
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 2
T ABLE OF CONT ENT S
Introduction ............................................................................................................................. 9
Overview 9
Vision and Goals 10
Provider Requirements............................................................................................................11
Overview 11
Designated HCBS Provider Attestation 11
Designation 12
Re-Designation 13
De-Designation 13
Medicaid Enrollment 14
Electronic Visit Verification (EVV) 14
CMS Final Rule on HCBS Settings 16
Background and Overview 16
DOH Compliance Process 16
HCBS Settings Rule Resources 17
Consolidated Fiscal Report 17
Criminal History, Background Checks, and Training Requirements 17
Required Clearances 17
Mandated Reporter Requirements 18
Training Requirements 18
Attestation for Foreign Education Documents 19
HCBS Eligibility and Enrollment ...............................................................................................19
Overview 19
NOTICE OF DECISION 22
Expectations for the Completion of NOD – Enrollment or Denial 23
Expectations for the Completion of NOD – Discontinuance 23
Additional Reasons for NOD Forms 24
Fair Hearing 24
HCBS Eligibility Reauthorization 25
Participant Placed in an HCBS Restricted Setting 26
Capacity Management 26
Capacity Management Process 26
Capacity Tracker/Waitlist 27
HCBS Disenrollment................................................................................................................27

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 3
Overview 27
Disenrollment Process 28
Discharge from HCBS Process 29
Care Management and Monitoring Access to Care for HCBS......................................................29
Care Management 30
Monitoring Access to Care 31
Person-Centered Plan of Care ..................................................................................................32
Plan of Care (POC) Development 32
Development of the POC and Referrals for HCBS 33
HCBS Service Plan 33
Components of a HCBS Service Plan 34
Expectations for the Development of a HCBS Service Plan 35
Plan of Care Workflow 36
Participants Rights and Protections .........................................................................................36
Overview 36
Freedom of Choice 36
Incident Reporting 37
Grievances and Complaints 38
Conflict Free Case Management 38
Quality Monitoring and Oversight 39
Annual Children’s Waiver Case Review and Audit 39
Billing and coding for HCBS ....................................................................................................40
Overview 40
Fundamental Requirements 40
Provider Designation to Deliver Services 40
Services that Do Not Require State Designation 41
Medicaid-Enrolled Provider 41
Medicaid Managed Care Plan Contracting 41
Rates 42
Government Rates 42
Productivity Adjustment 42
Regions 42
Claims 42
General Claim Requirements 42
Enrollment Status 43
Medicaid Fee-For-Service Claiming (eMedNY) 43

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 4
Medicaid Managed Care Plan Claiming 43
Services Included in or Excluded from Capitation Payments to Medicaid Managed Care
Plans 44
Third-Party Health Insurance Denials 45
Services Delivered by Multiple Staff Members 45
Multiple Services Provided on the Same Date to the Same Child/Youth 46
Services Provided During School/Day Time 46
Services Provided While in Transit 46
Out of State Services 47
Submitting Claims for Services When the Child/Youth Is Not Present 47
Submitting Claims for Non-Sequential Time for the Same Service, on the Same Day....... 48
Timed Units per Encounter of Service 48
Submitting Claims for Daily Billed Services 48
Claims Coding 48
Claims Testing 49
Service Combinations 49
Provider Assistance 49
Where to submit questions and complAints..............................................................................49
Service Definitions ..................................................................................................................50
Overview 50
Community Habilitation 51
Definition 51
Service Components 52
Provider and Condition Requirements 52
Modality 53
Setting 54
Limitations/Exclusions 54
Certification/Provider Qualifications 54
Training Requirements 55
Service Billing Details 56
Guidelines for Medical Necessity Criteria for Children, Adolescents, and Young Adults .... 57
Day Habilitation 61
Definition 61
Service Components 61

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 5
Modality 61
Setting 61
Limitations/Exclusions 62
Certification/Provider Qualifications 62
Training Requirements 64
Service Billing Details 64
Caregiver/Family Advocacy and Support Services 65
Definition 65
Service Components 66
Modality 67
Setting 67
Limitations/Exclusions 67
Certification/Provider Qualifications 67
Training Requirements 68
Service Billing Details 69
Respite 70
Definition 70
Service Components 70
Modality 71
Setting 72
Limitations/Exclusions 73
Certification/Provider Qualifications 73
Training Requirements 75
Service Billing Details 75
Prevocational Services 78
Definition 78
Service Components 78
Modality 79
Setting 79
Limitations/Exclusions 79
Certification/Provider Qualifications 79
Training Requirements 80
Service Billing Details 81
Supported Employment 82

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 6
Definition 82
Service Components 82
Modality 83
Setting 83
Limitations/Exclusions 83
Certification/Provider Qualifications 84
Training Requirements 85
Service Billing Details 85
Palliative Care – Expressive Therapy 86
Definition 86
Modality 87
Setting 87
Limitations/Exclusions 87
Certification/Provider Qualifications 87
Training Requirements 89
Service Billing Details 89
Palliative Care – Massage Therapy 90
Definition 90
Service Components 90
Modality 90
Setting 91
Limitations/Exclusions 91
Certification/Provider Qualifications 91
Training Requirements 92
Service Billing Details 92
Palliative Care – Counseling and Support Services 93
Definition 93
Modality 95
Setting 95
Limitations/Exclusions 95
Certification/Provider Qualifications 95
Training Requirements 96
Service Billing Details 96
Palliative Care – Pain and Symptom Management 98

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 7
Definition 98
Service Components 99
Modality 99
Setting 99
Limitations/Exclusions 99
Certification/Provider Qualifications 99
Training Requirements 100
Service Billing Details 101
Adaptive and Assistive Technology 102
Definition 102
Service Components 102
Modality 103
Limitations/Exclusions 103
Certification/ Provider Qualifications 104
Service Billing Details 105
Vehicle Modifications 106
Definition 106
Service Components 106
Modality 107
Limitations/Exclusions 107
Certification/Provider Qualifications 108
Service Billing Details 109
Environmental Modifications 110
Definition 110
Service Components 110
Modality 111
Limitations/Exclusions 111
Certification/Provider Qualifications 112
Service Billing Details 113
Non-Medical Transportation 114
Definition 114
Service Components 114
Limitations/Exclusions 114
Certification/Provider Qualifications 115

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 8
Roles Related to a Participant’s Access to Non-Medical Transportation 115
Service Billing Details 117
Appendices .......................................................................................................................... 118
Appendix A: Glossary of Key Terms 118
Appendix B: CMS Final Rule on HCBS Settings 125
Appendix C: Prior/Concurrent Authorization Grid 129
Appendix D: Utilization Management/medical Necessity Guidelines for Children’s Aligned Home and
COmmunity Based services 131
Appendix E: Table of Responsibilities for HCBS Workflow 132
Appendix F: Training Grid 133
Appendix G: Service Animal Guidance 135
Appendix H: Medicaid Eligibility Guidance 139
Medicaid Eligibility Status Impact on HCBS Eligible Children 139
Process for Renewing and Establishing Medicaid for Children’s Waiver Participants143
Medicaid Excess/Surplus Income (Spenddown) Program Guidance for Children’s Care
Management and HCBS 145
Appendix I: HCBS LOC Eligibility Guidance 148
Care Management Requirements for HCBS Eligible Children 148
Requirements Regarding the Children’s Waiver HCBS Participants Placed in a Restricted
Setting 151
HCBS Determination for Children Discharging from OMH Residential Treatment Facility or
Psychiatric Center 152
Appendix J: Health Home Serving Children Policy Information 157
Appendix K: Waiver Performance Measures 158
Appendix L: K-Codes RR/E for the Children’s Waiver 161
Appendix M: Billing and Claiming Resources 162
Appendix N: Allowable Billing Combinations 163

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 9
INT RODUCT ION
OVERVIEW
Home and Community Based Services (HCBS) are designed to allow children and
youth to participate in developmentally and culturally appropriate services through
Medicaid. New York State (NYS) is committed to serving individuals in the least
restrictive environment possible by providing services and supports to children/youth
and their families at home and in the community.
The Children’s Medicaid System Transformation for individuals under the age of 21
includes the alignment of the following NYS children’s waivers previously accessible
under the authority of the 1915(c) amendment of the Federal Social Security Act: Office
of Children and Family Services (OCFS) Bridges to Health (B2H) Serious Emotional
Disturbance (SED), B2H Developmental Disabilities (DD), B2H Medically Fragile
(MedF), the Office of Mental Health (OMH) SED Waiver, Office for People With
Developmental Disabilities (OPWDD) Care at Home (CAH) IV Waiver, and the
Department of Health (DOH) operated Care at Home (CAH) I/II Waiver.
The Office of Addiction Services and Supports (OASAS), OCFS, OMH, OPWDD, and
DOH have collaborated to create an aligned service array of HCBS benefits for children
meeting specific diagnostic and functional criteria. The 1915(c) Children’s Waiver and
1115 Medicaid Redesign Team (MRT) Waiver, with approval from the Centers for
Medicare and Medicaid Services (CMS) in 2019, provides NYS the authority for these
HCBS benefits. The waiver includes person-centered planning requirements and
specifies transitional coverage requirements for children/youth enrolled in any of the
aforementioned 1915(c) waivers at the time of transition.
HCBS are designed for children/youth who, if not receiving these services, would require the
level of care provided in a more restrictive environment such as a long-term care facility or
psychiatric inpatient care, as well as children/youth stepping down from a long-term care
facility or psychiatric inpatient care.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 10
This Manual defines the specific composition of each service while outlining provider
roles and responsibilities. Additionally, it is a reference tool for Health Homes (HH),
Health Home Care Managers (HHCM), HCBS Providers, Medicaid Managed Care
Plans (MMCPs), and the State’s Independent Entity of Children and Youth Evaluation
Services (C-YES) regarding care management, the service delivery system, and
Medicaid eligibility determination and impact to service delivery. All HCBS benefits are
applicable in any home or community setting meeting federal HCBS settings
requirements inclusive of the child/youth or family environment, with some exceptions
noted in this Manual.
This Manual also provides an outline of performance measures that are pertinent to the
HHCM/C-YES and HCBS Providers (see Appendix J. The performance measures noted
in the Appendix J are not inclusive of all performance measures required by the
Children’s Waiver. For a full list of all required reporting measures, please see the most
up to date Children’s Waiver amendment.
Vision and Goals
HCBS are designed to offer support and services to children/youth in non-
institutionalized settings that enable them to remain at home and in the community or
for children/youth being discharged from an institutional setting who require these
services to safely return to their home and community. HCBS provides a family-driven,
youth-guided, culturally and linguistically appropriate system of care that accounts for
the strengths, preferences, and needs of the individual, as well as the desired outcome.
Services are individualized to meet the physical health, developmental, and behavioral
health needs of each child/youth. Participants have independent choice among an array
of service options and providers. These services are provided in a flexible,
complimentary package that evolves over time to meet the changing needs of the
child/youth.
HCBS/Level of Care Eligibility Determination includes:
1) Target Population (TP) criteria,
2) Risk factors (for some TP),
3) Functional criteria, and
4) Medicaid eligibility.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 11
HCBS are intended to be provided to a
child/youth and family in their home
and/or the community. The array of
services is intended to assist
children/youth in being successful at
home, in school, and in their other
natural environments to help maintain
them in their community and avoid
higher levels of care and out-of-home
placements.
PROVIDER REQUIREMENT S
Overview
Service providers delivering Children’s Home and Community Based Services (HCBS)
must meet the following requirements:
• Be a qualified provider as described in this Children’s Home and Community
Based Services Manual and any subsequent updates
• Be in good standing according to the standards of each agency by which it is
licensed, certified, designated, or approved
• Possess, acquire, and retain any State licensure, certification, authorization, or
credential when required
• Be a fiscally viable agency and maintain fiscal integrity
• Be enrolled as a NY Medicaid Provider with an active provider identification
number prior to commencing service delivery
• Submit an application to and be designated by the NYS Children’s Provider
Designation Review Team
• Have appropriate agreements in place for any outsourced administrative
functions, if applicable
• Be compliant with the HCBS Settings Rule
• Have at least one contract with a Medicaid Managed Care Plan
• Sign and be compliant with the Children’s HCBS Provider Designation Attestation
Designated HCBS Provider Attestation
The Children’s Waiver requires provider designation to be renewed at least every three
years. Providers will be required to complete the Designated Home and Community
Based Services (HCBS) Provider Attestation as part of the re-designation process to
confirm they are familiar with the requirements of the Children’s Waiver and will adhere
to the standards, policies, procedures, and guidance put forth by NYS regarding the
HCBS Children’s Waiver.
It is the mission of NYS and its child and
family serving agencies to improve health
and behavioral health care access and
outcomes for individuals served while
demonstrating sound stewardship of
financial resources.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 12
Newly designated providers must complete the Designated Home and Community
Based Services (HCBS) Provider Attestation and return it to the NYS Children’s
Provider Designation Interagency Review Team within 30 days of receipt. If the
provider’s designation is altered (i.e. added/removed site(s), service(s), etc.), an
updated Provider Attestation is not required. Providers must adhere to all requirements
outlined in the attestation regardless of any designation alterations, unless the
alterations result in a de-designation from all HCBS.
Designation
The Children’s Designation process is a multi-State agency process that includes OMH,
DOH, OASAS, OCFS, and OPWDD (i.e., the NYS Children’s Provider Designation
Interagency Review Team). These agencies provide guidance to providers who intend
to become NYS HCBS providers serving children/youth under the 1915(c) Children’s
Waiver.
Any service provider delivering HCBS must be designated to do so by the NYS
Children’s Provider Designation Interagency Review Team. To become designated, the
provider:
NYS will initially verify provider designation status through the web-based online portal
system, assuring providers are approved and active before they are authorized to
1. Must meet the qualifications as outlined in this Manual and be identified
as a child serving agency or agency with children’s behavioral health and
health experience and;
2. Be an OMH, OASAS, OCFS, DOH, or OPWDD provider, that is
licensed, certified, designated, and/or approved by OMH, OASAS, OCFS,
OPWDD, or DOH or its designee to provide comparable and appropriate
services referenced in the service definition or;
3. Who are not currently licensed, designated, or certified by any of the
State agencies must follow the Designation Policy for Non-Licensed/Non-
Certified Providers.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 13
provide waiver services. Provider designation will be recertified at least every three
years and at the discretion of DOH. Additional information on provider designation can
be found in the HCBS Provider Designation and Re-designation Procedure.
Information on gaining access to the Children’s Waiver Provider Designation online
application is available within the Obtaining Access to the New York State Children and
Family Treatment and Supports Services (CFTSS)/HCBS Designation Application.
HHs are also designated and re-designated by NYS and must adhere to the Health
Home Standards and Requirements.
Re-Designation
The 1915(c) Children’s Waiver requires that provider designation is reverified at least
every three years. Designated providers must comply with State requests for
information to confirm compliance with Children’s HCBS designation. Re-designation for
currently designated providers is a State-led process. The State will notify designated
providers when they are required to re-designate as a provider of Children’s HCBS.
Providers that have been de-designated but wish to become re-designated as a
Children’s HCBS provider must complete a Children’s HCBS Provider Designation
application. Once the re-designation application has been reviewed, the provider will
receive a Children’s HCBS Re-Designation Letter that indicates approved services by
site. Re-designated agencies will also be required to complete the Designated Home
and Community Based Services (HCBS) Provider Attestation and return it to the NYS
Children’s Provider Designation Interagency Review Team within 30 days of receipt.
De-Designation
When an agency has made a decision to de-designate from a service, site, or county, a
formal request must be submitted in writing to the NYS Children’s Provider Designation
Interagency Team at (OMH-Childrens-Designation@omh.ny.gov).
New York State can also decide to de-designate an agency providing HCBS for some
services or all services due to non-compliance to the attestations, policies, procedures,
and/or claiming requirements.
If an HCBS provider determines to de-designate, they must notify the NYS Children’s
Provider Designation Interagency Team and establish a transition plan for any and all
children/youth being provided services. De-designation cannot occur until all
children/youth receiving services from the agency have been fully transitioned to

