the amount for the month’s supply of
insulin.
Effective July 1, 2023, to ensure the appropriate coinsurance is applied all claims billing
for insulin administered through an item of DME must have a modifier appended to
identify if the supply is for one month or a three month supply. Claims submitted for
insulin administered through an item of DME that do not include one of the modifiers
listed below will be returned to the supplier as un-processable.
JK - Short Descriptor: Drug supply 1 month or less;
Long Descriptor: One month supply or less of drug or biological
or
JL- Short Descriptor: Drug 3 month supply;
Long Descriptor: Three month supply of drug or biological
140.2 - Billing for HHA Medical Supplies
(Rev. 1, 10-01-03)
HHA-206.4, HHA-219.1, HHA-461 (partial), HO-228.3, SNF-260.3
Medical supplies are items that, due to their therapeutic or diagnostic characteristics, are
essential in enabling personnel to carry out effectively the care the physician has ordered
for the treatment or diagnosis of the patient's illness or injury. Medical supplies fit into
two categories. They are classified as:
• Routine because they are used in small quantities for patients during the usual
course of most home visits; or
• Nonroutine because they are needed to treat a patient's specific illness or injury in
accordance with the physician's plan of care and meet further conditions discussed
in more detail below.
Both routine and non-routine medical supplies are included in the home health PPS rate
and are not separately payable if the beneficiary is under a home health plan of care. The
CMS publishes a list of these medical supplies annually, identified by HCPCS code. If
no home health plan of care is in place, non-routine medical supplies are reported
separately on the bill and the supplies are payable on 34x bills.
140.3 - Billing DME MAC for Home Dialysis Supplies and Equipment
(Rev. 1, 10-01-03)
B3-3045.7
See Chapter 8 for claims processing instructions for Method II for suppliers and DME
MACs.
150 - Institutional Provider Reporting of Service Units for DME and
Supplies
(Rev. 2993, Effective: ASC X12 – 01-01-12, ICD-10 – Upon Implementation of ICD-
10; Implementation: ASC X12 – 08-25-14, ICD-10 – Upon Implementation of ICD-
10)
Provider outpatient departments report service units using the ASC X12 837 institutional
claim format or on the Form CMS 1450 the number of items being billed for orthotic and
prosthetic devices.
For purchased DMEPOS items (excluding items requiring frequent and substantial
servicing, capped rental items, and oxygen which cannot be purchased) HHAs report
service units using the ASC X12 837 institutional claim format or on the Form CMS-
1450 the number of purchased items billed. For rental DME items, including oxygen
equipment, HHAs report a separate line for each month billed indicating "1" on the ASC
X12 837 institutional claim format or in the service units field on the Form CMS-1450.
For oxygen contents (HCPCS codes E0441, E0442, E0443, and E0444), the HHAs report
the number of feet or pounds as described by the HCPCS code.
160 - Billing for Total Parenteral Nutrition and Enteral Nutrition
(Rev. 1, 10-01-03)
A3-3660.6
All providers and suppliers billing for parenteral and enteral nutrition covered as a Part B
prosthetic device benefit bill the DME MACs. Medicare pays for no more than a one-
month supply of parenteral or enteral nutrients for any one prospective billing period.
Claims submitted retroactively may include multiple months.
160.1 - Billing for Total Parenteral Nutrition and Enteral Nutrition
Furnished to Part B Inpatients
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
Inpatient Part A hospital or SNF care includes total parenteral nutrition (TPN) systems
and enteral nutrition (EN).
For inpatients for whom Part A benefits are not payable (e.g., benefits are exhausted or
the beneficiary is entitled to Part B only), total parenteral nutrition (TPN) systems and
enteral nutrition (EN) delivery systems are covered by Medicare as prosthetic devices
when the coverage criteria are met. When these criteria are met, the medical equipment
and medical supplies (together with nutrients) being used comprise covered prosthetic
devices for coverage purposes rather than durable medical equipment. However,
reimbursement rules relating to DME continue to apply to such items.
When a facility supplies TPN or EN systems that meet the criteria for coverage as a
prosthetic device to an inpatient whose care is not covered under Part A, the facility must
bill one of the DME MACs. Additionally, HHAs, SNFs, and hospitals that provide PEN
supplies, equipment and nutrients as a prosthetic device under Part B must use the ASC
X12 837 professional claim format or if permissible the Form CMS-1500 paper form to
bill the appropriate DME MAC. The DME MAC is determined according to the
residence of the beneficiary. Refer to §10 for jurisdiction descriptions.
A/B MACs (A) and (HHH) return claims containing PEN charges for Part B services
where the bill type is 12x, 13x, 22x, 23x, 32x, 33x, or 34x with instructions to the
provider to bill the DME MAC.
160.2 - Special Considerations for SNF Billing for TPN and EN Under
Part B
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
The HCPCS code and any appropriate modifiers are required.
SNFs bill the DME MAC for TPN and EN under Part B, using the ASC X12 837
professional claim format, or the Form CMS-1500 paper claim if applicable.
The following HCPCS codes apply.
B4034 B4035 B4036 B4081 B4082 B4083 B4084 B4085 B4150 B4151 B4152
B4153 B4154 B4155 B4156 B4164 B4168 B4172 B4176 B4178 B4180 B4184
B4186 B4189 B4193 B4197 B4199 B4216 B4220 B4222 B4224 B5000 B5100
B5200 B9000 B9002 B9004 B9006 E0776XA B9098 B9099
For SNF billing for PEN, a SNF includes the charges for PEN items it supplies
beneficiaries under Part A on its Part A bill. The services of SNF personnel who
administer the PEN therapy are considered routine and are included in the basic Part A
payment for a covered stay. SNF personnel costs to administer PEN therapy are not
covered under the Part B prosthetic device benefit.
If TPN supplies, equipment and nutrients qualify as a prosthetic device and the stay is not
covered by Part A, they are covered by Part B. Part B coverage applies regardless of
whether the TPN items were furnished by the SNF or an outside supplier. The Part B
TPN bill must be sent to the DME Medicare Administrative Contractor regardless of
whether supplied by the SNF or an outside supplier.
Enteral nutrients provided during a stay that is covered by Part A are classified as food
and included in the routine Part A payment sent to the SNF. (See the Medicare Provider
Reimbursement Manual, §2203.1E.) Parenteral nutrient solutions provided during a
covered Part A SNF stay are classified as intravenous drugs. The SNF must bill these
services as ancillary charges. (See the Medicare Provider Reimbursement Manual,
§2203.2.)
170 - Billing for Splints and Casts
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
The cost of supplies used in creating casts are not included in the payment amounts for
the CPT codes for fracture management and for casts and splints. Thus, for settings in
which CPT codes are used to pay for services that include the provision of a cast or
splint, supplies maybe billed with separate CPCS codes. The work and practice expenses
involved with the creation of the cast or splint are included in the payment for the code
for that service.
For claims with dates of service on or after July 1, 2001, jurisdiction for processing
claims for splints transferred from the DME MACs to the A/B MAC (B). The A/B
MACs (B) have jurisdiction for processing claims for splints and casts, which includes
codes for splints that may have previously been billed to the DME MACs.
Jurisdiction for slings is jointly maintained by the A/B MACs (B) (for physician claims)
and the DME MACs (for supplier claims). Notwithstanding the above where the
beneficiary receives the service from any of the following providers claims jurisdiction is
with the A/B MAC (A). An exception to this is hospital outpatient services and hospital
inpatient Part B services, which are included in the OPPS payment and are billed to the
A/B MAC (A) using the ASC X12 837 institutional claim format or Form CMS- 1450).
Other providers and suppliers that normally bill the A/B MAC (A) for services bill the
A/B MAC (B) for splints and casts.
180 - Billing for Home Infusion Therapy Services
(Rev. 4112, Issued: 08-10-18, Effective: 01-01-19, Implementation: 01-07-19)
Effective January 1, 2019 and until the implementation of the full home infusion therapy
benefit, Medicare makes separate temporary transitional payments for Home Infusion
Therapy (HIT) services to eligible home infusion suppliers (i.e., a licensed pharmacy that
provides external infusion pumps and external infusion pump supplies). This payment
amount covers the cost of professional services, including nursing services, training and
education (not otherwise paid for as durable medical equipment), remote monitoring, and
monitoring services for the provision of home infusion therapy furnished by a qualified
home infusion with administration of certain transitional home infusion drugs
administered through an item of DME.
Temporary transitional payments are made for HIT services based on the home infusion
drug provided. Home infusion drugs are assigned to three payment categories,
determined by the Healthcare Common Procedure Coding System (HCPCS) J-code.
Each DME MAC maintains a list of drugs that are administered through an item of DME
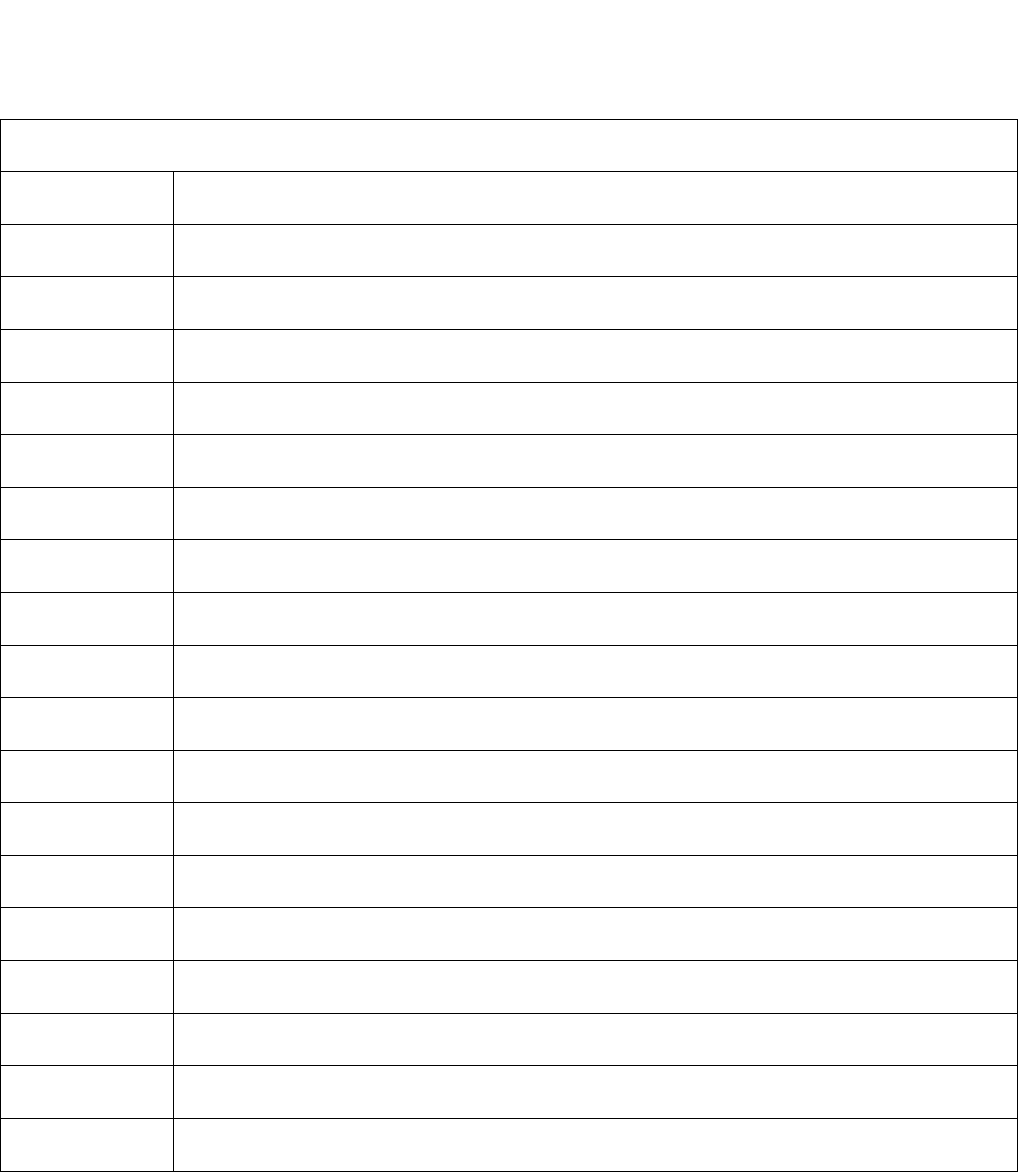
and HIT payment is made for days on which home infusion therapy services are
furnished by skilled professionals in the individual’s home on the day of infusion drug
administration.
Temporary Transitional Payment Categories for Home Infusion Therapy Services,
by Infusion Drug (J-Code)
Category 1
J-Code Description
J0133 Injection, acyclovir, 5 mg
J0285 Injection, amphotericin b, 50 mg
J0287 Injection, amphotericin b lipid complex, 10 mg
J0288 Injection, amphotericin b cholesteryl sulfate complex, 10 mg
J0289 Injection, amphotericin b liposome, 10 mg
J0895 Injection, deferoxamine mesylate, 500 mg
J1170 Injection, hydromorphone, up to 4 mg
J1250 Injection, dobutamine hydrochloride, per 250 mg
J1265 Injection, dopamine hcl, 40 mg
J1325 Injection, epoprostenol, 0.5 mg
J1455 Injection, foscarnet sodium, per 1000 mg
J1457 Injection, gallium nitrate, 1 mg
J1570 Injection, ganciclovir sodium, 500 mg
J2175 Injection, meperidine hydrochloride, per 100 mg
J2260 Injection, milrinone lactate, 5 mg
J2270 Injection, morphine sulfate, up to 10 mg
J2274 Injection, morphine sulfate, preservative-free for epidural or intrathecal use, 10 mg
J2278 Injection, ziconotide, 1 microgram

J3010 Injection, fentanyl citrate, 0.1 mg
J3285 Injection, treprostinil, 1 mg
Category 2
J-Code Description
J1555 JB Injection, immune globulin (cuvitru), 100 mg
J1559 JB Injection, immune globulin (hizentra), 100 mg
J1561 JB Injection, immune globulin, (gamunex-c/gammaked), non-lyophilized (e.g., liquid),
500 mg
J1562 JB Injection, immune globulin (vivaglobin), 100 mg
J1569 JB Injection, immune globulin, (gammagard liquid), non-lyophilized, (e.g., liquid), 500
mg
J1575 JB Injection, immune globulin/hyaluronidase, (hyqvia), 100 mg immune globulin
Category 3
J-Code Description
J9000 Injection, doxorubicin hydrochloride, 10 mg
J9039 Injection, blinatumomab, 1 microgram
J9040 Injection, bleomycin sulfate, 15 units
J9065 Injection, cladribine, per 1 mg
J9100 Injection, cytarabine, 100 mg
J9190 Injection, fluorouracil, 500 mg
J9200 Injection, floxuridine, 500 mg
J9360 Injection, vinblastine sulfate, 1 mg
J9370 Injection, vincristine sulfate, 1 mg
The payment category for subsequent transitional home infusion drug additions to the
Local Coverage Determinations (LCDs) and compounded infusion drugs not otherwise

classified, as identified by HCPCS codes J7799 and J7999, will be determined by the
DME MAC.
A single unit of payment will be made for HIT services provided in the individual’s home
during an infusion drug administration calendar day.
Suppliers will report the following HCPCS G-codes associated with the payment
categories for the professional services furnished in the individual’s home and on an
infusion drug administration calendar day:
1. G0068: Professional services for the administration of anti-infective, pain
management, chelation, pulmonary hypertension, and/or inotropic infusion
drug(s) for each infusion drug administration calendar day in the individual’s
home, each 15 minutes.
Short Descriptor: Adm of infusion drug in home
2. G0069: Professional services for the administration of subcutaneous
immunotherapy for each infusion drug administration calendar day in the
individual's home, each 15 minutes.
Short Descriptor: Adm of immune drug in home
3. G0070: Professional services for the administration of chemotherapy for each
infusion drug administration calendar day in the individual's home, each 15
minutes.
Short Descriptor: Adm of chemo drug in home
In the event that multiple drugs, which are not all assigned to the same payment category,
are administered on the same infusion drug administration calendar day, a single payment
would be made that is equal to the highest payment category.
Providers should report visit length in 15-minute increments (15 minutes=1 unit). See
the table below for the rounding of units.
Rounding of Time Units