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 14
another designated service provider or no longer require services as determined in
collaboration with the child/youth’s HHCM/C-YES. De-designation would occur only
after the NYS Children’s Provider Designation Interagency Team has confirmed that the
affected children/youth enrolled with the agency have been appropriately transitioned.
Participation in State-led annual case reviews and submission of all required reporting
documents remain requirements for providers that have provided services within the
review period (i.e., Waiver year), even if the provider has been de-designated.
Medicaid Enrollment
Prior to the delivery of HCBS, providers must be Medicaid enrolled. Providers who are
not already Medicaid enrolled must complete the NY Medicaid Provider Enrollment
Form.
Each provider delivering these services must be enrolled as a Medicaid provider with an
active provider identification number and Category of Service (COS): 0268. A list of
provider types and the application can be found on the eMedNY website; questions can
also be directed to the eMedNY Call Center at 1-800-343-9000.
Electronic Visit Verification (EVV)
All Providers and Fiscal Intermediaries (FIs) who provide Medicaid Personal Care
Services (PCS) and Home Health Care Services (HHCS) are required to utilize an EVV
system to capture services that begin or end in the consumer’s home. EVV applies to
both Fee-for Service (FFS) and Medicaid Managed Care (MMC) services.
The federal 21
st
Century Cures Act, signed into law on December 13, 2016, requires all
state Medicaid programs to implement an EVV system for PCS by January 1, 2021 and
HHCS by January 1, 2023. As such, DOH required providers of Medicaid-funded PCS
to select and implement compliant EVV systems that meet the requirements of the 21st
For more information
Refer to the Children’s HCBS Provider Designation and Re-designation Procedure.
For more information
Regarding the process for provider initiated and state initiated de-designation can be
found in the HCBS Children’s De-Designation Procedure.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 15
Century Cures Act by January 1, 2021. Providers of Medicaid-funded HHCS will be
required to select and implement compliant EVV systems by January 1, 2023.
For the Children’s Waiver, EVV requirements ALWAYS apply to Community Habilitation
and MAY apply to Respite services. EVV requirements do not apply to Day Habilitation.
Children’s HCBS providers that are designated or want to be designated for Community
Habilitation and or Respite services must self-assess as to whether they meet the EVV
criteria and, if necessary, take steps internally to become EVV compliant. Children’s
Waiver HCBS providers that might also serve the OPWDD Waiver will need to comply
also with OPWDD Guidance.
After self-assessment, some HCBS Respite providers will determine that they do not
meet EVV requirements for any of the HCBS-enrolled children/youth they serve, while
other HCBS Respite providers may meet the EVV requirement for some or all of the
enrolled children/youth they serve.
Since EVV may be applicable to Planned and Crisis Respite, Respite providers must
complete the Children’s Waiver EVV Declaration Form to confirm they understand the
EVV requirements and have determined if they meet EVV requirements. All Planned
and Crisis Respite that meet EVV, AND all Community Habilitation providers, will be
required to complete an EVV Attestation via eMedNY ensuring they have obtained the
appropriate systems for Electronic Verification.
Additional Information can be found in the following guidance and policies:
• EVV Section on DOH Website
• EVV Program Guidelines and Requirements: provides an overview of the
NYS EVV Program, providers that are subject to EVV, program and policy
requirements, technical system requirements, and steps on how to begin
working with DOH
• Considerations for Selecting an EVV System
• State's Model Choice for EVV: letter submitted to the Centers for Medicare
and Medicaid Services (CMS) on April 10, 2020 describing NYS progress
towards implementation
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 16
CMS Final Rule on HCBS Settings
Background and Overview
In 2014, Centers for Medicare & Medicaid Services (CMS) published new requirements
that settings where children/youth receive HCBS must meet to remain eligible for
Medicaid payment. These updated standards are designed to ensure these settings
protect the rights and choices of children/youth receiving HCBS and promote integration
in and full access to the community. By design, HCBS are provided in home and
community-based settings; for this reason, HCBS providers are required to demonstrate
compliance with these standards (see Appendix B for the detailed standards).
DOH Compliance Process
DOH assesses compliance with HCBS settings requirements for both existing
designated providers and those seeking designation.
All designated Children’s Waiver HCBS providers will need to be in compliance with the
settings requirements of the Final Rule by March 17, 2023. For current sites the State
believes overcome the presumption of institutionalization and meet the requirements of
the Final Rule, the State will submit to CMS information or documentation ensuring all
individuals served in that setting are afforded the degree of community integration
required by the Final Rule. Sites that are not able to come into compliance by this date
will be de-designated as a Children’s Waiver HCBS provider.
Additionally, during the annual case review and audit, HCBS providers will be
continually monitored to ensure continued compliance with the Final Rule, including
person-centered service planning and freedom of choice for participants.
For new providers seeking designation to provide HCBS, NYS will conduct a review of
the provider to ensure compliance with the HCBS Settings Rule through the following
steps:
• Provider self-assessment
• Documentation review of policies/procedures
• Potential site visit
For more information
For designated HCBS providers can be found in the March 8, 2019 NYS memo
Medicaid Provider Enrollment for Individual Practitioners and Designated Agencies

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 17
HCBS Settings Rule Resources
Please refer to Appendix B and the DOH website for more information about the CMS
Final Rule. CMS also has an HCBS Requirements Compliance Toolkit.
Consolidated Fiscal Report
The Consolidated Fiscal Report (CFR) is a standardized reporting method accepted by
state agencies (OASAS, OMH, OPWDD, SED, DOH and OCFS), consisting of
schedules which, in different combinations, capture financial information for budgets,
quarterly and/or mid-year claims, an annual cost report, and a final claim.
HCBS Designated provider agencies must submit an annual Consolidated Fiscal Report
(CFR) following the guidelines provided in the CFR Manual. HCBS is reported on the
CFR under the auspices of DOH.
Criminal History, Background Checks, and T raining Requirements
Required Clearances
The 2018-2019 Enacted Budget includes statutory requirements (Chapter 57 Laws of
2018) related to criminal history record checks, mandated reporter requirements,
Statewide Central Register Database checks, and Staff Exclusion List checks for
HHCMs and children’s HCBS providers. The statute requires that HHs and Care
Management Agencies (CMA) that provide care management to enrollees under age 21
and HCBS providers authorized under the 1915(c) Children’s Waiver conduct the
following on prospective employees:
1. Staff Exclusion List (SEL) through the NYS Justice Center for the
Protection of People with Special Needs (Justice Center)
The SEL is a Statewide Register maintained by the NYS Justice Center. The
SEL contains the names of people found responsible for serious or repeated acts
of abuse and neglect. The SEL check is required for all newly hired staff that will
have regular and substantial contact with individuals under the age of 21. The
SEL should be completed prior to all other required background checks f or
practical purposes.
2. Criminal History Record Checks (CHRC) through DOH
The CHRC is a fingerprint-based, national FBI criminal history record check.
CHRC is required for HCBS provider employees who provide direct care to
members under the age of 21 (with limited exceptions). A provider must
immediately, but no later than 30 calendar days after the event, notify DOH
when:
• an individual is subject to CHRC via 103 submission and

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 18
• an individual is no longer subject to CHRC via 105 termination
o Terminations include when an employee is no longer subject to
CHRC; is no longer employed by the provider; employee death; or
when a prospective employee is no longer being considered by the
provider.
Upon receipt of the request for fingerprint (LiveScan), an appointment must be
scheduled for the employee to be fingerprinted, along with indication of the
method of payment.
3. Statewide Central Register (SCR) Database Check through OCFS
The SCR maintains a database of records of child abuse and maltreatment
reports. The purpose of the Database Check is to find out if a prospective
employee of a HCBS provider is a confirmed subject of an indicated report of
child abuse or maltreatment. The SCR Database Check is required for those
employees that will have regular and substantial contact with members, which
includes but is not limited to HCBS providers.
Please refer to the Background Check Requirements for HCBS Providers policy for
more details on scope, timeline, potential exemptions, and processes for each of these
three types of clearances.
Mandated Reporter Requirements
HCBS providers and other applicable agency employees are mandated to report
suspected child abuse or maltreatment, per NYS Social Services Law 413.
OCFS has information and registration links for free Mandated Reporter Training
available on its website.
Training Requirements
The HCBS provider Human Resources staff must receive training on these
requirements to ensure that staff receive the appropriate required clearances and to
ensure that the HCBS provider is in compliance.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 19
Each HCBS provider agency must maintain
documentation indicating that all staff who
provided HCBS during the Waiver Year
(including those staff no longer employed by
the agency) meet all training, qualifications,
and required employment check
requirements based upon the designation of
the agency and the service provided by the
staff member. Designated HCBS provider
agencies will be required to submit proof of this documentation to the State on at least
an annual basis.
Attestation for Foreign Education Documents
HCBS designated provider agencies that employ staff who have obtained their
education outside the United States must complete the Use of Foreign Education
Documents to Verify HCBS Staff Qualification Requirements attestation for each
applicable staff member. This attestation should be kept in the employee’s file along
with a copy of the relevant documentation.
HCBS ELIGIBILIT Y AND ENROLLMENT
Overview
To receive HCBS under Medicaid, a child/youth must be determined eligible based on
meeting Target Population, risk factors, if applicable, and functional criteria measured
by the HCBS/LOC Eligibility Determination. Only HHCMs or C-YES can determine
HCBS/LOC Eligibility Determination; for some Target Populations, the assistance from
the OPWDD DDRO is necessary for the HCBS/LOC eligibility determination.
Children/youth receiving HCBS through enrollment in a 1915(c) Medicaid Children’s
Waiver will have continued access to HCBS for as long as the child/youth continues to
meet the eligibility criteria for the 1915(c) Medicaid Children’s Waiver as listed below.
Children/youth who are eligible and appropriate for HCBS must have a physical health,
developmental disability, and/or mental health diagnosis with related significant needs
that place them at risk of hospitalization or institutionalization, or that HCBS is needed
for the child/youth to return safely home and to their community from a higher level of
care. (Institutionalization refers to children/youth at risk of being admitted to a higher
level of care such as out-of-home residential settings, hospitalization, ICF-I/ID, or
nursing facility).
This information is required to be
reported to NYS DOH as part of
the waiver annual case review and
audit to meet performance
measures within the Children’s
Waiver and reported to CMS.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 20
Children and youth must be under 21 years old and eligible for Medicaid to receive
Children’s HCBS. Children’s HCBS eligibility is comprised of three components: 1)
target criteria, 2) risk factors, if applicable, and 3) functional criteria.
The HCBS eligibility groups are as follows:
Level of Care (LOC): children/youth that meet institutional placement criteria.
There are four subgroups for children/youth within the LOC group:
The services described in this document are accessible to eligible children/youth once a
Plan of Care (POC) is in place. Further information regarding the POC can be found in
the Children’s HCBS POC Workflow Policy.
To access Children’s HCBS, a child/youth must meet LOC criteria (target criteria, risk
factors, if applicable, and functional limits) using the HCBS/LOC Eligibility Determination
which is housed within the Uniform Assessment System (UAS) along with the Child and
Adolescent Needs and Strengths – NY (CANS-NY) assessment. Only a HHCM, C-YES,
or the OPWDD Developmental Disabilities Regional Office (DDRO; refer to the DDRO
Manual for Children’s Waiver for additional information) are given access in the UAS to
complete the HCBS/LOC Eligibility Determination. During this evaluation and
assessment, the care manager must maintain regular contact with the child/family.
Upon signing and finalizing the HCBS/LOC Eligibility Determination within the UAS, the
HHCM/C-YES assessor will be presented with an outcome of either HCBS/LOC eligible
or not HCBS/LOC eligible, for the identified Target Population. The assessor MUST sign
the UAS Outcome report to lock the HCBS eligibility determination and if found eligible,
trigger the 12 months (365 days) of eligibility. Additionally, this trigger will send a report
to DOH Capacity Management system to add the Recipient Restriction Exception
1. Serious Emotional Disturbance (SED)
2. Medically Fragile Children (MFC)
3. Developmental Disability (DD) and Medically Fragile
4. Developmental Disability (DD) and Foster Care

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 21
(RR/E) Code K-codes to the child’s/youth’s Medicaid file demonstrating that the
child/youth is eligible and enrolled in the Children’s Waiver and can receive services. If
the K-codes are not placed on the child/youth’s Medicaid file, the HCBS provider cannot
provide services and or get paid for services provided. Collaboration between the HCBS
provider and HHCM/C-YES is necessary to ensure proper enrollment of the member
and the ability to receive services. HCBS providers should verify within eMedNY or
ePACES K-codes monthly prior to providing services.
The HHCM/C-YES will send the child/youth a Notice of Decision, which will document
the outcome of the HCBS/LOC Eligibility Determination and provide information on
State Fair Hearing rights. HHCMs/C-YES must notify the child/youth of the HCBS/LOC
eligibility determination within 3 – 5 business days of determining the eligibility outcome.
The HCBS/LOC Eligibility Determination is an annual (12 month) determination. The
annual determination date does not change according to the CANS-NY completed for
the Health Home Serving Children (HHSC) program. Once the HCBS/LOC Eligibility
Determination outcome is complete within the UAS, it remains active for one year from
the date of signature and finalization, with three exceptions:
If a child/youth is found HCBS/LOC ineligible and there is a change in circumstances,
the child/youth can be reassessed at any time, as there is no wait period between
assessments.
1. Significant life event (as noted below)
2. In the event that a child/youth that has been determined
HCBS/LOC eligible and initially declines HCBS, but later requests
HCBS, or if a child has been determined HCBS/LOC eligible but has
been placed on a waitlist due to capacity limitations of the Children’s
Waiver. A new HCBS/LOC Eligibility Determination is required if an
approved/active HCBS/LOC Eligibility Determination is not utilized
within six months from the date of the HCBS/LOC Eligibility
Determination outcomes.
3. If the child/youth is placed in a restrictive setting i.e., hospitalized or
institutionalized for longer than 90 days and is disenrolled from the
Waiver (as noted below)