Unit Time
1 <23 minutes
2 = 23 minutes to <38 minutes
3 = 38 minutes to <53 minutes
4 = 53 minutes to <68 minutes
5 = 68 minutes to <83 minutes
6 = 83 minutes to <98 minutes
7 = 98 minutes to <113 minutes
8 = 113 minutes to <128 minutes
9 = 128 minutes to <143 minutes
10 = 143 minutes to <158 minutes
Claims that include G-codes for HIT services are not required to, but may also include
the HCPCS J-code for the infusion drug, the E-code for the external infusion pump, and
A-codes for supplies other than the drug.
A submitted claim for HIT services is subject to a Common Working File (CWF) edit in
the event that a transitional drug J-code is not found on the same claim as the billed
professional HIT services, or in claims history in the previous 30 days. If a J-code is not
found on the same claim as the billed professional services, the claims processing system
will recycle the G-code claim for the professional services associated with the
administration of the home infusion drug, until a claim containing the J-code for the
infusion drug is received in the CWF. The professional visit claim will recycle three
times (with a 30-day look back period) for a total of 15 business days. After 15 business
days, if no J-code claim is found in claims history, the G-code claim will be denied.
Suppliers must ensure that the appropriate drug associated with the visit is billed with the
visit or no more than 30 days prior to the visit. Visits are denied if the appropriate drug
for the visit is not billed. In the event that multiple visits occur on the same date of
service, suppliers must only bill for one visit and should report the highest paying visit
with the applicable drug. Claims reporting multiple visits on the same line item date of
service will be returned as unprocessable.
181 – Lymphedema Compression Treatment Benefit
(Rev. 12741; Issued: 01-24-24; Effective: 01-01-24; Implementation:01-02-24)
Effective for items furnished on or after January 1, 2024, section 4133 of the
Consolidated Appropriations Act (CAA), 2023, establishes a new Medicare DMEPOS
benefit category for standard and custom fitted compression garments and additional
lymphedema compression treatment items for the treatment of lymphedema that are
prescribed by an authorized practitioner.
Claims for lymphedema treatment items that do not have an appropriate diagnosis for
lymphedema will be denied. Claim payment can be made for lymphedema compression
treatment items for more than one body part/area per beneficiary. In addition, claim
payment can be made for both a daytime and nighttime garment for the same body
part/area per beneficiary.
A quantity of three daytime garments or wraps per body area and two nighttime garment
per body area is allowed. Any amount billed that exceeds frequency limitations will be
denied unless a replacement is needed due to a change in medical need or because a
garment or wrap is lost, stolen, or irreparably damaged. Replacement of the garments can
only be made in accordance with the proposed frequency limitation of once every 6
months for a daytime garment or wrap and once every two years for a nighttime garment.
When billing for replacement of a garment or wrap use of the RA modifier is required.
181.1 - Payment Policy for Lymphedema Compression Treatment Items
(Rev. 12557; Issued:03-28-24; Effective: 01-01-24; Implementation: 04-29-24)
Payment for lymphedema compression treatment items is made in a lump sum payment
for standard or custom daytime gradient compression garments, nighttime gradient
compression garments, gradient compression wraps with adjustable straps, accessories
necessary for the effective use of gradient compression garments and wraps with
adjustable straps, compression bandaging supplies, and other lymphedema
compression treatment items described in section 145 of chapter15 of the Medicare
Benefit Policy Manual.
A national Medicare allowed payment amount is established for each lymphedema
compression treatment item and is updated on an annual basis. Payment is based on 80
percent of the lesser of the supplier’s actual charge or the national Medicare allowed
payment amount for the item.
In accordance with regulations at 42 CFR §414.1660, if a new HCPCS code is added
for a lymphedema compression treatment item, CMS and/or DME MACs make efforts
to determine whether the item has a pricing history. If there is a pricing history, the
previous payment amounts for the previous code(s) are mapped to the new code(s) to
ensure continuity of pricing. When the code for an item is divided into several codes for
the components of that item, the total of the separate payment amounts established for
the components must not be higher than the payment amount for the original item.
When there is a single code that describes two or more distinct complete items (for
example, two different but related or similar items), and separate codes are
subsequently established for each item, the payment amounts that applied to the single
code continue to apply to each of the items described by the new codes. When the codes
for the components of a single item are combined in a single global code, the payment
amounts for the new code are established by totaling the payment amounts used for the
components (that is, use the total of the payment amounts for the components as the
payment amount for the global code). When the codes for several different items are
combined into a single code, the payment amounts for the new code are established
using the average (arithmetic mean), weighted by allowed services, of the payment
amounts for the formerly separate codes.
National Medicare payment amounts for new lymphedema compression treatment items
that do not have a pricing history are established using the public meeting process and
procedures described in regulations at 42 CFR §414.1670. If a new code for a
lymphedema compression treatment item that does not have a pricing history takes
effect before the national payment amount is established using the public meeting
process, until the national payment amount is established for the code/item, the DME
MACs consider what an appropriate payment amount is for the item on an individual,
claim-by-claim basis and may consider using pricing for similar items that already
have established payment amounts.
190 - A/B MAC (A), (B), or (HHH), or DME MAC Application of Fee
Schedule and Determination of Payments and Patient Liability for
DME Claims
(Rev. 1, 10-01-03)
A3-3629, B3-5102
The following instructions apply to all A/B MACs (A), (B), and (HHH), and DME
MACs processing DMEPOS claims:
First the 'allowable amount' is determined. This is the lower of the fee schedule amount
or the billed charge.
The application of deductible and coinsurance are calculated as follows.
A. Claims to A/B MACs (B) or DME MACs
Any unmet deductible is subtracted from the allowed amount and 80 percent of the
remainder is paid.