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 22
The target criteria, risk factors, if applicable, and functional limits must be documented
in the UAS. Children/youth seeking HCBS who are not otherwise eligible for Medicaid
(e.g. income and resources are above Medicaid eligibility allowances) should be
referred to Children and Youth Evaluation Services (C-YES) and must meet a needs-
based criterion for Medicaid eligibility determination via the following process:
• C-YES must complete the HCBS/LOC Eligibility Determination
• If found HCBS/LOC eligible, C-YES will assist families in completion of the
Medicaid application and submission to the Local District of Social Services
(LDSS) or New York City (NYC) Human Resources Administration (HRA) to
determine Medicaid Eligibility
• Once Medicaid is established, referral to appropriate care management will be
completed by choice of the child/youth/family
HHCM or C-YES must retain the letter of notification, LOC eligibility determinations,
home assessments, plans of care, and all other information pertaining to the
child/youth's eligibility determination, enrollment and continued eligibility for the Waiver
in the applicant's file.
For more information regarding HCBS requirements for independent assessment, see
Section 1915(i)(1)(F) of the Social Security Act.
For further information, refer to the HCBS Waiver Enrollment Policy.
Please refer to Appendix G for further information regarding the impact of Medicaid
Family of One budgeting and Spenddown on HCBS eligibility and care management.
Please refer to Appendix K for further information regarding K-Codes.
NOT ICE OF DECISION
Once the Children’s Waiver eligibility determination is complete, the HHCM/C-YES will
send the child/youth/family a Notice of Decision (NOD) form.
This information must be retained for the duration of the child/youth's enrollment in
the Waiver and for at least six years after the child/youth's 21
st
birthday for possible
post-audit and evaluation by either state or federal agents.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 23
Expectations for the Completion of NOD – Enrollment or Denial
The HHCM/C-YES must issue an adequate NOD to accept or deny an application for
Waiver enrollment within 3 – 5 days of the HCBS LOC/Eligibility determination. There
should be documentation to support the enrollment/denial decision. The member has 60
days from the date of the Notice of Decision to request a Fair Hearing from the Office of
Temporary and Disability Assistance (OTDA). Fair Hearing rights are located on page 2
of DOH-5287 form. HHCMs/C-YES staff are expected to review the entire form with the
member and their family. Care managers and providers should know the process for
Fair Hearings as well as who to contact in the event the family in interested in pursuing
a Fair Hearing.
Further information regarding the Fair Hearing process is outlined in the Health Home
Notices of Determination and Fair Hearing Process policy.
Expectations for the Completion of NOD – Discontinuance
The HHCM/C-YES must issue an adequate and timely NOD to discontinue services.
The Notice of Decision for Discontiuance should be sent out within 1-2 business days of
the decision made by the HHCM/C-YES, the lead HH, HCBS provider, and other care
team members. The member has 10 business days from receiving the NOD of
discontinuance to ask for a Fair Hearing and receive continuing aid until a decision has
been made by OTDA. If the member files for continuing aid, the HCBS provider must
continue to provide services to the member until the results of the Fair Hearing are
determined. The member’s Care Manager should inform the HCBS provider(s) of
pertinent information concerning any changes in service eligibility and, if the results of
the Fair Hearing support the decision to discontinue services, then the HHCM/C-YES
should begin transition planning and documentation to support that decision. The Notice
of Decision for Discontinuance is found here.
Note: The member has 60 days from the date of the Notice of Decision to request a
Fair Hearing from the Office of Temporary and Disability Assistance (OTDA). Fair
Hearing rights are located on page two of DOH-5287 form. HHCM/C-YES are expected
to rewview the entire form with the member and their family.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 24
Additional Reasons for NOD Forms
Fair Hearing
If a child/youth and/or family does not agree with the decision indicated on the Notice of
Decision form, they have a right to a conference and/or Fair Hearing. Upon receiving a
copy of a NOD from the HH, the member has 60 days to request a Fair Hearing if they
disagree with the determination as stated on the NOD. Decisions regarding Medicaid
eligibility and the provision of waiver services (e.g., denial/reduction of services;
child/youth was not offered choice of services) can be addressed through the Fair
Hearing process. Care managers should explain these rights and the process for
requesting them to the participant and their parent/guardian/legally authorized
representative.
Information regarding the Right to a Conference and the right to Request a Fair Hearing
are located on page 2 of the Notice of Decision form and Health Home Notices of
Determination and Fair Hearing Policy.
• If child/youth lose Medicaid, the LDSS will send NOD and the HHCM/C-YES
will work with family to reestablish Medicaid; if the child/youth is eligible for
HCBS, the HHCM/C-YES will work with the family and LDSS/HRA to
reestablish Medicaid.
• If the child/youth is HCBS LOC eligible but no slot is available, the family will
receive a NOD from the HHCM/C-YES and when a slot is available, the
HHCM/C-YES will send the family a letter notifying them of the available slot.
• For children/youth in the Target Populations DD Med Frag or DD foster care,
please refer to the OPWDD DDRO Manual for Children’s Waiver for guidance
for each applicable situation.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 25
HCBS Eligibility Reauthorization
The 1915(c) Children’s Waiver for HCBS requires an annual (12 month) HCBS/LOC
Eligibility Re-determination to be completed for the child/youth to remain in the Waiver
and continue receiving Waiver services.
All HHs, HH CMAs, and C-YES should audit their records of Waiver-enrolled
children/youth to ensure all HCBS LOCs are up to date and completed timely. HHCM/C-
YES staff should begin gathering annual re-determination supporting documentation
two months prior to the re-determination due date to ensure enough time to complete
the annual HCBS LOC within the required timeframe (365 days).
Note: For children/youth requiring an ICF-IDD LOC from OPWDD Developmental
Disabilities Regional Office (DDRO), it is important to remember this process can take
up to a month to complete. Timely and on-going communication with the DDRO is
encouraged.
Significant Life Event
If a significant life event occurs for a child/youth while receiving HCBS, a new
HCBS/LOC Eligibility Determination may be needed. A significant life event is
something that occurs in a child’s/youth’s life that impacts their functioning, daily living
situation, or those that care for the child/youth. Reasons for HCBS/LOC Reassessment
Change of Circumstances include:
• Significant change in child/youth’s functioning (including increase or decrease
of symptoms or new diagnosis)
• Service plan or treatment goals were achieved
• Child/youth admitted, discharged or transferred from hospital/detox,
residential setting/placement, or foster care
• Child/youth has been seriously injured in a serious accident or has a major
medical event
• Child/youth’s (primary or identified) caregiver is different than on the previous
HCBS/LOC
• Significant change in caregiver’s capacity/situation

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 26
If the child/youth is also enrolled in the Health Home program, a significant life event
may also require a full CANS-NY to be completed. The CANS-NY is completed on a
yearly cadence otherwise and may not coincide with the HCBS/LOC eligibility
determination.
Participant Placed in an HCBS Restricted Setting
If a child/youth enrolled in the Children’s Waiver is hospitalized or placed in an HCBS
restricted setting, then the child/youth can remain in such setting for 90 days prior to
having to be disenrolled from the Children’s Waiver program. If the Waiver child/youth is
also enrolled in the Health Home program while entering a restricted setting, the HHCM
would “pend” the enrollment segment in the MAPP tracking system.
Follow the Health Home Continuity of Care and Re-Engagement for Enrolled Health
Home Members policy.
Please also refer to Appendix G for guidance related to referring for HCBS while a
child/youth is in a restricted setting, including a Residential Treatment Facility (RTF) or
OMH State-operated Psychiatric Centers Serving Children (State PC).
HHCMs should also refer to the HH Care Management Activities and Billing Protocols
for Managing Newly Referred Individuals from Excluding Settings.
Capacity Management
Capacity Management is the process by which New York State manages the allowable
number of enrolled participants and available slots for the 1915(c) Children’s Waiver.
Slot capacity is tracked by Target Population and by Region. Slot capacity is monitored
to ensure that all regions have equitable access to the Children’s Waiver. Should
Capacity Management become concerned about Waiver enrollment reaching a
threshold, then a waitlist might occur and limits by Target Population and Region will be
set.
Capacity Management Process
The NYS DOH Capacity Management Team receives information from the Uniform
Assessment System (UAS) daily reporting all completed HCBS/LOC Eligibility
Determinations. This report allows the DOH Capacity Management Team to begin the
process to place the K-codes on the participant’s Medicaid file to notify HCBS providers
and Medicaid Managed Care Plans that the child/youth is eligible and enrolled within the
Waiver. The Capacity Management Team will notify the HHCM/C-YES assessor of any