B. Claims to A/B MACs (A) or (HHH)
NOTE: Per 42 CFR 410.2 (Follow the link, choose the applicable year, select Title 42,
then open Chapter IV. You then must choose which part to open. To get to §410.2 you
select the second choice and open it, then select Part 410 and download the pdf version.),
a nominal charge provider means a provider that furnishes services free of charge or at a
nominal charge, and is either a public provider or another provider that (1) demonstrates
to CMS's satisfaction that a significant portion of its patients are low-income; and (2)
requests that payment for its services be determined accordingly.
1. Payment to a Provider Other Than Nominal Charge Provider
To determine the Part B payment to a provider other than nominal charge provider, A/B
MACs (A) and (HHH) subtract any unmet Part B deductible from the lower of the actual
charge or the fee schedule amount for the item or service and multiply the remainder by
80 percent. This is the final payment. (If the item or service is furnished by a HHA and
is covered under a plan of care, the payment is determined in the same way, except that
no deductible is applicable.)
2. Payment to a Nominal Charge HHA
To determine the Part B payment to a nominal charge HHA, A/B MACs (HHH) subtract
any unmet Part B deductible from the fee schedule amount and multiply the remainder by
80 percent. This is the final payment. (If the item or service is covered under a plan of
care, the payment is determined in the same way, except that no deductible is applicable.)
For these items and services, no providers other than HHAs are considered nominal
charge providers.
3. Payment to a Nominal Charge Provider Other Than a Nominal Charge HHA
To determine the Part B payment to a nominal charge provider other than a nominal
charge HHA, A/B MACs (A) and (HHH) subtract any unmet Part B deductible from the
lower of the actual charge or the fee schedule amount and multiply the remainder by 80
percent. This is the final payment.
4. Patient Liability to a HHA Other Than a Nominal Charge HHA
To determine the patient liability to a HHA other than a nominal charge HHA under Part
B, A/B MACs (HHH) subtract any unmet deductible from the lower of the actual charge
or fee schedule amount and multiply the remainder by 20 percent. The result, plus the
unmet deductible is the patient's liability. If the item or service is covered under a plan of
care, the deductible does not apply.
5. Patient Liability to a Nominal Charge HHA
To determine patient liability to a nominal charge HHA under Part B, A/B MACs (HHH)
subtract any unmet deductible from the fee schedule amount and multiply the remainder
by 20 percent. The result, plus the unmet deductible is the patient's liability. If the item
or service is covered under a Plan of Care, the deductible does not apply.
6. Patient Liability to a Provider Other Than a HHA
To determine patient liability to a provider other than an HHA (including nominal charge
providers other than a HHA), A/B MACs (A) subtract any unmet deductible from the
actual charge and multiply the remainder by 20 percent. The result, plus the unmet
deductible is the patient's liability. Coinsurance is applied as applicable.
The following describes application of deductible and coinsurance on HHA bills by bill
type:
a. Patient Under Part B Plan of Treatment (Bill Type 32X)
• No deductible applicable; and
• No coinsurance applicable
Exception: Coinsurance applies on DME and orthotic/prosthetic claims.
b. Patient Under Part A Plan of Treatment (Bill Type 33X)
• No deductible applicable; and
• No coinsurance applicable
Exception: Coinsurance applies on DME and orthotic/prosthetic claims.
c. Patient Not Under Plan of Treatment, Part B Medical and Other Health
Services and Osteoporosis Injections (Bill Type 34X)
• Deductible applies; and
• Coinsurance applies
The following examples illustrate how to calculate provider payment and patient liability
in various situations. The examples, like the preceding rules for HHAs, address items
and services not under a Plan of Care and, therefore, include deductible application. The
Note following each HHA example addresses items and services obtained under a Plan of
Care and, therefore, do not address deductible application.
EXAMPLE 1: CLAIM CONTAINING ONLY ORTHOTIC/PROSTHETIC CHARGES
$200.00 Orthotic/prosthetic charges
$140.00 Orthotic/prosthetic fee schedule amount
$100.00 Part B deductible to be met
To determine the payment to all providers (other than nominal charge HHAs) apply the
following steps:
Step 1:
Determine the lower of the actual charge or the fee schedule amount:
$140.00 (do not apply the provider's interim rate)
Step 2:
Subtract any unmet Part B deductible from the amount determined in
Step 1: $140.00 - $100.00 = $40.00
Step 3:
Apply 80% to the amount determined in Step 2: $40.00 X 80% = $32.00
The Part B payment to the provider in this example is $32.00
To determine payment to nominal charge HHAs apply the following steps:
Step 1:
Subtract any unmet deductible from the fee schedule amount: $140.00 -
$100.00 = $40.00
Step 2:
Apply 80% to the amount determined in Step 1: $40.00 x 80% = $32.00
The Part B payment to the nominal charge HHA in this example is $32.00
NOTE: If the item or service is covered under a Home Health Plan of Care, the payment
is determined the same way, except no deductible is applicable. In the above examples
the payment would be $112.00 ($140.00 x 80%).
To determine beneficiary liability to providers other than HHAs apply the following
steps:
Step 1:
Subtract any unmet Part B deductible from the actual charge: $200.00 -
$100.00 = $100.00
Step 2:
Multiply the amount determined in Step 1 by 20% coinsurance: $100.00
x 20% = $20.00
Step 3:
Add the result of Step 2 to the unmet deductible: $20.00 + $100.00 =
$120.00
The beneficiary's liability in this example is $120.00. ($100.00 Part B deductible and
$20.00 coinsurance.)
NOTE: If the item of service is covered under a Home Health Plan of Care, the
beneficiary's liability is determined the same way, except no deductible is applicable. In
this example, the beneficiary's liability would be $28.00 ($140.00 x 20% coinsurance).
EXAMPLE 2: CLAIM CONTAINING ONLY ORTHOTIC/PROSTHETIC CHARGES
- NEGATIVE PAYMENT
$120.00 Orthotic/prosthetic charges
$ 80.00 Orthotic/prosthetic fee schedule amount
$100.00 Part B deductible to be met
To determine the payment to all providers (other than nominal charge HHAs) apply the
following steps:
Step 1:
Determine the lower of the actual charge or the fee schedule amount:
$80.00 (do not apply the provider's interim rate)
Step 2:
Subtract any unmet Part B deductible from amount determined in Step 1:
$80.00 - $100.00 = -$20.00
Do not apply the 80 percent since the result of Step 2 is a negative amount. There is no
Part B payment to the provider in this example because the result equals a negative
payment amount. A/B MACs (A) or (HHH) do not take the negative amount of (-$20.00)
from future payments to the provider.
To determine payment to nominal charge HHAs, apply the following step:
Step 1:
Subtract any unmet deductible from the fee schedule amount: $80.00 -
$100.00 = -$20.00
Do not apply the 80 percent since the result of Step 1 is a negative amount. There is no
Part B payment to the nominal charge HHA in this example because the result equals a
negative payment amount. A/B MACs (HHH) do not take the negative amount of (-
$20.00) from future payments to the HHA.
NOTE: If the item or service is covered under a Home Health Plan of Care the payment
is determined in the same way, except no deductible is applicable. In the above examples
the payment would be $64.00 ($80.00 x 80%).
To determine beneficiary liability to providers other than HHAs, apply the following
steps:
Step 1:
Subtract any unmet Part B deductible from the actual charge: $120.00 -
$100.00 = $20.00
Step 2:
Multiply the amount in Step 1 by 20% coinsurance: $20.00 x 20% =
$4.00
The beneficiary's liability in this example is $104.00 ($100.00 Part B deductible and
$4.00 coinsurance).
The beneficiary's liability to HHAs (nominal charge and other than nominal charge) in
this example is $80.00 (the fee schedule amount for nominal charge HHAs or the lower
of the fee schedule amount or the actual charge for other than nominal charge HHAs).
The HHA cannot charge the beneficiary the $100.00 deductible since it exceeds $80.00.
$80.00 is credited to the beneficiary's deductible. The beneficiary's deductible to be met
on the next claim is $20.00. The beneficiary has no coinsurance obligation.
NOTE: If the item or service is covered under a Home Health Plan of Care, the
beneficiary's liability is determined the same way, except that no deductible is applicable.
The beneficiary's liability in this example would be $16.00 coinsurance ($80.00 x 20%).
200 - Automatic Mailing/Delivery of DMEPOS
(Rev. 1, 10-01-03)
Suppliers/manufacturers may not automatically deliver DMEPOS to beneficiaries unless
the beneficiary, physician, or designated representative has requested additional
supplies/equipment. The reason is to assure that the beneficiary actually needs the
DMEPOS. DME MAC review should be done on a post-pay basis.
A beneficiary or their caregiver must specifically request refills of repetitive services
and/or supplies before a supplier dispenses them. A supplier may not initiate a refill of
an order. The supplier must not automatically dispense a quantity of supplies on a
predetermined regular basis.
A request for refill is different than a request for a renewal of a prescription. Generally,
the beneficiary or caregiver will rarely keep track of the end date of a prescription.
Furthermore the physician is not likely to keep track of this. The supplier is the one who
will need to have the order on file and will know when the prescription will run out and a
new order is needed. It is reasonable to expect the supplier to contact the physician and
ask for a renewal of the order. This is consistent with the DME MAC Supplier Manual
for the particular jurisdiction, which states: "The description of the item (on an order)
may be completed by someone other than the physician (most commonly the supplier).
However, the physician must review the order and sign and date it to indicate
agreement." Again the supplier must not automatically mail or deliver the DMEPOS to
the beneficiary until specifically requested.
The DME MACs inform suppliers of these procedures via their bulletins and training
sessions. These procedures will benefit suppliers by helping to maximize claims
processing accuracy, and to reduce the likelihood of a postpayment claim denial because
the DMEPOS were not medically necessary.
DME MACs must publish this information on their Web sites and in their bulletins on an
annual basis.
210 - CWF Crossover Editing for DMEPOS Claims During an Inpatient
Stay
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
I. General Information
A. Background:
In general, the DMEPOS benefit is meant only for items a beneficiary is using in his or
her home. For a beneficiary in a Part A inpatient stay, an institutional provider (e.g.,
hospital) is not defined as a beneficiary’s home for DMEPOS, and so Medicare does not
make separate payment for DMEPOS when a beneficiary is in the institution. The
institution is expected to provide all medically necessary DMEPOS during a
beneficiary’s covered Part A stay.
EXCEPTION: Medicare makes a separate payment for a full month for DMEPOS
items, provided the beneficiary was in the home on the “from” date or anniversary date
defined below.
For capped rental items of durable medical equipment (DME) where the DME supplier
submits a monthly bill, the date of delivery (“from” date) on the first claim must be the
“from” or anniversary date on all subsequent claims for the item. For example, if the first
claim for a wheelchair is dated September 15, all subsequent bills must be dated for the
15th of the following months (October 15, November 15, etc.).
B. Policy:
If a beneficiary using DMEPOS is at home on the “from” date or anniversary date,
Medicare pays for the DMEPOS for the entire month, even if the “from” date is the date
of discharge from the institutional provider.
If a beneficiary using DMEPOS is in a covered Part A stay for a full month, Medicare
does not make payment for the DMEPOS for that month.
For capped rental items, if the covered Part A stay overlaps the anniversary date (“from”
date on the claim), and the beneficiary is not in the covered Part A stay for the entire
month, the date of discharge becomes the new anniversary date (“from” date on the
claim) for subsequent claims. In this situation, the supplier must submit a new claim with
the date of discharge as the new anniversary date upon the beneficiary’s release from the
institution. Suppliers should annotate the claims, to indicate that the patient was in an
institution, resulting in the need to establish a new anniversary date.
The CWF:
• rejects a DME MAC claim that contain DMEPOS HCPCS codes when the DME
MAC claim has a date of service that falls within the inpatient stay;
• considers an inpatient stay to include all days prior to the date of discharge;
• processes a DME MAC claim that contain DMEPOS HCPCS codes when the DME
MAC claim has the same “from” date equal to the date of inpatient discharge;
• validates for a crossover service on a DME MAC claim for an inpatient beneficiary
based on the “from” date only of the DME MAC claim;
• identifies a DME MAC claim for maintenance and servicing by the “MS” modifier;
and
• allows payment for a DME MAC claim for maintenance and servicing of capped
rental items when a claim contains the “MS” modifier.
The CWF approves to pay maintenance and servicing claims regardless of whether the
beneficiary is in an institutional setting or in the home environment.
The changes in the general policy apply to all items of DMEPOS paid by the DME
MACs, however, changes in anniversary date billing apply only to capped rental DME.
In cases where the anniversary date falls at the end of the month (for example January 31)
and a subsequent month does not have a day with the same date (for example, February),
the DME MAC uses the final date in the calendar month (for example, February 28).
EXAMPLE 1:
A beneficiary rents a wheelchair beginning on January 1. The DME MAC determines
that the wheelchair is medically necessary and that the beneficiary meets all coverage
criteria, and so begins to make payment on the wheelchair. The beneficiary enters a
covered a hospital on February 15 and is discharged on April 5.
In this example, Medicare pays for the entire month of February, because the patient was
in the home for part of the month. However, the DME MAC denies the claim for March,
because the patient was in a covered hospital stay for the entire month.
Because the anniversary date (“from” date) of the monthly bill was April 1, and the
patient was still in the covered hospital stay on that date, the DME supplier must not
submit another claim until April 5 (the date of discharge). April 5 becomes the new
anniversary date (“from” date) for billing purposes, so the supplier would now bill on the
5th of the month rather than the 1st of the month for the remainder of the capped rental
period. The supplier should annotate the claim to indicate that the patient was in a
hospital on the first claim with the new anniversary date.
EXAMPLE 2:
A beneficiary receives oxygen on January 1. On February 28, the patient enters a
hospital and is discharged on March 15.
In this example, the DME MAC denies a claim dated March 1. The supplier submits a
new claim dated March 15, which would then become the anniversary date for billing
purposes. The supplier should annotate the claim to indicate that the patient was in a
hospital on the first claim with the new anniversary date.