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 27
newly assessed (initial assessment only) and eligible child/youth of their slot availability
within one business day of the completed, signed/finalized assessment outcome. The
HHCM/C-YES assessor will receive a Health Commerce System (HCS) Secure File
Transfer (SFT) email with a subject line “Slot Availability” indicating if the child/youth has
secured a slot prior to HCBS being provided or if the child/youth is on a waitlist. The
HHCM/C-YES should not send Notice of Decisions or send HCBS referrals to providers
until verifying the new member slot availability.
It is necessary for HHCM/C-YES to also notify DOH Capacity Management Team when
a participant is being disenrolled from the Waiver so the K-code can be removed from
the participant’s Medicaid file.
There are specific requirements about how and when communication is required by
HHCM/C-YES to Capacity Management, which are located in the Children’s Waiver
Communication to/from NYS Capacity Management Requirements and the Capacity
Management and RR/E K-Codes Webinar.
Capacity Tracker/Waitlist
All HCBS Providers are required to complete the Children’s Services Capacity Tracker
survey every three weeks. Due dates for the survey are on Fridays at 11:59pm. The
Children’s Service Capacity Tracker is located within the Incident Reporting and
Management System (IRAMS) system and is a requirement for compliance. In addition
to the survey, providers are required to maintain an ongoing waitlist within the system.
This Capacity Tracker is distinct from the DOH Capacity Management Process outlined
in the previous section.
For general guidance and instruction on the Children’s Services Capacity Tracker
System, please reference the User Guide, FAQ, and webinars.
HCBS DISENROLLMENT
Overview
The HHCM/C-YES and HCBS providers maintain a responsibility for carrying out the
discharge planning for the child/youth being disenrolled from the Children’s Waiver
and/or discharged from HCBS.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 28
The situations under which children/youth may be disenrolled from the Children’s
Waiver and/or discharged from HCBS include:
Additional information can be located in the HCBS Waiver Disenrollment and Discharge
Policy and Appendix H of this Manual.
Disenrollment Process
Once determined that disenrollment is appropriate and/or necessary, the HHCM/C-YES
will issue the child/youth/family a Notice of Decision (NOD) for Discontinuance
explaining the reason for the disenrollment from the Children’s Waiver. This notice
should be sent within 1-2 business days of the decision made by the HHCM/C-YES to
the family the lead HH, HCBS provider, and other care team members. Prior to sending
the NOD, the HHCM/C-YES must discuss options with the child/youth/family, if they are
no longer found eligible for HCBS, including their option to request a Fair
Hearing, following the process as outlined in the HCBS Notice of Decision for
Discontinuance and HCBS Waiver Disenrollment and Discharge policy.
The HHCM/C-YES will also need to complete the Fair Hearing / State Review NOD
within the child/youth’s HCBS/LOC Eligibility Determination in the UAS to indicate the
change in status.
1. Child/youth no longer meets admission criteria and/or meets
criteria for another, more appropriate service, either more or less
intensive.
2. Child/youth or parent/guardian withdraws consent for
treatment.
3. Child/youth is not participating in the POC development and/or
utilizing referred services.
4. Child/youth’s needs have changed, and current services are not
meeting those needs.
5. Child/youth’s goals would be better served with an alternate
service and/or service level.
6. Child/youth’s POC goals have been met.
7. Child/youth’s support system is in agreement with the aftercare
service plan.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 29
The HHCM/C-YES must give notice to the HCBS providers, Medicaid Managed Care
Plans, and other involved providers of the disenrollment/discharge of a participant.
The HHCM/C-YES must also communicate any discharge and/or disenrollment
to DOH Capacity Management in a timely manner and provide the date of discharge or
disenrollment, reason for discharge or disenrollment, name, date of birth, CIN,
and Target Population. In instances of disenrollment, Capacity Management will remove
the R/RE K-codes from the file (see Appendix K for a list of K-codes).
In addition to communication with Capacity Management, the HHCM/C-YES must also
communicate the change in status with all involved interdisciplinary team
members, provider(s), and MMCP, as appropriate.
Discharge from HCBS Process
In some cases, a child/youth may be discharged from an individual HCBS that no longer
meets the child/youth’s goals, but the child/youth may remain in receipt of additional
needed HCBS and enrollment within the Waiver. In all instances of individual
service discharge, whether accompanied by disenrollment from the Children’s Waiver
or continuation of alternative HCBS, both the HHCM/C-YES and HCBS provider(s) will
need to execute and document the discharge planning process in the Case Record.
CARE MANAGEMENT AND MONIT ORING ACCESS T O CARE FOR
HCBS
Additional Information can be found in
The HCBS Waiver Disenrollment and Discharge Policy.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 30
Care Management
Children and youth who are enrolled in the Children’s Waiver, are HCBS/LOC eligible,
and are receiving HCBS are required to receive care management. This requirement
may be met in one of the following three ways:
Care management is required for all participants receiving HCBS. The HCBS referred
and provided cannot duplicate or replace existing and required care management
services through HHCM/C-YES. HCBS providers must communicate with HHCM/C-
YES regarding any additional care management needs the participant/family may have;
it is then the HHCM/C-YES’s responsibility to coordinate such related services.
• HH comprehensive care management: Children/youth eligible for HCBS are
eligible for HH services, including comprehensive care management; care
coordination and health promotion; comprehensive transitional care; enrollee
and family support; and referral to community and social supports. HH
comprehensive care management ensures a holistic assessment, through the
CANS-NY and comprehensive assessments, of the child/youth’s behavioral
health, medical, community and natural supports as identified through a person-
centered Plan of Care (POC) by the child/family.
• C-YES: If a child/youth and their family do not want HH care management
(which is an optional benefit), they can opt-out of HH and receive HCBS care
management from C-YES. C-YES will develop a HCBS POC using information
from the HCBS/LOC Eligibility Determination, and a person-centered discussion
that identifies personal goals and how specific HCBS may support the child in
achieving those goals. C-YES will maintain the POC for children who opt of HH
and are not enrolled in a Medicaid Managed Care Plan.
• MMCP: For children/youth who opt-out of HH and are enrolled with a MMCP,
once C-YES establishes HCBS/LOC eligibility and the HCBS POC, the MMCP
updates the POC annually through a person-centered planning process. C-YES
conducts the HCBS/LOC Eligibility Determination annually for children/youth
who are managed by the MMCP.
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 31
Monitoring Access to Care
The State must ensure children/youth participating in the Children’s Waiver are able to
access and receive HCBS identified in the POC. The MMCP will monitor access to care
for all enrolled children/youth in receipt of HCBS. The HH will monitor access to care for
children and youth in receipt of HCBS who are enrolled in the HH and are not enrolled
in an MMCP. C-YES will monitor access to care for children/youth in receipt of HCBS
who opt out of HH and are not enrolled in an MMCP.
Contact with the family may be by phone or other regular communication methods
(unless otherwise outlined) and must occur at least once per quarter for C-YES and the
MMCP and once per month for HHCMs. This verification can be combined with a
regularly scheduled meeting or care management contact with the child/youth and
family. HHCM/C-YES should document this contact in a case note. The monitoring
access to care requirement does not change the high-medium billable standard for HHs.
Alternatively, MMCPs can combine monitoring of access to care with the plan’s service
verification activity.
In-person meetings between the HHCM and the child/family are required based upon
CANS-NY acuity or if the child/youth has Medicaid Family of One budgeting and is not
receiving a monthly HCBS. In-person meetings must have a purpose and an outcome;
meetings for social and recreational purposes are not appropriate.
Contact by the care management entity with HCBS providers must occur to ensure that
appointment times and scheduling accommodates the family’s schedule and ability to
attend. Additionally, this contact occurs to verify that the service(s) is meeting the
identified need and progressing towards established identified goals.
The HCBS provider(s) need to be an active member in the family’s care team and
person-centered POC development, monitoring, and planning. HCBS providers should
attend meetings that discuss the POC, communicate with care managers regarding the
child/youth’s progress toward goals and/or any changes in status/significant life events,
and be aware of care management requirements to facilitate an effective conversation
with the child/youth.
Monitoring access to care means that there is contact with the child/youth and family
to ensure that they are receiving the HCBS indicated in the POC within 45 days of
the POC being signed by the child/youth and the parent/guardian/legally authorized
representative and have contact with the HCBS providers to ensure child/youth and
family are attending the appointment and working toward established identified
service goals.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 32
PERSON-CENT ERED PLAN OF CARE
Plan of Care (POC) Development
To develop a POC, the HHCM/C-YES must meet with the child/youth and their family
and their identified care team to discuss the strengths and needs of the child/youth,
using person-centered planning guidelines/principles. The person- centered service
planning process guides the delivery of services and supports towards achieving
outcomes in areas of the individual’s life that are most important to them (e.g., health,
relationships, work, and home, etc.). HHCMs/C-YES and MMCPs are responsible for
ensuring that the POC is developed and services are authorized in accordance with the
POC. The PCSP process and POC must reflect the person’s choices, preferences, and
goals, and support his or her inclusion in the community.
The child/youth and their family/caregiver will lead the development of the POC,
alongside the HHCM/C-YES and involved care team members. The POC development
is based upon the assessment of needs which is determined through interaction with
the child/youth, their family, the child/youth’s representative (if applicable), and identified
supports as well as through the multi-disciplinary team meeting/information, CANS-NY
(for HH), HH Comprehensive Assessment, and HCBS/LOC Eligibility Determination.
The POC involves collaboration between the HHCM/C-YES, the child/youth, the
family/caregiver, family-identified supports, providers, other child-serving systems, and
the MMCP (if enrolled).
The HHCM/C-YES will recommend services that can support the child/youth in reaching
their defined goals and addressing identified needs. Each HCBS that the child/youth
receive must be listed in their POC with a defined goal. HCBS providers must refer to
the POC during service delivery to ensure that the services provided are in alignment
with the POC. HCBS providers will also play a role in providing information to care
managers regarding progress toward goals that will be used in updating the POC.
The POC will change and evolve over time as the child/youth meets their goals or
there is a need for new services/supports. The POC is a fluid document that can be
developed incrementally and may be updated at any time. At a minimum, the POC
must be reviewed annually.The POC must also be reviewed any time the child/youth,
and/or parent/guardian requests a review, and/or any time a significant life event
occurs. The POC must be reviewedduring the HCBS/LOC Eligibility determination
reassessment.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 33
The POC must be signed by the child/youth, if age appropriate (i.e., able to understand
and contribute to their own POC) and/or the parent, guardian, or legally authorized
representative. All involved providers must be given an opportunity to contribute to the
POC and, with informed consent of the child/parent/guardian/legally authorized
representative, sign the POC when it is developed. Services must be provided within 45
days of POC approval (i.e., the date it is signed by the child/youth/parent/guardian).
POCs must be developed following the NYS Person-Centered Planning Guidelines and
the Health Home Plan of Care Policy.
Development of the POC and Referrals for HCBS
At the time of the initial development of the POC, the POC must identify the need(s) of
the child/family, the chosen HCBS, and goal/outcome to be attained. The POC must be
reviewed with the child/family, signed by the child/family, and copies given to the
child/family and, with informed consent, to the involved multi-disciplinary team providers
upon request if appropriate. HCBS providers should have a role in POC updates and
changes to the POC. To obtain and document consent for the HCBS provider to
communicate with care team members, HCBS providers must have their own consent
form and related policy and cannot utilize the HH 5201 form.
When adding identified needs and services to a POC (initial and/or updated), it is not
necessary to immediately identify the specific providers; providers should be specified
once it is assured the HCBS provider identified and chosen has availability to accept the
referral. Additionally, forms have been developed, as indicated in this Manual, to
facilitate updating and sharing the POC. This process will also ensure that the HHCM/C-
YES are compliant with the child/family-specific Protected Health Information (PHI)
requests regarding the sharing of the POC with various providers. HCBS providers must
also follow requirements to protect PHI.
HCBS Service Plan
Once a HCBS provider receives a referral from a care manager, the HCBS provider will
meet with the child/youth and family/caregiver to identify how the referred services will
help to address identified needs. Based on the determination of needs, the HCBS
provider is responsible for documenting the approach for service provision on an HCBS
Service Plan for the services they expect to provide. The purpose of the HCBS Service
Plan is to outline the service(s) that will/is provided with corresponding goals and
objectives that describes the need for the service(s) and the anticipated benefit to the
child/youth and family. The HCBS Service Plan determines the focus of the particular

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 34
service(s), while also documenting the scope, duration, and frequency to which each
service will be provided. An HCBS Service Plan is required to outline each of the
services the HCBS provider is providing to the child/youth. If the child/youth is referred
to more than one HCBS provider, then each HCBS provider will have their own Service
Plan for the services they will provide to the child/youth. The HCBS provider is required
to communicate the scope, duration, and frequency of the service to the HHCM/C-YES
and have regular contact regarding the service delivery and the service plan progress.
Components of a HCBS Service Plan
As with any Service Plan, it is expected that the plan will be developed within 30 days of
the first in-person appointment with the child/youth and family/caregiver. The necessary
components of the HCBS Service Plan should, at a minimum, include the following:
a) Child’s Name
b) Child’s home address and phone number
c) Date of Birth
d) CIN (Medicaid #)
e) Managed Care Organization (if applicable) and Member ID
f) Lead HH or C-YES
g) HH CMA or C-YES
h) HHCM or C-YES staff, including their contact information
i) HCBS Provider: The name of the agency delivering services as well as contact
information for the agency/provider
j) Service Plan Development Date
k) Goals and Objectives of the service(s)
l) Scope: The service components and interventions being provided and utilized to
address the identified needs of the child
m) Duration: Describes how long the service will be delivered to the child and/or
family. The duration of the service should correspond to the abilities of the
child/family and be reflective of the billing unit identified by service.
n) Frequency: Outlines how often the service will be offered to the child and/or
family. Services may be delivered on a weekly, biweekly or monthly basis,
according to the needs of the child and family.
Note: The duration of a service should not exceed six months at a time. This timeframe
provides enough time for the HCBS provider to evaluate if the service(s) is meeting the
child/youth’s needs and whether the service(s) should be continued or discontinued.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 35
Expectations for the Development of a HCBS Service Plan
The HCBS Service Plan should begin with the service(s) referred to an HCBS provider
based upon the needs identified by the HHCM/C-YES. The HCBS Service Plan should
continue the care manager’s discussion with the child/youth and family/caregiver while
ensuring their involvement in the development of the Service Plan and that the goals
outlined by the child/youth and family/caregiver are captured in the plan. The
development of this plan should begin during the first meeting with the child/youth and
family/caregiver as the goals are discussed. The HCBS Service Plan must be
completed within 30 days of the first in-person appointment with the child/youth and
family/caregiver. The duration and frequency of service delivery should not be
dependent upon the availability of the provider, but rather, the availability and needs of
the child/youth. The frequency of services should be in relation to other appointments or
commitments the child/youth may have, including but not limited to any educational or
vocational placement, medical or behavioral health therapies, community activities, etc.
and not be delivered beyond “typical" hours available when these things are considered
in addition to the child/youth’s age, attention span, and development. HCBS cannot be
provided during school/educational hours. A plan, including the types of interventions
provided and the goals to be achieved, must be developed that is reflective of the
developmental and physical needs of the child/youth.
The HCBS Service Plan should be monitored regularly , every month when services are
delivered. If there is a significant change in the child/youth’s health, hospitalization,
functioning, living situation, incarceration, or other significant life event, the HCBS
Service Plan must be reevaluated to determine whether the goals remain appropriate.
The HCBS Service Plan may be modified at the request of the child/youth and
family/caregiver at any time. Whenever a modification is made to the HCBS Service
Plan, it must be reviewed in total with the child/youth and family/caregiver and
appropriate signatures obtained, including the child/youth (if appropriate, and if not, it
should be specified that the child is unable to provide a signature), the parent/caregiver
of the child/youth and the signature of the HCBS provider. The HCBS provider must
communicate with the HHCM/C-YES regarding any changes, so it can be determined if
there is a change needed to the child/youth’s POC as well as the potential for other
services needed.
Note: Based on the 1915(c) Waiver amendment from April 2022, “Caregiver Family
Supports and Services” (CFSS) was combined with “Community Self-Advocacy Training
and Supports” (CSATS) into the consolidated service “Caregiver/Family Advocacy and
Support Services.” If a child had separate service plans for CFSS and CSTAS, these
separate plans must be combined into one plan under the new service title. Please also

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 36
note that when appropriate, a Service Plan may include all HCBS that a child/youth
receives from an agency on one singular Service Plan.
Plan of Care Workflow
DOH issued the HCBS POC Workflow Policy and the required use of related forms to
facilitate information sharing between the HHCM/C-YES, HCBS providers, and MMCPs.
Please refer to the HCBS POC Workflow Policy for the complete HCBS POC Workflow
process.
PART ICIPANT S RIGHT S AND PROT ECT IONS
Overview
In compliance with CMS and the 1915(c) Children’s Waiver, participants must be
informed of their rights and protections regarding their options to receive care, how to
report a complaint and/or grievance, how to report abuse or suspected abuse, and
when and how to request a Fair Hearing. Documentation indicating that this information
has been provided must be included in the child/youth’s case file maintained by the
designated HCBS provider agency.
HHCMs and C-YES care managers must also adhere to guidance regarding protocols
and reporting requirements intended to ensure the safety and well-being of Waiver
participants.
Freedom of Choice
Eligible individuals must be informed of feasible alternatives for care and given the
choice of either institutional or Home and Community-Based Services. During an in-
person meeting, the HHCM/C-YES will provide information and discuss Freedom of
Choice. The individual’s parents/guardians/legally authorized represented must sign the
Freedom of Choice form indicating their decisions and whether to participate in the
HCBS 1915(c) Children’s Waiver. This form must be witnessed and dated and kept as
part of the member’s HH/C-YES’ file with a copy provided to the member upon request.
Care managers are responsible for explaining the participant’s options and reviewing
the Freedom of Choice form. With this form, the participant will indicate their decision for
the following choices:
• Choice between HCBS and an institution (such as a hospital, ICF-IDD, or nursing
home)

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 37
• Choice to receive care coordination through HH or C-YES; if choosing HH, the
participant may also choose their CMA/care manager
• Choice of service providers
Although care managers are responsible for providing information regarding Freedom of
Choice and the Participant: Rights and Responsibilities Fact Sheet. HCBS providers
should understand and honor the family’s right to the choice of services and document
that those choices were provided.
Incident Reporting
Care managers and HCBS providers must follow their agency processes for managing
and recording reportable incidents, which include the following:
1.
Allegation of abuse, including
o Physical abuse
o Psychological abuse
o Sexual abuse/sexual contact
o Neglect
o Misappropriation of member funds
2.
Suicide attempt
3.
Death
4.
Crime Level 1
5.
Missing person
6.
Violation of Protected Health Information (PHI)
7.
Exploitation
8.
The use of restrictive interventions, including restraints and seclusion
DOH requires that all complaints/grievances and critical incidents are timely
documented within the Incident Reporting and Management System (IRAMS). HCBS
providers must have procedures in place to ensure the timely review and resolution of
member’s complaints and grievances, and they are responsible for creating a process
and informing the member of timeframes for addressing verbal or written complaints or
grievances. This process must include contacting and updating the member within 72
hours of receiving the complaint or grievance. Response and resolution of the complaint
Additional Information can be found in
The Children’s Waiver Participant: Rights and Responsibilities Fact Sheet.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 38
or grievance process cannot exceed 45 calendar days from the receipt of the complaint
or grievance. Documentation of the resolution must be in the member’s file.
For further information, refer to the IRAMS User Guide.
Care managers should refer to Health Home Monitoring: Reportable Incidents Policies
and Procedures, and HCBS providers should refer to HCBS Provider Reportable
Incidents Policies and Procedures.
Grievances and Complaints
Care managers and HCBS providers must follow their agency processes for managing
and reporting grievances and complaints. Grievances and complaints are external to,
but not in lieu of, the existing right to request a Fair Hearing. Children’s Waiver
participants should be informed, by their care manager, of the process for submitting a
grievance or complaint related to their HCBS, care coordination, or participation in the
Children’s Waiver.
DOH’s process for grievances and complaints is not intended to replace the Medicaid
Fair Hearing process and therefore, members should be made aware that filing
a grievance or making a complaint is not a prerequisite or substitute for a Medicaid Fair
Hearing. DOH requires that all complaints/grievances and critical incidents are timely
documented within the Incident Reporting and Management System (IRAMS).
For further information, refer to the IRAMS User Guide.
MMCPs should refer to requirements for addressing and reporting grievances and
complaints as outlined in the Model Contracts and 1915(c).
Health Homes should refer to the Health Home Grievances and Complaints Policy, and
HCBS Providers should refer to the HCBS Provider Grievances and Complaints Policy.
Conflict Free Case M anagement
Per federal regulation §441.301(c)(1)(vi), states are required to separate case
management (including the development of person-centered plans) from service
delivery functions for services delivered under 1915(c) waivers. Care managers must
implement conflict-free case management principles. A “conflict of interest” is defined as
a “real or seeming incompatibility between one’s private interests and one’s public or
fiduciary duties.” When the same entity is both assisting an individual to gain access to