EXAMPLE 3:
A beneficiary rents a hospital bed beginning on January 1. On March 15, the patient
enters a hospital and is discharged on March 25.
In this example, the DME MAC pays for the entire month of March.
EXAMPLE 4:
A beneficiary rents a wheelchair beginning December 15. On January 1, the patient
enters a hospital and is discharged on January 31.
In this example, the DME MAC denies the claim dated January 15. The supplier submits
a new claim dated January 31, which becomes the anniversary date for billing purposes.
The supplier should annotate the claim to indicate that the patient was in a hospital on the
first claim with the new anniversary date. The February claim would be dated February
28 because there is no 31st day in February.
211 - SNF Consolidated Billing and DME Provided by DMEPOS
Suppliers
(Rev. 222, Issued: 07-02-04) (Effective/Implementation: Not Applicable)
211.1 - General Information
(Rev. 222, Issued: 07-02-04) (Effective/Implementation: Not Applicable)
The Social Security Act (§1861(n)) specifies that a hospital or a skilled nursing facility
(SNF) cannot be considered a patient’s “home” for purposes of the DME benefit. (This
restriction of coverage to only those items that are furnished for use in the patient’s home
does not apply to coverage under the separate Part B benefits for Prosthetics, Orthotics,
and Supplies, which are payable without regard to the particular setting in which they are
furnished.)
When DME is furnished for use in a SNF during a covered Part A stay, the DME MACs
shall not make separate payment for DME, since the DME is already included in the
payment that the SNF receives for the covered stay itself. When DME is furnished for
use in a SNF during a noncovered stay (SNF benefits exhausted, no qualifying 3-day
hospital stay, etc.), the DME MACs still shall not make separate payment for DME, as
explained above, Part B’s DME benefit does not cover DME items that are furnished for
use in SNFs. Even if a patient already rents or owns a piece of DME in their home, the
SNF cannot require the patient to bring their own rented or purchased DME with them
into the SNF.
211.2 - Partial Month Stays For Capped Rental Equipment
(Rev. 2993, Effective: ASC X12 - 01-01-12, ICD-10 - Upon Implementation of ICD-
10; Implementation: ASC X12 - 08-25-14, ICD-10 - Upon Implementation of ICD-
10)
A. General Rule
For capped rental DME items where the DME supplier submits a monthly bill, the date of
delivery (the “from” date) on the first claim must be the “from”, or “anniversary date”, on
all subsequent claims for the item. For example, if the first claim for a wheelchair is
dated September 15, all subsequent bills must be dated on the 15
th
of the following
months (October 15, November 15, etc.).
The following instructions discuss DME payment when the DME is furnished during a
month in which the beneficiary spends part of the month in a SNF, and part of the month
in his or her own home. In accordance with DME payment policy, Medicare will make
separate payment for a full month for DME items in such situations, provided the
beneficiary was in the home on the “from” date or “anniversary date” defined above.
B. Policy
If a beneficiary using DME is at home on the “from” or “anniversary date”, Medicare
will make payment for DME for the entire month, even if the “from” date is the date of
discharge from the SNF.
If a beneficiary using DME is in a covered Part A stay in a SNF for a full month,
Medicare will not make payment for DME for that month.
For capped rental items, if the covered Part A SNF stay overlaps the “from” or
“anniversary date” of the Certificate of Medical Necessity (CMN), and the beneficiary is
not in the covered Part A SNF stay for the entire month, the date of discharge becomes
the new “anniversary date” for subsequent claims. In this situation, the supplier must
submit a new claim with the date of discharge as the new anniversary date upon the
beneficiary’s release from the SNF. Suppliers should annotate claims, to indicate that the
patient was in a SNF, resulting in the need to establish a new anniversary date.
NOTES: The DME MACs must continue to make payment for maintenance and
servicing of capped rental items regardless of whether the beneficiary is in a covered Part
A SNF stay on the date of service of the maintenance and servicing claim.
The DME MACs must make payment for DME on the date of discharge from a covered
Part A SNF stay. Claims must edit based on the “from” date of the claim and not the
“through” date of the claim.
EXAMPLE 1:
A beneficiary rents a wheelchair beginning on January 1. The DME MAC determines
that the wheelchair is medically necessary and that the beneficiary meets all coverage
criteria, and so begins to make payment on the wheelchair. The beneficiary enters a
covered Part A stay in a SNF on February 15 and is discharged on April 5. In this
example, Medicare will make payment for the entire month of February, because the
patient was in the home for part of the month. However, the DME MAC will deny the
claim for March, because the patient was in a covered Part A stay in the SNF for the
entire month.
Because the anniversary date (“from” date) of the monthly bill was April 1, and the
patient was still in the covered Part A stay in a SNF on that date, the DME supplier must
not submit another claim until April 5 (the date of discharge). April 5 becomes the new
anniversary date (“from” date) for billing purposes, so the supplier would now bill on the
5
th
of the month rather than the 1
st
of the month for the remainder of the capped rental
period. The supplier should annotate the claim to indicate that the patient was in a SNF
on the first claim with the new anniversary date.
EXAMPLE 2:
A beneficiary receives oxygen on January 1. On February 28, the patient enters a
covered Part A stay in a SNF and is discharged on March 15.
In this example, the DME MAC would deny a claim dated March 1. The supplier would
submit a new claim dated March 15, which would then become the anniversary date for
billing purposes. The supplier should annotate the claim to indicate that the patient was
in a covered Part A stay in a SNF on the first claim with the new anniversary date.
EXAMPLE 3:
A beneficiary rents a hospital bed beginning on January 1. On March 15, the patient
enters a covered Part A stay in a SNF and is discharged on March 25.
In this example, the DME MAC will make payment for the entire month of March.
NOTE: The changes in the general policy in this instruction apply to all items of DME
paid by the DME MACs. However, changes in “anniversary date” billing requirements
only apply to capped rental DME.
212 - Home Health Consolidated Billing and Supplies Provided by
DMEPOS Suppliers
(Rev. 2977, Issued; 06-20-14, Effective: 09-23-14; ICD-10: Upon Implementation of
ICD-10, Implementation: 09-23-14; ICD-10: Upon Implementation of ICD-10)
Section 1842 (b)(6)(F) of the Social Security Act requires consolidated billing of all
home health services while a beneficiary is under a home health plan of care authorized
by a physician. Consequently, Medicare makes payment for all such items and services
to a single home health agency (HHA) overseeing that plan.
The law states payment will be made to the HHA without regard as to whether or not the
item or service was furnished by the agency, by others under arrangement to the HHA, or
when any other contracting or consulting arrangements exist with the primary HHA, or
“otherwise.” Payment for all items is included in the home health prospective payment
system (HH PPS) episode payment the HHA receives.
Nonroutine medical supplies are among the types of services that are subject to the home
health consolidated billing provision. Medicare periodically publishes Recurring Update
Notifications that contain updated lists of nonroutine supply codes that must be included
in home health consolidated billing. These services may not be billed separately by a
DMEPOS supplier when a Medicare beneficiary is in a HH PPS episode of care.
Durable Medical Equipment (DME), including prosthetics, orthotics and oxygen, is
exempt from home health consolidated billing by law.
For detailed information regarding home health consolidated billing, DMEPOS suppliers
should refer to chapter 10, section 20 of this manual.
213- Billing for Home IVIG Items and Services
(Rev. 12437, Issued: 12-28-23, Effective: 01-01-24, Implementation: 01-02-24)
Effective January 1, 2024, Medicare makes a separate bundled payment for home intravenous
immune globulin (IVIG) items and services to DME suppliers. This payment amount covers the
cost of nursing services and supplies including an infusion set and tubing, for the provision of
IVIG administration in the home by a DME supplier.
The items and services payment is made per visit for days on which the IVIG is administered by
a nurse in the patient’s home. The patient must have a diagnosis of Primary Immune Deficiency
Disease (PIDD) as indicated in the Intravenous Immune Globulin Policy Article (A5209).
Payment for home IVIG items and services is only made when the patient is receiving one of the
IVIG products listed on the Local Coverage Determination (LCD) for Intravenous Immune
Globulin (L33610).
A single payment will be made for the items and services provided on the calendar day when
such items and services are furnished in the home. The HCPCS (Q2052) “Services, Supplies,
and Accessories used in the Home for the Administration of Intravenous Immune Globulin”)
will be billed separately from, or on the same claim as, the J-code for the IVIG product. The Q-
code should be billed as a separate claim line on the same claim for the same place of service as
the J-code for the IVIG. In cases where the IVIG product is mailed or delivered to the patient
prior to administration, the date of service for the administration of the IVIG (the Q-code) may be
no more than 30 calendar days after the date of service on the IVIG product claim line. No more
than one Q-code should be billed per claim line per date of service.
If a provider is billing for multiple administrations of IVIG on a single claim, then the supplier
would bill the Q-code for each date of service on a separate claim line, which would be payable
per visit (that is, each time the IVIG is administered). There may be situations in which multiple
units of IVIG are shipped to the patient and billed on a single “J” code claim line followed by
more than one Q-code administration claim line, each with the date of service on which the IVIG
was administered. However, only one unit of service (Q-code) shall be paid per infusion date of

service.
Providers should report visit length in 15-minute increments (15 minutes=1 unit) ) when billing
for IVIG (Q2052). See the table below for the rounding of units.
Rounding of Time Units
Unit
Time
1
<23 minutes
2
= 23 minutes to <38 minutes
3
= 38 minutes to <53 minutes
4
= 53 minutes to <68 minutes
5
= 68 minutes to <83 minutes
6
= 83 minutes to <98 minutes
7
= 98 minutes to <113 minutes
8
= 113 minutes to <128 minutes
9
= 128 minutes to <143 minutes
10
= 143 minutes to <158 minutes
A submitted claim for home IVIG items and services is subject to a Common Working File (CWF)
edit in the event that an IVIG J-code is not found on the same claim as the IVIG items and services
payment code (Q-code), or in claims history in the previous 30 days. If a J-code is not found on the
same claim as the Q-code, the claims processing system will recycle the Q-code claim for the IVIG
items and services associated with the administration of the IVIG product (J-code), until a claim
containing the J-code for IVIG product is received in the CWF. The home IVIG items and services
claim will recycle three times (with a 30-day look back period) for a total of 15 business days. After
15 business days, if no J-code claim is found in claims history, the Q-code claim will be denied.
Suppliers must ensure that an eligible J-code (as indicated on L33610) associated with the visit is
billed with the visit or no more than 30 days prior to the visit. Visits are denied if an eligible J-code
for the visit is not billed. Claims reporting multiple visits on the same line item date of service will
be returned as unprocessable.
220 - Appeals
(Rev. 1, 10-01-03)
See chapter 29 for a description of the appeals process.
230 - DME MAC Systems
(Rev. 629, Issued: 07-29-05; Effective: 01-01-06; Implementation: 01-03-06)
The VMS shall allow the DME MACs the flexibility to report CMN edits as medical
review or claims processing workload.
300 - New Systems Requirements
(Rev. 166, 4-30-04)
The DME MAC systems have the capability to turn off the remit switch when sending a
remittance notice is not appropriate (e.g. when the beneficiary has submitted a claim).