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 39
services and providing services to that individual, the role of the care manager has
potential to be conflicted. Further, for HHCMs who are also employed by an HCBS
provider, that HHCM cannot provide HCBS to children/youth who are also on the
HHCM’s case load.
Note: To maintain the enrollee’s autonomy and Freedom of Choice, it is not allowable
for a HHCM or HCBS Provider to be related by blood or marriage to the served
child/youth. Further, an individual residing in the same residence as the HCBS-enrolled
child/youth or in a relationship with someone residing in the same residence, would not
be an appropriate HHCM or HCBS provider. It is up to the agency to determine if a
conflict of interest is present in a potential staffing relationship beyond the specifics
provided above, and whether the family believes there is an opportunity for Freedom of
Choice. Subsequently, it is not appropriate and is a conflict to request that the
child/youth/family/caregiver find and or obtain their own provider to then be employed by
an HCBS provider.
Quality Monitoring and Oversight
HCBS providers are responsible to develop policies, procedures, and processes that
align with the requirements to deliver HCBS. HCBS providers are required to ensure all
staff/employees/providers working for the designated agency are properly trained to all
HCBS requirements and monitored for compliance with the requirements outlined in the
Background Check Requirements for HCBS Providers policy. HCBS providers should
have a process in place to monitor and regularly audit cases and the delivery of
services.
Annual Children’s Waiver Case Review and Audit
On an annual basis, the NYS DOH will conduct a case review and audit of the previous
waiver year’s (April 1
st
through March 30
th
) services and providers, inclusive of HCBS
providers, Health Homes, Health Home care managers, and C-YES policies, records,
reporting, claims/billing, and other HCBS requirements. This information is required to
be reported to NYS DOH as part of the waiver annual case review and audit to meet
performance measures within the Children’s Waiver and reported to CMS.
Additional Information can be found in
The Conflict Free Case Management Policy.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 40
BILLING AND CODING FOR HCBS
Overview
This section outlines general claiming requirements necessary to ensure proper claim
submission for HCB services. This information was previously located in the separate
New York State Children’s Health and Behavioral Health Medicaid System
Transformation: Billing and Coding Manual and has been integrated into this Manual
instead, with general information in the “Billing and Coding for HCBS Services” section
and service-specific details, such as rate codes, within the “Service Definitions” section.
The content included within applies to services covered by Medicaid Managed Care
(MMC) and the Medicaid fee-for-service (FFS) delivery system. The billing guidance in
this document does not supersede applicable regulatory requirements or procedures for
admission to a program, record keeping, service documentation, initial and on-going
treatment planning and reviews, etc. Contents of this Manual are subject to change.
Fundamental Requirements
Provider Designation to Deliver Services
Providers are required to receive a designation from NYS to provide and be reimbursed
for Children’s HCBS. For more information qualifications required for provider
designation, refer to “Provider Requirements” section of this Manual.
HHs, HH CMAs, C-YES, and HCBS providers must comply with all requests for records
and files, as well as agency’s/organization’s practices as requested by NYS DOH or
their designee. Agencies/organizations can be de-designated for care management
services or HCBS if failing to meet these requirements.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 41
Services that Do Not Require State Designation
The following services do not require State designation; these will be coordinated
between the Care Management agency/C-YES, LDSS/MMCP, and DOH.
• Adaptive and Assistive Technology (AT)
• Environmental Modifications (EMods)
• Vehicle Modifications (VMods)
• Non-Medical Transportation
Medicaid-Enrolled Provider
As referenced earlier in this document, all providers eligible to enroll in Medicaid are
required to enroll in Medicaid to be paid for delivering a Medicaid service. Information
on how to become a Medicaid provider is available on the eMedNY website.
For additional information specific to Medicaid provider enrollment for children/youth
services, refer to the MCTAC CTAC training and the DOH memo on Medicaid Provider
Enrollment for Individual Practitioners and Designated Agencies.
Medicaid Managed Care Plan Contracting
To be paid for services delivered to a child/youth enrolled in a Medicaid Managed Care
Plan, a provider must be contracted and credentialed with that MMCP for the service
rendered (i.e., in the MMCP’s network).
A MMCP has discretion to deny a claim from an out of network provider:
• Exception: For any of the newly carved-in services, if a provider is delivering a
service to the enrollee prior to the implementation date and does not contract with
the MMCP, the MMCP must allow a provider to continue to treat an enrollee on an
out of network basis for up to 24 months following the implementation date.
• Single Case Agreements (SCA) may be executed between a MMCP and a
provider when an out of network provider has been approved by a MMCP to
deliver specific services to a specific MMCP enrollee. MMCPs must execute SCAs
with non-participating providers to meet clinical needs of children/youth when in-
network services are not available. The MMCP must pay at least the NYS
government rates for 24 months from the service implementation date.
MMCPs are held to specific network requirements for services described in this Manual.
NYS monitors MMCP contracting regularly to ensure network requirements are met.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 42
RATES
Government Rates
NYS law requires that MMCPs pay government rates (otherwise known as Medicaid
fee-for-service rates) for certain services, including Children’s HCBS, administered by a
MMCP.
MMCPs will be required to pay government rates until otherwise notified.
Productivity Adjustment
HCBS rates are subject to change based on factors such as budget adjustments,
Waiver amendments, Federal regulation, and other similar external events. Any
temporary rate adjustments for the budget year will be reflected in the HCBS rate chart
available on the DOH website.
Regions
Regions are assigned to providers based upon the geographic location of the provider’s
headquarters, and are defined by DOH as follows:
• Downstate: 5 boroughs of New York City, counties of Nassau, Suffolk,
Westchester, Rockland, Putnam, Orange, Dutchess, Sullivan and Ulster
• Upstate: Rest of State
CLAIM S
General Claim Requirements
1
Electronic claims will be submitted using the 837i claim form to both Medicaid FFS and
MMCPs. Paper claims (UB-04) and web-based claiming will also be accepted by
MMCPs. For Medicaid Managed Care billing for EMods, VMods, and AT, please refer to
applicable guidance in this Manual.
Each service has a unique rate code. If a child/youth receives multiple services in the
same day with the same Current Procedural Terminology (CPT) code, but separate rate
codes and modifiers, all services would be payable.
1
NYS will be reviewing claim and encounter data periodically and annually, or upon information that
there has been fraud or abuse, to determine if inappropriate HCBS combinations were
provided/allowed. In instances where such combinations are discovered, NYS will make the appropriate
recoveries and referrals for judicial action.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 43
Enrollment Status
Before delivering services to a child/youth, providers are responsible for checking the
Electronic Provider Assisted Claim Entry System (ePaces)
2
to verify the child/youth’s:
Claims will not be paid if a claim is submitted for a child/youth who is not enrolled with
Medicaid, a child/youth not eligible for HCBS, or if the claim was submitted to an
incorrect MMCP.
Medicaid Fee-For-Service Claiming (eMedNY)
Claims for services delivered to a child/youth in receipt of fee-for-service Medicaid are
submitted by providers to eMedNY. See the eMedNY website for training on use of the
eMedNY system. Claim submissions need to adhere to the 90-day timely filing rules for
Medicaid FFS, unless the claim is delayed due to circumstances outside of the
provider’scontrol—for example, attempts to recover from a third-party insurer or legal
proceedings against a responsible third-party. See NYS Medicaid timely billing guidance
here.
Medicaid Managed Care Plan Claiming
MMCPs and providers must adhere to the billing and coding rules in this Manual.
The MMCP shall support both paper and electronic submission of claims for all claim
types. The MMCP shall offer its providers an electronic payment option including a web-
based claim submission system. MMCPs rely on CPT codes and modifiers when
processing claims. Therefore, all MMCPs will require claims to be submitted with the
CPT code and modifier (if applicable), in addition to the NYS assigned rate code.
Providers will enter the rate code in the header of the claim as a value code. This is
done in the value code field by first typing in “24” followed immediately with the
appropriate four-digit rate code. This is the standard mechanism historically and
currently used in Medicaid FFS billing.
3
2
ePaces is a web-based application which will allow Providers to create/submit claims and other transactions in
HIPAA format.
3
Attention MMCPs: This field serves a dual purpose and is already used by MMCPs to report the weight of a low
birth weight baby.
• Medicaid enrollment status
• HCBS eligibility status – both Level of Care (LOC) and active, correct k-code
(before delivering HCBS)
• MMCP enrollment status

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 44
Billing requirements depend on the type of service provided; however, every claim
submitted will require at least the following:
Sample institutional claim form can be found through MCTAC/CTAC.
MMCPs will not pay claims if submitted without the applicable rate code, CPT code, and
modifiers. If an individual service has multiple modifiers listed, they must all be included
on the claim submission. If an MMCP receives an HCBS claim for a child whose
enrollment in the Children’s Waiver cannot be verified by confirming a K1 Recipient
Restriction/Exemption (RR/E) code on the child’s record, and/or if the MMCP has not
received an HCBS Authorization and Care Manager Notification Form for the billed
service(s) provided beyond the initial 24 hours/60 days/96 units, the MMCP should deny
the claim for lack of verification of Children’s Waiver eligibility, enrollment, and approved
service. The MMCP may also deny the claim if the units billed are not supported by the
frequency, scope, and duration documented on the HCBS Authorization and Care
Manager Notification Form.
Providers must adhere to timely filing guidelines as outlined in their contract with the
MMCP. When a clean claim is received by the MMCP, the Plan must adjudicate per
prompt pay regulations.
If a provider does not have a contract or a Single Case Agreement in place with the
MMCP, the claim can be denied.
Services Included in or Excluded from Capitation Payments to Medicaid Managed
Care Plans
The MMCP capitation payment will not include Children’s HCBS and MMCPs will not be
at-risk for Children’s HCBS until at least September 30
th
, 2023. DOH will confirm this
date in writing. MMCPs will be reimbursed on FFS basis outside the capitation rate by
submitting claims for Children’s HCBS to NYS under supplemental rate codes.
All non-risk payment claims that have a valid delay reason code must be submitted to
eMedNY within two years from the date of service. Please refer to eMedNY for further
information regarding non-risk billing guidance.
• Use of the 837i (electronic) or UB-04 (paper) claim format
• Medicaid fee-for-service rate code
• Valid CPT code(s)
• CPT code modifiers (as needed)
• Units of service
• Revenue codes

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 45
Non-risk payment claims must include the same fields as in all other claims (i.e., rate
code, procedure code, modifier(s) as applicable, units of service, revenue codes). The
rate code/CPT code/modifier code combinations for the services described in this
document are shown within each “Service Billing Details” subheader in the Service
Definitions section.
Third-Party Health Insurance Denials
It is the provider’s responsibility to determine the type of coverage (Medicare, Medicaid,
or private insurance) that the member is eligible to receive. Medicaid is the payor of last
resort and all Medicare and third-party coverage must be exhausted before payment for
HCBS by Medicaid.
Acceptable documentation of attempts to secure third party reimbursement as required
under 18 NYCRR §540.6 includes documentation of a rejection by third party insurance
for a date of service within the previous 12 months of the date of service being billed, or
since a change in third party coverage, whichever is later.
There are exceptions to this requirement for 29-I Health Facilities delivering HCBS to
children/youth in foster care. Refer to the 29-I Billing Manual for additional details.
Services Delivered by Multiple Staff Members
If two practitioners are required to deliver a service to a child/youth and family
members/resources on the same date and at the same time, the provider must
delineate what service and what goals each practitioner is addressing directly with the
child/youth and on behalf of the child/youth in the child/youth’s progress notes. The
need for two practitioners should reflect the needs of the child/youth and/or
family/caregiver and be aligned with the goals outlined in the POC and HCBS Service
Plan. The claim should reflect the time spent for each practitioner in a single claim.
Services and staffing should be streamlined whenever possible. No more than two
practitioners can provide HCBS to the child/youth and family members/resources on the
same date and at the same time.
Example: Practitioner (A) meets with the child/youth directly to deliver
Caregiver/Family Advocacy and Support Services from 10:00 am to 10:30 am and
Practitioner (B) meets with a family member/resource to deliver Caregiver/Family
Advocacy and Support Services addressing a need on the behalf of the
child/youth from 10:00 am to 10:30 am. The combined claim would reflect the 60-
minute combined duration of the service.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 46
Children’s HCBS participants cannot receive the same HCBS from multiple designated
provider agencies (e.g., participant cannot receive Planned Respite from both Provider
Agency (A) and Provider Agency (B). If extenuating circumstances necessitate the
provision of the same HCBS from different providers, the HHCM/C-YES must provide
documented justification for these scenarios and receive approval from the State.
Multiple Services Provided on the Same Date to the Same Child/Youth
In some cases, a child/youth can receive multiple HCB services on the same day. This
can include services provided by separate providers (e.g., planned respite and
Supported Employment). If these services are allowed per the service combination grid
in this Manual, they would both be reimbursable when billed using the appropriate rate
code and CPT code.
Services Provided During School/Day Time
HCBS cannot be duplicative or delivered at the same time as services otherwise
available to the individual through a local educational agency for educational services in
grades K - 12 under the Individuals with Disabilities Education Act (IDEA) or Vocational
Rehabilitation under the Rehabilitation Act of 1973.
The schedule for HCBS delivery for children/youth who attend K-12 school in-person
must be outside of regular school hours. For students who are home schooled or
receiving virtual instruction, HCBS can be delivered during traditional school hours, but
the services must be outside the scheduled time for educational instruction provided to
the child.
Support for adult education outside of K-12 education may be provided under the HCBS
waiver. Technical schools, colleges, and other adult education settings are approvable
HCBS settings because adult education and adult education settings are not
addressed/prohibited under the IDEA.
Please refer to HCBS Versus State Plan Services Delivered During School/Day Time
for more information.
Services Provided While in Transit
Services that are delivered in transit are allowable and may be billed within the daily
limits of the service.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 47
Out of State Services
Only providers located in New York State are eligible to become designated HCBS
providers. Children/youth must be enrolled in New York State Medicaid to receive
Children’s HCBS, and the services must be provided in the state in which the Medicaid
recipient is enrolled in Medicaid. As such, while an individual HCBS provider may reside
in a neighboring state, the HCBS must be provided in New York State by an HCBS
provider that is located in and designated in New York State.
Submitting Claims for Services When the Child/Youth Is Not Present
Services delivered on behalf of a child/youth to collateral contacts (family members,
caregivers, and other stakeholders identified on the child/youth’s plan of care) without
the child/youth present are allowable and may be billed within the daily limits, if the
service description includes interaction with collateral contacts.
Such services may include sharing techniques and information so the collateral can
better respond to the needs of the child/youth, meetings with employers or prospective
employers regarding the child/youth’s needs, or education and training for family
members/caregivers.
For example, a child/youth receives Day Habilitation services on Mondays and
Wednesdays and is employed at a movie theatre on Tuesdays, Thursdays, and
Fridays. The job coach has a 30-minute meeting with the supervisor at the
movie theatre on a Monday to discuss new job responsibilities for the
child/youth. The service provider may bill for Supported Employment services
for the 30-minutes, even though the child/youth was not present when the
service was delivered and even though the child/youth was receiving another
service (Day Habilitation) at the time that Supported Employment was delivered
on the child/youth’s behalf, this is not considered double billing because the
child/youth is receiving two separate services.
For example, a Caregiver/Family Advocacy and Support Services worker escorts
a family to a destination where the family will implement a strategy supported by
the Caregiver/Family Advocacy and Support Services worker; while in route, the
Caregiver/Family Advocacy and Support Services worker talks through the plan to
help prepare the family. The time spent in transit would be considered part of the
billable service. Transportation is not reimbursable.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 48
Submitting Claims for Non-Sequential Time for the Same Service, on the Same
Day
If the same service is delivered to the same child/youth on the same day but at non-
sequential times, the total time spent on the service must be submitted as a combined
claim.
Timed Units per Encounter of Service
Timed Units per Encounter of Service
Range of Minutes per In-Person Encounter
Billable Minutes
Billable Units (15
Minutes per Unit)
Under 8 minutes
1-7 minutes
Not billable
8-22 minutes
15 minutes
1 unit
23-37 minutes
30 minutes
2 units
38-52 minutes
45 minutes
3 units
53-67 minutes
60 minutes
4 units
68-82 minutes
75 minutes
5 units
83-97 minutes
90 minutes
6 units
98-112 minutes
105 minutes
7 units
113-127 minutes
120 minutes
8 units
Submitting Claims for Daily Billed Services
Services that are billed on a daily basis should be submitted on separate claims.
Claims Coding
The Service Billing Details for each HCBS shows the rate code, CPT code, and modifier
code combinations that are required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
For example, from 10:00am to 10:15am, a job developer meets with a potential
employer about hiring a child/youth receiving supported employment services. If,
later in the same day, provider staff meet with the child/youth and their family
from 1:15 pm to 1:45 pm to discuss the potential new job, the service provider
would document the multiple services provided during the day and bill for a
combined time of 45 minutes (3 units) at the individual fee.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 49
Claims Testing
MMCPs will reach out and offer billing/claim submission training to newly contracted
Children’s HCBS providers and Children’s HCBS providers in active negotiation to
contract. This will include testing claims submission and processing, and issuance of
MMCP contact and support information to assist programs in claim submission.
Children’s HCBS providers are expected to test the claims submission process with
MMCPs for all delivered services prior to the service implementation date and upon
executing a new contract.
Service Combinations
Only certain combinations of Children’s HCBS and State Plan services are allowed by
Medicaid within a child/youth’s current treatment plan. Appendix M has a table showing
the allowable service combinations.
When determining which service should be utilized, MMCPs, providers, families, and
care managers should discuss which services best meet the individual needs of the
child/youth.
Provider Assistance
MMCPs are required to develop and implement provider training and support programs
for network providers. This training and support will allow network providers to gain the
appropriate knowledge, skills, and expertise, and receive technical assistance to comply
with the MMCPs’ requirements. Training and technical assistance shall be provided to
network providers on billing/claims submission, coding, data interface, documentation
requirements, and UM requirements.
Network providers shall be informed in writing regarding the information requirements
for UM decision making, procedure coding and submitting claims. MMCPs will provide
technical assistance in other areas such as claim submission as indicated by provider
performance identified through the quality management and provider profiling programs
put in place by the MMCP. MMCPs will ensure providers receive prompt resolution to
their inquiries.
WHERE T O SUBMIT QUEST IONS AND COMPLAINT S
If you have questions or complaints, please reach out to the following mailboxes:
• Regarding HCBS or the Children’s Health and Behavioral Health System
Transformation generally: BH.Transition@health.ny.gov
• Specific to Medicaid Managed Care and for any type of provider/service:
Managedcarecomplaint@health.ny.gov

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 50
• Specific to a mental health provider/service: OMH-Managed-Care@omh.ny.gov
• Specific to a substance use disorder provider/service: PICM@oasas.ny.gov
• Specific to an OPWDD provider/service: Central.Operations@opwdd.ny.gov
• Specific to a Health Home provider/service: HHSC@health.ny.gov
SERVICE DEFINIT IONS
Overview
As described in the introduction of this Manual, all HCBS have been approved by CMS
through the 1915(c) Children’s Waiver and 1115 MRT Waiver. There are currently 14
services available to children/youth that meet the diagnostic and functional criteria for
HCBS and each service:
1. Community Habilitation
2. Day Habilitation
3. Caregiver/Family Advocacy and Support Services
4. Respite (both Planned and Crisis)
5. Prevocational Services
6. Supported Employment
7. Palliative Care – Expressive Therapy
8. Palliative Care – Massage Therapy
9. Palliative Care – Counseling and Support Services
10. Palliative Care – Pain and Symptom Management

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 51
11. Adaptive and Assistive Technology
12. Vehicle Modifications
13. Environmental Modifications
14. Non-Medical Transportation
Each service has unique requirements. Please review the following sections for more
details on each service including Definition, Service Components, Modality, Setting,
Certification/Provider Qualifications, Training Requirements, and Service Billing Details.
As a reminder, all services need to be properly documented in the participant’s POC
and HCBS Service Plan. Services and staffing should be streamlined whenever
possible, with no more than two practitioners providing HCBS to the child/youth and
family members/caregivers on the same date and at the same time. In addition, care
management is required for all participants receiving HCBS. The HCBS referred and
provided cannot duplicate or replace existing and required care management services
through HH/C-YES. HCBS providers must communicate with HHCM/C-YES regarding
any additional care management needs the participant/family may have; it is then the
HHCM/C-YES’s responsibility to coordinate such related services, as the HCBS
provider cannot provide any HCB Services without the HHCM/C-YES knowledge,
referral, and documented on the POC.
Community Habilitation
Definition
Community Habilitation covers in-person services and supports related to the
child/youth’s acquisition, maintenance, and enhancement of skills necessary to perform
Activities of Daily Living (ADLs), Instrumental Activities of Daily Living (IADLs), and/or
Health-Related Tasks delivered in the community (non-certified) settings.
Acquisition is described as the service available to a child/youth who is seeking greater
independence by learning to perform the task for him or herself. There should be a
reasonable expectation that the individual will acquire the skills necessary to perform
that task within the authorization period.
Maintenance is described as the service available to prevent or slow regression in the
child/youth’s skill level and to prevent loss of skills necessary to accomplish the
identified task.
Enhancement activities are provided to the child through training and demonstration to
promote growth and independence with an already acquired skill level and to support
the child/youth’s goal outside of the training environment.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 52
ADL, IADL, skill acquisition, maintenance, and enhancement are in-person services that
are determined by the person-centered planning process and must be identified in the
child/youth’s POC on an individual or group basis. These identified services will be used
to maximize personal independence and integration in the community, preserve
functioning, and prevent the likelihood of future institutional placement. Skill acquisition,
maintenance, and enhancement services are appropriate for children/youth who have
the capacity to learn to live in the community, with or without support. Community
Habilitation may be delivered in individual or group modality.
Service Components
ADL, IADL skill acquisition, maintenance, and enhancement is related to assistance
with functional skills and may help a child/youth who has difficulties with these types of
skills accomplish tasks related to, but not limited to:
• Self-care
• Life safety
• Medication and health management
• Communication skills
• Mobility
• Community transportation skills
• Community integration
• Appropriate social behaviors
• Problem solving
• Money management
Provider and Condition Requirements
ADL, IADL, skill acquisition, maintenance, and enhancement will be performed by a
direct care worker, who shall include personal care aides, personal attendants, certified
home health aides, direct service professionals who meet the licensure and certification
requirements under NYCRR Title 18, and/or providers approved through OPWDD to
provide Community Habilitation.
ADL, IADL skill acquisition, maintenance, and enhancement must be provided under the
following conditions:
• The need for skills training or maintenance activities has been assessed,
determined, and authorized as part of the person-centered planning process
• Provider agencies of Community Habilitation must develop a Community
Habilitation Service Plan to document the child/youth’s goal(s)/outcome(s),
health/safety needs required during the delivery of the service, and the
necessary staff actions to assist the child/youth reach his/her Community
Habilitation goal(s)/outcome(s), and health/safety needs; the activities are for the
sole benefit of the child/youth and are only provided to the child receiving HCBS
or to the family/caregiver in support of the child/youth
• The activities are designed to preserve or enhance independence or slow/reduce
the loss of independence when the child/youth have a progressive medical

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 53
condition; the activities provided are consistent with the child/youth’s stated
preferences and outcomes in the POC
• The activities provided are coordinated with the performance of ADLs, IADLs,
and health-related tasks
• Training for skill acquisition, maintenance, and enhancement activities that
involve the management of behaviors must use positive enforcement techniques
• The provider is authorized to perform these services for HCBS recipients and has
met any required training, certification, and/or licensure requirements
Some specific ADL services available for training include, but are not limited to:
bathing/personal hygiene; dressing; eating; mobility (ambulation and transferring); and
toileting.
Some specific IADL services available for skills training include, but are not limited to:
managing finances; assisting with transportation (as indicated in the POC); shopping for
food, clothes, and other essentials; preparing meals; assisting with the use of the
telephone and/or other communication devices; managing medications; light
housekeeping; environmental maintenance such as maintaining safe egress; and
laundry.
If the POC indicates that learning how to navigate travel from one location in the
community to another is a goal for the child, this service will include the assistance
provided by a direct care worker to accompany the child/youth while learning the skill.
The in-person service time when a direct care worker is assisting or providing
transportation to an individual may also be billed as part of the Community Habilitation
service.
Health-related tasks are defined as specific tasks related to the needs of a child/youth,
which can be delegated or assigned by licensed healthcare professionals under state
law to be performed by a certified home health aide or a direct service professional.
Health-related tasks also include tasks that home health aides, or a direct service
professional can perform under applicable exemptions from the Nurse Practice Act.
Some specific health-related tasks available for assistance include but are not limited to:
performing simple measurements and tests; assisting with the preparation of complex
modified diets; assisting with a prescribed exercise program; pouring, administering,
and recording medications; assisting with the use of medical equipment, supplies, and
devices; assisting with special skin care; assisting with a dressing change; and assisting
with ostomy care.
Modality
• Individual in-person service
• Group in-person service

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 54
Setting
These services can be delivered at any non-certified, community setting. Such a setting
might include the child/youth’s home, which may be owned or rented, and work setting.
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community-based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network. Family is broadly
defined, and can include families created through birth, foster care, adoption, or a self-
created unit.
Limitations/Exclusions
Please note that this service cannot be substituted for vocational rehabilitation services
provided under the Rehabilitation Act of 1973 or other Children’s HCBS. Approved
settings do not include an OPWDD certified residence, congregate or institutional
settings, a social day care or health care setting in which employees of the particular
setting care for or oversee the child/youth. Foster Care children/youth meeting LOC
may receive these services in a home or community-based setting where they reside
that is not an institution. OCFS Licensed Institutions are defined in New York State
Social Services Law section 427.2(f) as a facility established for the 24-hour care and
maintenance of 13 or more children and operated by a childcare agency (Voluntary
Foster Care Agency).
Only those services not reimbursable under the Community First Choice Option (CFCO)
State Medicaid Plan will be reimbursable under this HCBS Waiver.
Children/youth living in certified settings may only receive this service on weekdays with
a start time prior to 3 pm and are limited to a maximum of six hours of non-residential
services (or its equivalent) daily. For school-age children/youth, this service cannot be
provided during the school day when a child/youth is participating or enrolled in a school
program. Time spent receiving another Medicaid service cannot be counted toward the
Community Habilitation billable service time. This service cannot be delivered nor billed
while a child/youth is in an ineligible setting, such as in a hospital, ICF/IID, or skilled
nursing facility. Community Habilitation services provided under this waiver cannot be
duplicative or delivered at the same time as services otherwise available to a child/youth
through a local educational agency including those services available under the
Individuals with Disabilities Education Act (IDEA) or Rehabilitation Act of 1973.
Certification/Provider Qualifications
Provider Agency Qualifications

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 55
New York State Office for People with Developmental Disabilities (OPWDD) certified,
not-for-profit habilitation provider agencies.
Practitioners must operate in agencies that have been designated through the NYS
Children’s Provider Designation Review Team. This requires that agencies have
appropriate license, certification, and/or approval in accordance with State designation
requirements.
• Provider agencies and practitioners must adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and statutes
• Provider agencies must adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency must ensure that staff receive Mandated Reporting training
prior to service delivery
• The provider agency must ensure that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law, if
applicable
• The provider agency must ensure that any insurance required by the designating
state agency is obtained and maintained
• The provider agency must ensure that any safety precautions needed to protect
the child/youth population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Staff/Agency Qualifications
Providers must have appropriate license, certification, and/or approval in accordance
with State requirements.
OPWDD directs provider agencies to screen staff against the Medicaid Excluded
Provider lists maintained by DOH and the HHS Office of the Inspector General.
Direct support professionals must be employed by the designated agency and have
completed the training stipulated in 14 NYCRR Part 633.8 and the Direct Support
Professionals Core Competencies curriculum.
Additional information can be found in the DSP Core Competencies section of the
OPWDD website.
Training Requirements

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 56
Service Type
Trainings Required
Requirement Completion
Timeframe
Community
Habilitation
• Mandated Reporter
• Prior to service delivery
• Personal Safety/ Safety in the
Community
• Strength Based Approaches
• Suicide Prevention
• Domestic Violence Signs and
Basic Interventions
• Trauma Informed Care
• Training must be completed within
six (6) months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The below table shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers must maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization, the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Community Habilitation
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Community HCBS
Habilitation
8012
H2014
HA
15 minutes
24/day