Transmittals Issued for this Chapter
Rev # Issue Date Subject Impl Date CR#
R12557CP
03/28/2024
Updates to Pub. 100-04 Claims Processing
Manual, Chapter 20, Section 181.1 Payment
for Lymphedema Compression Treatment
Items
04/29/2024
13528
R12471CP
01/24/2024
Implementation of New Benefit Category for
Lymphedema Compression Treatment Items
01/02/2024
13286
R12437CP
12/28/2023
Implementation of the New Home
Intravenous Immune Globulin (IVIG) Items
and Services Payment
01/02/2024
13217
R12423CP
12/20/2023
Enforcing Billing Requirements for Intensive
Outpatient Program (IOP) Services with New
Condition Code 92
01/02/2024
13222
R12379CP
11/22/2023
Implementation of New Benefit Category for
Lymphedema Compression Treatment Items-
Rescinded and replaced by transmittal 12471
01/02/2024
13286
R12359CP
11/09/2023
Implementation of New Benefit Category for
Lymphedema Compression Treatment Items-
Rescinded and replaced by transmittal 12379
01/02/2024
13286
09/14/2023
Implementation of the New Home
Intravenous Immune Globulin (IVIG) Items
and Services Payment- Rescinded and
replaced by transmittal-12437
01/02/2024
13217
07/28/2023
Implementation of New Benefit Category for
Lymphedema Compression Treatment Items-
SENSITIVE CONTROVERSIAL-
Rescinded and replaced by transmittal
12359/ NO LONGER SENSITIVE
01/02/2024
13286
07/21/2023
Implementation of the New Home
Intravenous Immune Globulin (IVIG) Items
and Services Payment- SENSITIVE
CONTROVERSIAL- Rescinded and
replaced by transmittal 12252
01/02/2024
13217
R12013CP
05/02/2023
Inflation Reduction Act Section 11407:
Limitations on Monthly Coinsurance and
Adjustments to Supplier Payment Under
Medicare Part B for Insulin Furnished
Through Durable Medical Equipment (DME)
– IMPLEMENTATION
07/03/2023
13014

Rev # Issue Date Subject Impl Date CR#
R11917CP
03/21/2023
Inflation Reduction Act Section 11407:
Limitations on Monthly Coinsurance and
Adjustments to Supplier Payment Under
Medicare Part B for Insulin Furnished
Through Durable Medical Equipment (DME)
– IMPLEMENTATION - Rescinded and
replaced by transmittal12013
07/03/2023
13014
R11834CP
02/02/2023
Inflation Reduction Act Section 11407:
Limitations on Monthly Coinsurance and
Adjustments to Supplier Payment Under
Medicare Part B for Insulin Furnished
Through Durable Medical Equipment (DME)
– IMPLEMENTATION
NO LONGER SENSITIVE- Rescinded and
replaced by transmittal11917
07/03/2023
13014
R11429CP
05/23/2022 Revisions to National Coverage
Determination (NCD) 240.2 (Home Use of
Oxygen) and 240.2.2 (Home Oxygen Use for
Cluster Headache)
01/03/2023
12607
R11414CP
05/12/2022 Claims Processing Manual Update - Pub.
100.04 for Elimination of Certificates of
Medical Necessity (CMNs) and Durable
Medical Equipment Forms (DIFs)
06/13/2022
12734
R11263CP
02/10/2022 Revisions to National Coverage
Determination (NCD) 240.2 (Home Use of
Oxygen) and 240.2.2 (Home Oxygen Use for
Cluster Headache)- Rescinded and replaced
by transmittal 11429
06/14/2022
12607
R10840CP
06/11/2021 Updates to the Internet Only Publication
100-04, Chapter 1, Section 10.1 and Chapter
20, Section 10
07/12/2021
12310
R10236CP
07/31/2020 Update to the IOM Publication (Pub) 100-
04,
Medicare Claims Processing Manual,
Chapters 1, 6, 8, 17, 20, 22, 24, and 31
Referencing the Active Universal Resource
Locators (URLs) for the Washington
Publishing Company (WPC) and the ASC
X12 Organizations, and Updates to the
08/31/2020
11857

Rev # Issue Date Subject Impl Date CR#
HIPAA Eligibility Transaction System
(HETS)
12/20/2019 Manual Update to Publication (Pub.) 100-
04,
Chapter 20, to Revise the Subsection 10 -
Where to Bill Durable Medical Equipment,
Prosthetics, Orthotics, and Supplies
(DMEPOS) and Parenteral and Enteral
Nutrition (PEN) Items and Services
03/23/2020
11554
R4202CP 01/18/2019 Update to Pub. 100-04 Chapters 8, 20, and
24 to Provide Language-Only Changes for
the New Medicare Card Project
02/19/2019
10964
R4112CP 11/01/2018 Temporary Transitional Payment for Home
Infusion Therapy Services for CYs 2019 and
2020
01/07/2019
10836
R4052CP 05/17/2018 Removal of KH Modifier from Capped
Rental Claims
10/01/2018
10422
R4037CP 04/27/2018 Removal of KH Modifier from Capped
Rental Claims - Rescinded and replaced by
transmittal 4052
10/01/2018
10422
R4027CP 04/27/2018 Inexpensive or Routinely Purchased Durable
Medical Equipment (DME) Payment
Classification for Speech Generating Devices
(SGD) and Accessories
10/01/2018
10604
R4001CP 03/16/2018 Internet Only Manual Updates to Pub. 100-
01, 100-02 and 100-04 to Correct Errors and
Omissions (SNF) (2018)
06/19/2018
10512
R3895CP 10/27/2017 Revised and New Modifiers for Oxygen
Flow Rate
04/02/2018
10158
R3824CP 08/02/2017 July Quarterly Update for 2017 Durable
Medical Equipment, Prosthetics, Orthotics,
and Supplies (DMEPOS) Fee Schedule
07/03/2017
10071

Rev # Issue Date Subject Impl Date CR#
R3801CP 06/28/2017 Extension of the Transition to the Fully
Adjusted Durable Medical Equipment,
Prosthetics, Orthotics and Supplies Payment
Rates under Section 16007 of the 21st
Century Cures Act
07/03/2017
9968
R3730CP 03/03/2017 Payment for Oxygen Volume Adjustments
and Portable Oxygen Equipment
04/03/2017
9848
R3716CP 02/10/2017 Extension of the Transition to the Fully
Adjusted Durable Medical Equipment,
Prosthetics, Orthotics and Supplies Payment
Rates under Section 16007 of the 21st
Century Cures Act – Rescinded and replaced
by transmittal 3801
07/03/2017
9968
R3713CP 02/03/2017 Extension of Payment Change for Group 3
Complex Rehabilitative Power Wheelchairs
Accessories and Seat and Back Cushions
under Section 16005 of the 21st Century
Cures Act
07/03/2017
9966
R3679CP 12/16/2016 Payment for Oxygen Volume Adjustments
and Portable Oxygen Equipment -
Rescinded
and replaced by Transmittal 3730
04/03/2017
9848
R3649CP 11/10/2016 Payment for Oxygen Volume Adjustments
and Portable Oxygen Equipment –
Rescinded
and replaced by Transmittal 3679
04/03/2017
9848
R3593CP 08/17/2016 Durable Medical Equipment, Prosthetics,
Orthotics and Supplies (DMEPOS)
Competitive Bidding Program (CBP):
Additional Instructions for the
Implementation of Round 2 Recompete of
the DMEPOS CBP and National Mail Order
(NMO) Recompete
10/03/2016
9579
R3565CP 07/20/2016 Durable Medical Equipment, Prosthetics,
Orthotics and Supplies (DMEPOS)
Competitive Bidding Program (CBP):
Additional Instructions for the
10/03/2016
9579

Rev # Issue Date Subject Impl Date CR#
Implementation of Round 2 Recompete of
the DMEPOS CBP and National Mail Order
(NMO) Recompete –
Rescinded and replaced
by Transmittal 3593
R3535CP 07/07/2016 Payment Change for Group 3 Complex
Rehabilitative Power Wheelchairs
Accessories and Seat and Back Cushions
under Section 2 of the Patient Access and
Medicare Protection Act (PAMPA)
07/05/2016
9520
R3500CP 04/28/2016 Durable Medical Equipment, Prosthetics,
Orthotics and Supplies (DMEPOS)
Competitive Bidding Program (CBP):
Additional Instructions for the
Implementation of Round 2 Recompete of
the DMEPOS CBP and National Mail Order
(NMO) Recompete – Rescinded and replace
d
by Transmittal 3565
10/03/2016
9579
R3493CP 04/14/2016 Payment Change for Group 3 Complex
Rehabilitative Power Wheelchairs
Accessories and Seat and Back Cushions
under Section 2 of the Patient Access and
Medicare Protection Act (PAMPA) –
Rescinded and replaced by Transmittal 3535.
07/05/2016
9520
R3491CP 04/05/2016 Payment for Purchased Durable Medical
Equipment, Prosthetics, Orthotics, and
Supplies (DMEPOS) Furnished to Medicare
Beneficiaries Residing Outside the U.S. -
Expatriate Beneficiaries
07/05/2016
9468
R3459CP 02/05/2016 Payment Change for Group 3 Complex
Rehabilitative Power Wheelchairs
Accessories and Seat and Back Cushions
under Section 2 of the Patient Access and
Medicare Protection Act (PAMPA) –
Rescinded and replaced by Transmittal 3493.
07/05/2016
9520
R3444CP 01/29/2016 Payment for Purchased Durable Medical
Equipment, Prosthetics, Orthotics, and
Supplies (DMEPOS) Furnished to Medicare
07/05/2016
9468

Rev # Issue Date Subject Impl Date CR#
Beneficiaries Residing Outside the U.S. -
Expatriate Beneficiaries – Rescinded and
replaced by Transmittal 3491
R3443CP 01/29/2016 Manual Update to Pub. 100-04, Chapter 20,
to Include Used Rental Equipment
07/05/2016
9488
R3416CP 11/23/2015 CY 2016 Update for Durable Medical
Equipment, Prosthetics, Orthotics and
Supplies (DMEPOS) Fee Schedule
01/04/2016
9431
R3196CP 02/13/2015 Payment Repairs to Capped Rental
Equipment Prior to the End of the 13-Month
Cap
07/06/2015
9062
R2993CP 07/25/2014 Update to Pub. 100-04, Chapter 20 to
Provide Language-Only Changes for
Updating ICD-10 and ASC X12
08/25/2014
8694
R2977CP 06/20/2014 Clarification of Billing Instructions Related
to the Home Health Benefit
09/23/2014
8775
R2687CP 04/19/2013
Clarify the Definition of Customized Durable
Medical Equipment (DME) Items
07/19/2013
8194
R2629CP 01/04/2013 Updating the VMAP/4D Table with B5
Ocularist Specialty Code
02/05/2013
8123
R2605CP 11/30/2012 Transcutaneous Electrical Nerve Stimulation
(TENS) for Chronic Low Back Pain (CLBP)
01/07/2013
7836
R2511CP 08/03/2012 Transcutaneous Electrical Nerve Stimulation
(TENS) for Chronic Low Back Pain (CLBP)
– Rescinded and replaced by Transmittal
2605
01/07/2013
7836
R2487CP 06/08/2012 Internet Only Manual (IOM) Update for
Laboratory Services and Durable Medical
Equipment, Prosthetics, Orthotics, and
Supplies (DMEPOS) Claims Processed
06/19/2012
7749

Rev # Issue Date Subject Impl Date CR#
under the End Stage Renal Disease
Prospective Payment System (ESRD PPS)
R2475CP 05/18/2012 Internet Only Manual (IOM) Update for
Laboratory Services and Durable Medical
Equipment, Prosthetics, Orthotics, and
Supplies (DMEPOS) Claims Processed
under the End Stage Renal Disease
Prospective Payment System (ESRD PPS)
06/19/2012
7749
R2465CP 05/11/2012 Assigned Codes for Home Oxygen Use for
Cluster Headaches (CH) in a Clinical Trial
(ICD-10)
10/01/2012
7820
R2464CP 05/04/2012 Enhance the Multi-Carrier System (MCS)
and ViPS Medicare System (VMS) to
Maintain Five Full Years of Pricing Data and
to Automatically Price Claims/Adjustments
at the Rates in Effect at the Dates of Service
10/01/2012
for VMS
7383
R2299CP 09/08/2011 Enhance the Multi-Carrier System (MCS)
and ViPS Medicare System (VMS) to
Maintain Five Full Years of Pricing Data and
to Automatically Price Claims/Adjustments
at the Rates in Effect at the Dates of Service
– Rescinded and replaced by Transmittal
2464.
10/03/2011
7383
R2210CP 05/06/2011 Enhance the Multi-Carrier System (MCS)
and ViPS Medicare System (VMS) to
Maintain Five Full Years of Pricing Data and
to Automatically Price Claims/Adjustments
at the Rates in Effect at the Dates of Service
– Rescinded and replaced by Transmittal
2299
10/03/2011
7383
R1961CP 04/30/2010 Payment for Replacement of Oxygen
Equipment in Bankruptcy Situations
10/04/2010
6838
R1603CP 09/26/2008 Claims Jurisdiction and Enrollment
Procedures for Suppliers of Certain
Prosthetics, Durable Medical Equipment
10/27/2008
5917

Rev # Issue Date Subject Impl Date CR#
(DME) and Replacement Parts, Accessories
and Supplies
R1493CP 04/18/2008 Establish Pre-Payment Auto-denial Edits in
Applicable States for DMEPOS Suppliers of
Oxygen and Oxygen Equipment (DME
MACs only)
04/07/2008
5929
R1472CP 03/06/2008 Update of Institutional Claims References 04/07/2008
5893
R1421CP 01/25/2008 Update of Institutional Claims References -
Rescinded and Replaced by Transmittal 1472
04/07/2008
5893
R1378CP 11/23/2008 Establish Pre-Payment Auto-denial Edits in
Applicable States for DMEPOS Suppliers of
Oxygen and Oxygen Equipment (DME
MACs only) – Replaced by Transmittal 1493
04/07/2008
5471
R1368CP 11/02/2007 Reporting an NPI and the “EY” Modifier on
Claims for DMEPOS Items Dispensed
Without a Physician’s Order to Obtain a
Medicare Denial for Coordination of
Benefits (COB)
04/07/2008
5771
R1142CP 12/22/2006 DMERC Claim Modifiers for Upgrades 04/02/2007
5367
R961CP 05/26/2006 Home Use of Oxygen in Approved Clinical
Trials
10/03/2006
4389
R867CP 02/17/2006 Elimination of the DMERC Information
Form (DIF)
04/03/2006
4241
R863CP 02/17/2006 Update to Chapter 20, “Billing for Oxygen
and Oxygen Equipment”, Section 130.6
03/17/2006
4271
R745CP 11/04/2005 Elimination of the DMERC Information
Form (DIF)
04/03/2006
4040
R656CP 08/19/2005 Full Replacement of CR 3607, Payment
Edits in Applicable States for DMEPOS
Suppliers of Prosthetics and Certain Custom-
10/03/2005
3959

Rev # Issue Date Subject Impl Date CR#
Fabricated Orthotics, Change Request 3607
is Rescinded (DMERC Only)
R629CP 07/29/2005 Certificate of Medical Necessity Claim Edits
Workload Reporting
01/03/2006
3699
R546CP 04/29/2005 Number of DMEPOS Pricing Files That
Must be Maintained Online for Medicare-
DMERC, FI and RHHI Only
10/03/2005
3792
R489CP 03/04/2005
Correction to Healthcare Common Procedure
Coding System (HCPCS) Code A4217
07/05/2005
3714
R445CP 01/21/2005 Payment to Providers/Suppliers Qualified to
Bill Medicare for Prosthetics and Certain
Custom Fabricated Orthotics
07/05/2005
3607
R330CP 10/22/2004 DMERC-Beneficiary Submitted Claims,
Process First Claim
04/04/2005
3233
R329CP 10/22/2004 DMERC Only-Payment to
Providers/Suppliers Qualified to Bill
Medicare for Prosthetics and Certain Custom
Fabricated Orthotics
07/05/2005
3373
R284CP 08/27/2004 DMERCs Only-Appeals of Duplicate Claims
09/27/2004
3371
R236CP 07/23/2004 2005 DMEPOS Pricing File Record Layout 01/03/2005
3300
R222CP 07/02/2004 Skilled Nursing Facility Consolidated
Billing-New Requirements for Claims for
DMEPOS
N/A 2453
R166CP 04/30/2004 New Systems Requirements 10/04/2004
2761
R001CP 10/01/2003 Initial Release of Manual N/A N/A
Back to top of chapter