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 57
Community HCBS
Habilitation -
Group of 2
8013
H2014
HA, UN
15 minutes
24/day
Community HCBS
Habilitation –
Group of 3
8014
H2014
HA, UP
15 minutes
24/day
Guidelines for Medical Necessity Criteria for Children, Adolescents, and Young
Adults
The hours/ billing units are provided as guidance and may be exceeded with additional
review. Factors to be considered regarding higher service levels include other available
paid services. Consideration must also be made for natural supports and individual
needs at the time of the request and included in the assessment and Plan of Care.
Age Range
Typical
Approval
Ranges
Admission and Criteria
Discharge Criteria
Children Ages
0 - 2
0 hours/
0 units per
week
• Skill building typically
met through parental
support/ natural
caregivers and use of
services such as Early
Intervention (EI) and
educational/ school
programs. Services
necessary at this age
typically are provided by
licensed practitioners
including Occupational
Therapy, Physical
Therapy, and Speech
Therapy
• CH should be used as
described and not in lieu
of another, more
appropriate service
• CH will only be
authorized when clear
documentation exists of
a lack of availability of EI
services, EI Respite and/
or other Respite services
and natural supports
(e.g., parent has a
• Child/ youth no longer
meets Level of Care
(LOC) for Home and
Community-based
Services (HCBS); OR
• Child/ youth no longer
wishes to receive the
service or withdraws
consent for the service;
OR
• EI services are made
available; OR
• Child/ youth has
successfully met their
specific goal outlined in
their service plan and no
longer needs this service;
OR
• Child/ youth is no longer
engaged in the service
despite multiple attempts
on the part of the provider
to apply reasonable
engagement strategies;
OR
• Child/ youth moves to a
certified residential setting

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 58
Age Range
Typical
Approval
Ranges
Admission and Criteria
Discharge Criteria
disability and the
provision of CH supports
the child and parent skill
development or the
family has significant
stressors that negatively
impact the ability to
support the child)
Children Ages
3 - 9
0 to 3
hours
per week/
0 to 12
units
per week
• Supports to facilitate
community inclusion,
relationship building, and
adaptive/ social skill
development, when not
available through
Preschool Supportive
Health services, School
Supportive Health
services, or other
Respite services. May
include social skills
groups, music or art
therapy where the child
is working to develop
specific goals on their
person-centered plan
such as appropriate
social interaction and
mimicking others
• CH should be used as
described and not in lieu
of another, more
appropriate service
• CH will only be
authorized when clear
documentation exists of
a lack of availability of
Respite services and
natural supports (e.g.,
parent has a disability
and the provision of CH
supports the child and
parent skill development
or the family has
significant stressors that
negatively impact the
• Child/ youth no longer
meets LOC for HCBS;
OR
• Child/ youth no longer
wishes to receive the
service or withdraws
consent for the service;
OR
• Child/ youth has
successfully met their
specific goal outlined in
their service plan and no
longer needs this service;
OR
• Child/ youth is no longer
engaged in the service,
despite multiple attempts
on the part of the provider
to apply reasonable
engagement strategies;
OR
• Child/ youth moves to a
certified residential setting

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 59
Age Range
Typical
Approval
Ranges
Admission and Criteria
Discharge Criteria
ability to support the
child)
• Not allowed during
school/ educational
hours
Children Ages
10 - 13
0 to 10
hours
per week/
0 to 40
units
per week
• Supports to facilitate
community inclusion,
relationship building, and
adaptive/ social skill
development
• Average hours and need
for CH typically increase
over the years to support
a growing level of
developmental
independence
• Not allowed during
school/ educational
hours
• Child/ youth no longer
meets LOC for HCBS;
OR
• Child/ youth no longer
wishes to receive the
service or withdraws
consent for the service;
OR
• Child/ youth has
successfully met their
specific goal outlined in
their service plan and no
longer needs this service;
OR
• Child/ youth is no longer
engaged in the service,
despite multiple attempts
on the part of the provider
to apply reasonable
engagement strategies;
OR
• Child/ youth moves to a
certified residential setting
Children Ages
14 - 17
0 to 15
hours
per week/
0 to 60
units
per week
• Focus on transition
activities including
increased
independence/ life skill
building including
prevocational type skills
such as riding the bus,
grocery shopping, using
the library,
understanding health
issues, personal
appearance and hygiene
• Not allowed during
school/ educational
hours
• If child/ youth graduates/
discontinues K-12
• Child/ youth no longer
meets LOC for HCBS;
OR
• Child/ youth no longer
wishes to receive the
service or withdraws
consent for the service;
OR
• Child/ youth has
successfully met their
specific goal outlined in
their service plan and no
longer needs this service;
OR
• Child/ youth is no longer
engaged in the service,
despite multiple attempts

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 60
Additional Considerations for Service Authorization Decisions
Other Paid Supports
• Department of Health (DOH) Personal Care and Respite services may
be utilized in many instances. CH should be used as described above
and not in lieu of DOH Personal Care or Respite services or other
available services (e.g., services available through a 1915c waiver).
• CH services can be increased or faded as the individual’s needs,
outcomes, goals and paid and unpaid supports change.
• Individuals with behavioral health issues should be connected to the
appropriate behavioral health and/or crisis services, if available and
appropriate to maximize support.
Natural Supports
• Families in caregiving roles or other naturally supportive living
situations should receive the support needed to assist in creating and
maintaining a stable environment. Relief for family members/
caregivers may be provided through Respite services.
• A family’s capacity to provide natural supports should be evaluated,
with additional support being required if the family situation is
destabilized due to mental health issues, the death of a family member
or other stressors.
• Additional support may also be required as the primary caregiver ages
or when multiple members of the family require the support of a single
caregiver.
Individual Needs
• Individuals may require reassessment when they:
o Have significant/ complex medical or behavioral needs and are not
presenting as clinically stable; OR
o Have frequent use of hospital emergency rooms and inpatient
services; OR
o Require heightened levels of supervision such as being within line
of sight or 1:1 within arm’s length for safety
• Individualized support models may need a blend of DOH Personal
Care, Respite services, and CH.
Note: OPWDD Community Habilitation provider agencies are bound by MHL § 13.01 and MHL §
1.03(22) to only provide the Community Habilitation service to individuals with intellectual and
developmental disabilities (I/DD). These approved provider agencies are not allowed to provide the
service to individuals without an I/DD.
Age Range
Typical
Approval
Ranges
Admission and Criteria
Discharge Criteria
education services, CH
can increase to meet
additional need for skill
building.
on the part of the provider
to apply reasonable
engagement strategies;
OR
• Child/ youth moves to a
certified residential setting

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 61
Day Habilitation
Definition
Assistance with acquisition, retention or improvement in self-help, socialization and
adaptive skills including communication, and travel that regularly takes place in a non-
residential setting, separate from the person's private residence or other residential
arrangement. Activities and environments are designed to foster the acquisition of skills,
appropriate behavior, greater independence, community inclusion, relationship building,
self-advocacy, and informed choice. Day Habilitation (DH) services must be provided to
a child/youth at an OPWDD certified setting typically between the daytime hours of 9
a.m. and 3 p.m.
Service Components
Individual Day Habilitation (a one-to-one, individual-to-worker provided service with an
hourly unit of service) and Group Day Habilitation services are furnished four or more
hours per day on a regularly scheduled basis for one or more days per week or less
frequently as specified in the participant's POC. Meals provided as part of these
services shall not constitute a "full nutritional regimen" (three meals per day).
A supplemental version of Individual and Group Day Habilitation is available for
children/youth who do not reside in a certified setting. The supplemental Day
Habilitation is provided outside the 9 a.m. to 3 p.m. weekday time period and includes
later afternoon, evenings, and weekends. Day Habilitation and Supplemental Day
Habilitation services cannot be delivered at the same time.
All Day Habilitation services (Group and Individual) have the same service description
and focus on enabling the participant to attain or maintain his or her maximum
functional level and shall be coordinated with any physical, occupational, or speech
therapies in the POC. In addition, Day Habilitation services may serve to reinforce skills,
behaviors, or lessons taught in other settings. Provider agencies of Day Habilitation
must develop a Day Habilitation service plan to document the child/youth’s
goal(s)/outcomes(s), health/safety needs required during the delivery of the service, and
the necessary staff actions to assist the child/youth in reaching his/her Day Habilitation
goal(s)/outcomes(s), and health/safety needs.
Modality
• Individual in-person service
• Group in-person service
Setting
Day Habilitation (DH) services are provided to a child at an OPWDD certified setting.
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 62
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration.
Limitations/Exclusions
Group and Individual DH cannot be billed as overlapping services. Any child/youth
receiving HCBS under this waiver may receive this service. Service necessity criteria for
this service requires that the child/youth must have a developmental delay justifying the
need for the provision of Day Habilitation, but the child/youth may meet NF, ICF/IID, or
Hospital LOC.
Day Habilitation services will not include funding for direct, hands-on physical therapy,
occupational therapy, speech therapy, nutrition, or psychology services.
Children/youth have a maximum daily amount of services that are available to
individuals based upon their residence. Individuals residing in certified settings are
limited to a maximum of six hours of non-residential services (or its equivalent) which
must commence no later than 3 p.m. on weekdays.
Supplemental DH services are those services provided on weekends and/or on
weekdays with a service start time after 3 p.m. Supplemental DH services are not
available to individuals residing in certified residential settings with paid, professional
staff, because the certified residential habilitation provider is responsible for the
habilitation needs of the individual on weekday evenings and anytime on weekends.
Certification/Provider Qualifications
Provider Agency Qualifications
New York State Office for People with Developmental Disabilities (OPWDD) Regional
Office or non-profit organization certified by OPWDD.
OPWDD Regional Office
• OPWDD Regional Offices may provide Day Habilitation HCBS waiver services
directly through its Regional Offices
• OPWDD directs provider agencies to screen staff against the Medicaid Excluded
Provider lists maintained by DOH and the HHS Office of the Inspector General
Non-Profit Organization
• Certified by OPWDD to provide Day Habilitation
• OPWDD directs provider agencies to screen staff against the Medicaid Excluded
Provider lists maintained by DOH and the HHS Office of the Inspector General
• Non-profit organizations include nonprofit corporations formed under New York
State Law or authorized to do business in New York, local government units, or
organizations created by an act of the New York State Legislature for charitable

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 63
purposes, which include providing services to persons with developmental
disabilities
• If the provider agency employs professional clinical staff, that staff person must
have the appropriate credentials stipulated by the OPWDD and/or the NYS
Department of Education under the following regulations and laws:
o Nursing (8 NYCRR Part 64 and Education Law Title 8, Article 139)
o Speech Language Pathologist (8 NYCRR Part 75 and Education Law Title
8, Article 159)
o Psychology (8 NYCRR Part 72 and Education Law Title 8, Article 153)
o Social Work (8 NYCRR Part 74 and Education Law Title 8, Article 154)
o Rehab Counselor (14 NYCRR Part 679.99)
o Dietetics/Nutrition (8 NYCRR Part 79 and Education Law Title 8, Article
157)
o Occupational Therapy (8 NYCRR Part 76 and Education Law Title 8,
Article 156)
o Physical Therapy (8 NYCRR part 77 and Education Law Title 8, Article
136)
o Applied Behavioral Sciences Specialist (8 NYCRR Part 79 and Education
Law Title 8, Article 167)
o Behavioral Intervention Specialist (14 NYCRR part 633-16.b(32))
Practitioners must operate in agencies that have been designated through the NYS
Children’s Provider Designation Review Team. This requires agencies to have
appropriate license, certification, and/or approval in accordance with State designation
requirements.
• Provider agencies and practitioners must adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and statutes
• Provider agencies must adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency must ensure that staff receive Mandated Reporting training
which is provided throughout New York State and Personal Safety in the
Community training prior to service delivery
• The provider agency must ensure that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law, if
applicable
• The provider agency must ensure that any insurance required by the designating
state agency is obtained and maintained
• The provider agency must ensure that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 64
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Staff/Agency Qualifications
• Providers must have appropriate license, certification, and/or approval in
accordance with State requirements
• Direct support professionals must have completed the training stipulated in 14
NYCRR Part 633.8 and the Direct Support Professionals Core Competencies
curriculum
Additional information can be found in the DSP Core Competencies section of the
OPWDD website.
Training Requirements
Service Type
Trainings Required
Requirement Completion
Timeframe
Day
Habilitation
• Mandated Reporter
• Prior to Service Delivery
• Personal Safety/ Safety in the
Community
• Strength Based Approaches
• Suicide Prevention
• Domestic Violence Signs and
Basic Interventions
• Trauma Informed Care
• Training must be completed within
six (6) months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Descriptions
The table below shows the rate code, CPT code, and modifier code combinations that
will be required under Medicaid Managed Care. Providers will use these coding
combinations to indicate to the MMCP that the claim is for a children/youth service and
is to be paid at the government rate. The procedure and modifier code combinations
must be adhered to by both provider and MMCP to ensure appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 65
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization, the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Day Habilitation
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Day HCBS
Habilitation
7933
T2020
HA
15 minutes
24/day
Day HCBS
Habilitation -
Group of 2
7934
T2020
HA, UN
15 minutes
24/day
Day HCBS
Habilitation -
Group of 3
7935
T2020
HA, UP
15 minutes
24/day
Caregiver/Family Advocacy and Support Services
Definition
Caregiver/Family Advocacy and Support Services enhance the child/youth’s ability,
regardless of disability (developmental, physical, and/or behavioral), to function as part
of a caregiver/family unit and enhance the caregiver/family’s ability to care for the
child/youth in the home and/or community as well as, provides the child/youth, family,
caregivers, and collateral contacts (family members, caregivers, and other stakeholders
identified on the child/youth’s POC) with techniques and information not generally
available so that they can better respond to the needs of the participant. These services
are intended to assist the child/youth, family/caregiver, and collateral contacts in
understanding and addressing the participant’s needs related to their disability(ies).
The use of this service may appropriately be provided to prevent problems in
community settings when the child/youth is experiencing difficulty.
The POC objectives must clearly state how the service can prevent as well as
ameliorate existing problems and to what degree. This service cannot be used to
develop an Individualized Education Program (IEP), the plan for students with
disabilities who meet the federal and state requirements for special education, or to
provide special education services to the child/youth. Participating in community events
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 66
and integrated interests/occupations are important activities for all children/youth,
including those with disabilities (developmental, physical, and/or behavioral health in
origin). Success in these activities is dependent not only on the child/youth, but on the
people, who interact with and support the child/youth in these endeavors.
Caregiver/Family Advocacy and Support Services improve the child/youth’s ability to
gain from the community experience and enables the child/youth’s environment to
respond appropriately to the child/youth’s disability and/or healthcare issues.
Note: This service is not the State Plan service of Family Peer Support Services which
must be delivered by a certified/credentialed Family Peer with lived experience.
Service Components
Based upon the Caregiver/Family Advocacy and Support Services plan developed by
the child/youth and caregiver/family team; this service provides opportunities to:
• Interact and engage with family/caregivers and children/youth to offer
educational, advocacy, and support resources to develop family/caregivers’
ability to independently access community services and activities
• Maintain and encourage the caregivers’/families’ self-sufficiency in caring for the
child/youth in the home and community
• Address needs and issues of relevance to the caregiver/family unit as the
child/youth is supported in the home and community
• Educate and train the caregiver/family unit on available resources so that they
might better support and advocate for the needs of the child and appropriately
access needed services
• Provide guidance in the principles of children’s chronic condition or life-
threatening illness
• Training (one-on-one or group) for the child/youth and/or the family/caregiver
regarding methods and behaviors to enable success in the community; each
group must not exceed 12 participants (enrollees and collaterals)
• Direct self-advocacy training in the community with collateral contacts regarding
the child/youth’s disability(ies) and needs related to his or her health care issues
• Self-advocacy training for the child/youth and/or family/caregiver, including during
community transitions
When outlined in the child/youth’s POC, the service can be delivered to multiple family
members or other identified resources for the child/youth by more than one practitioner
to address the child/youth’s needs by educating, engaging, and guiding their families to
ensure that the child/youth and family’s needs are met. In instances where two
practitioners are required to meet the needs of the child/family, and the encounters
occur at the same date and time, the agency can bill for both practitioners in one claim
by adding the time the service was delivered by each practitioner into a combined claim.
If one practitioner delivers the services to a child/youth and/or multiple family members/
resources at the same date and time, the claim should reflect the exact time spent as a
single encounter.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 67
Modality
• Individual in-person intervention
• Group in-person intervention (no more than three HCBS eligible children/families)
Note: Services can be delivered with or without the child/youth present.
Setting
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community- based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network, family is broadly
defined, and can include families created through birth, foster care, adoption, or a self-
created unit.
Limitations/Exclusions
• This service cannot be delivered or billed while an enrolled child/youth is in an
ineligible setting, including hospitalization
• Caregiver/Family Advocacy and Support Services cannot duplicate or replace
special education and related services that are otherwise available to the
individual through a local educational agency, under the provisions of the
Individuals with Disabilities Education Act (IDEA)
• Caregiver/Family Advocacy and Support Services cannot duplicate or replace
existing and required care management services provided through HH/C-YES
• Caregiver/Family Advocacy and Support Services are limited to six hours per day
Certification/Provider Qualifications
Provider Agency Qualifications
Practitioners must operate in agencies that have been designated through the NYS
Children’s Provider Designation Review Team. This requires that agencies have
appropriate license, certification, and/or approval in accordance with State designation
requirements.
• Provider agencies and practitioners must adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and statutes
• Provider agencies must adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency must ensure that staff receive Mandated Reporting training
prior to service delivery

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 68
• The provider agency must ensure that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law, if
applicable
• The provider agency must ensure that any insurance required by the designating
state agency is obtained and maintained
• The provider agency must ensure that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Staff Qualifications:
• Level 1 Minimum Qualifications: Requires a high school diploma, high school
equivalency preferred or a State Education Commencement Credential (e.g.,
SACC or CDOS) with related human service experience
• Level 1 Preferred Qualifications: Experience working with children/youth
• Level 2 Minimum Qualifications: Requires a bachelor’s degree plus two years
of related experience
• Level 2 Preferred Qualifications: Requires a master’s degree in education, or a
master’s degree in a human services field plus one year of applicable experience
Supervisor Qualifications:
• Level 1 Minimum Qualifications: Requires a bachelor’s degree with one year of
experience in human services working with children/youth
• Level 1 Preferred Qualifications: Two years’ experience in human services
working with children/youth
• Level 2 Minimum Qualifications: Requires a master’s degree with one year of
experience or a bachelor’s degree with four years of experience in human
services working with children/youth
Level 2 Preferred Qualifications: Master’s degree with two years of experience
in human services working with children/youth
Training Requirements
Service Type
Trainings Required
Requirement Completion
Timeframe
Caregiver/Family
Advocacy and
Support
Services
• Mandated Reporter
• Prior to Service Delivery
• Personal Safety/ Safety in the
Community
• Strength Based Approaches
• Suicide Prevention
• Domestic Violence Signs and
Basic Interventions
• Training must be completed
within six (6) months of hire
date.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 69
Service Type
Trainings Required
Requirement Completion
Timeframe
• Trauma Informed Care
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The table below shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization, the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Caregiver/Family Advocacy and Support Services
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Caregiver/Family
Advocacy and
Support Services
– L1 Individual
8003
H2014
UK, HA
15 minutes
24/day

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 70
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Caregiver/Family
Advocacy and
Support Services
– L1 Group of 2
8004
H2014
HA, UK,
UN
15 minutes
24/day
Caregiver/Family
Advocacy and
Support Services
– L1 Group of 3
8005
H2014
HA, UK,
UP
15 minutes
24/day
Caregiver/Family
Advocacy and
Support Services
– L2 Individual
8009
H2015
HA
15 minutes
24/day
Caregiver/Family
Advocacy and
Support Services
– L2 Group of 2
8010
H2015
HA, UN
15 minutes
24/day
Caregiver/Family
Advocacy and
Support Services
– L2 Group of 3
8011
H2015
HA, UP
15 minutes
24/day
Respite
Definition
This service focuses on short-term assistance provided to children/youth, regardless of
disability (developmental, physical and/or behavioral), because of the absence of or
need for relief of the child/youth or the child/youth’s family caregiver. Such services can
be provided in a planned mode or delivered in a crisis situation. Respite workers
supervise the child/youth and engage the child/youth in activities that support his/her
and/or primary caregiver/family’s constructive interests and abilities.
Respite providers offer services with a level of expertise in understanding and
implementing behavioral/developmental interventions required to support optimal
functioning for children/youth. Respite providers regularly communicate the details of
the child/youth’s intervention plan so that there is a carryover of skill from the respite
source to the caregivers and treatment providers.
Service Components
Planned
Planned Respite services provide planned short-term relief for the child/youth or
family/primary caregivers to enhance the family/primary caregiver’s ability to support the
child/youth’s functional, developmental, behavioral health, and/or health care needs.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 71
The service is direct care for the child/youth by individuals trained to support the
child/youth’s needs. This support may occur in short-term increments of time (usually
during the day) or on an overnight or longer-term increment. Planned Respite activities
support the POC goals and include providing supervision and activities that match the
child/youth's developmental stage and continue to maintain the child/youth health and
safety.
Respite services may be delivered in a home or residence by qualified practitioners,
out-of-home/residence by staff in community-based sites (e.g., community centers,
camps, parks), or in allowable facilities.
Crisis
Crisis Respite is a short-term care and intervention strategy for children/youth and their
families that helps to alleviate the risk for an escalation of symptoms, a loss of
functioning, and/or a disruption in a stable living environment. It may be used when
challenging behavioral or situational crises occur that the child/youth and/or
family/caregiver is unable to manage without intensive assistance and support. Crisis
Respite can also be used for crisis intervention or from visiting the emergency room.
Crisis Respite should be included on the POC to the extent that it is an element of the
crisis plan or risk mitigation strategy. Crisis Respite should only be used in response to
an immediate crisis.
Crisis Respite services may be delivered in a home or residence by qualified
practitioners, out-of-home/residence by staff in community-based sites, or in allowable
facilities. Services offered may include site-based crisis residence, monitoring for high-
risk behavior, health and wellness skill building, wellness activities, family/caregiver
support, conflict resolution, and other services as needed.
Ongoing communication between child/youth or the family/primary caregiver receiving
Crisis Respite for their child, the Crisis Respite staff, and the child/youth’s established
behavioral health and healthcare providers is required to assure collaboration and
continuity in managing the crisis situations and identifying subsequent support and
service needs.
At the conclusion of a Crisis Respite period, Crisis Respite staff, together with the
child/youth and family/primary caregiver, and his or her established behavioral health or
health care providers when needed, will make a determination as to the continuation of
necessary care and make recommendations for modifications to the child’s POC.
Children/youth are encouraged to receive Crisis Respite in the most integrated and
cost-effective settings appropriate to meet their respite needs. Out-of-home Crisis
Respite is not intended as a substitute for permanent housing arrangements.
Modality
Planned Day Respite, Planned Overnight Respite, Crisis Day Respite, Crisis Overnight
Respite:

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 72
These services may be delivered with support of staffing ratios necessary to keep the
child/youth, and other children/youth in the environment, safe and as indicated in the
child/youth’s POC overseen by the Respite provider.
Overnight Respite is defined as Respite services provided to a person on two
consecutive days when Respite staff are providing oversight to a participant during
nighttime hours. Overnight Respite should follow the general limits for respite (see
below).
Overnight Respite should be used in instances to enhance the family/primary
caregiver’s ability to support the child/youth’s functional, developmental, behavioral
health, and/or health care needs or to help alleviate the risk for an escalation of
symptoms, a loss of functioning, and/or a disruption in a stable living environment.
Overnight Respite is not a substitute for childcare.
Setting
Planned or Crisis Day Respite services can be provided in the home of an eligible
child/youth or a community setting. Community settings may include areas where a
child/youth lives, attends school, works, engages in services and/or socializes and is in
compliance with CMS Final Rule (§441.301(c)(4) and (§441.710), HCBS Settings Rule
(Appendix B).
Note: a provider can be designated for Crisis or Planned Respite without an overnight
setting; however, they will only be authorized to provide Respite that does not include
an overnight stay or overnight service provision. If the Respite service is provided
overnight, it can only be done so in an authorized overnight setting, and that setting
must be a licensed/certified facility as outlined below.
Planned or Crisis Overnight Respite settings include those licensed or certified by
OCFS, OMH, or OPWDD and designated to provide Respite services. Please note
there is an exemption in the CMS HCBS Final Rule (March 16, 2014) for allowable
Respite care settings.
• OMH licensed Community Residence (community-based or state-operated),
including Crisis Residence, which has an OMH Operating Certificate
demonstrating compliance with 14 NYCRR 594
• OCFS Licensed agency boarding home, a group home, a group residence, or an
institution and certified foster boarding homes
• OPWDD certified residential setting where the individual does not permanently
reside (i.e., Family Care Home; Intermediate Care Facility for Individuals with
Intellectual and Developmental Disabilities (ICF/IDD); Individualized Residential
Alternative (IRA) or Community Residence (CR); or Free-Standing Respite
facility under the auspices of OPWDD)

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 73
Limitations/Exclusions
• Services to children/youth in foster care must comply with Part 435 of 18
NYCRR. Respite is not an allowable substitute for permanent housing
arrangements.
• For Respite services that may be provided as crisis or overnight, Federal
Financial Participation is not claimed for the cost of room and board except when
provided as part of respite care furnished in a facility approved by the State that
is not a private residence.
• It is the responsibility of the HHCM/C-YES upon referral to ensure that Respite
providers have adequate training and knowledge to address the individual
child/youth’s needs (including but not limited to physical and/or medical needs
such as medications or technology), OR have made arrangements for an
appropriately trained and knowledgeable individual to address the individual
child/youth’s needs (including but not limited to physical and/or medical needs
such as medications or technology). Examples include arrangement of an
approved Private Duty Nurse for a technology dependent child/youth while in a
Respite setting.
• Respite is not a substitute for child care and should only be used in instances to
enhance the family/primary caregiver’s ability to support the child/youth’s
functional, developmental, behavioral health, and/or health care needs. The
needs of the child/youth should be driving this service and not the availability of
the family/primary caregiver to supervise the child/youth. For example,
accompanying a child/youth to a community activity at a local park from 5 PM – 7
PM would be billable if aligned with the child/youth’s POC and in alignment with
the f/s/d outlined in the HCBS Service Plan, whereas the provider staying in the
home from 8 PM – 10 PM to provide supervision after bedtime would not be
billable.
Certification/Provider Qualifications
Provider Agency Qualifications
Practitioners must operate in agencies that have been designated through the NYS
Children’s Provider Designation Review Team. This requires that agencies have
appropriate license, certification, and/or approval in accordance with State designation
requirements.
• Provider agencies and practitioners must adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and statutes.
• Provider agencies must adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency must ensure that staff receive Mandated Reporting training
prior to service delivery

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 74
• The provider agency must ensure that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law if
applicable
• The provider agency must ensure that any insurance required by the designating
state agency is obtained and maintained
• The provider agency must ensure that any safety precautions needed to protect
the child/youth population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.
For Overnight Planned or Crisis Respite, the designated provider must meet the
Provider Agency Qualifications above AND must be one of the following:
• OMH-certified Community Residence: (community-based or State-operated)
including Crisis Residence
• OCFS licensed/certified setting including agency boarding home, a group home,
a group residence, or an institution
• OPWDD certified residential setting
Individual Staff Qualifications
• Provision of service in child’s residence or other community-based setting
(e.g., park, shopping center, etc.)
o Respite providers are paraprofessionals with a high school diploma or
equivalent and with appropriate skills and training. It is the responsibility of the
HHCM/C-YES to ensure that providers have adequate training and
knowledge to address the individual child/youth’s needs (including but not
limited to physical and/or medical needs such as medications or technology).
▪ Experience working with children/youth (preference given to those with
experience working with children/youth with special needs)
▪ A high school diploma, high school equivalency preferred or a State
Education Commencement Credential (e.g. SACC or CDOS)
• Provision of service outside child/youth’s residence and in an allowable
licensed/certified setting
o In a foster boarding home: Respite providers must be a Licensed Foster
Parent pursuant to Part 435 of 18 NYCRR
o In a OCFS licensed/certified setting: Respite providers are paraprofessionals
with a high school diploma or equivalent and with appropriate skills and
training
o In an OMH-certified Community Residence: (community-based or State-
operated), including Crisis Residence, which has an OMH Operating
Certificate demonstrating compliance with 14 NYCRR 594: Respite workers
must be staff of the licensed program

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 75
o In an OPWDD-certified setting: (community-based or State-operated), Family
Care Home, Intermediate Care Facility for Individuals with Intellectual and
Developmental Disabilities (ICF/IDD); Individualized Residential Alternative
(IRA) or Community Residence (CR); or Free-Standing Respite facility under
the auspices of OPWDD; Respite workers must be staff of the certified
program.
Supervisor Qualifications
Minimum Qualifications: An individual with a bachelor's degree and one year of
experience in human services working with children/youth
Training Requirements
Service Type
Trainings Required
Requirement Completion Timeframe
Respite
(Crisis/Planned)
• Mandated Reporter
• Prior to Service Delivery
• Personal Safety
• Safety in the Community
• Strength Based
Approaches
• OMH-recommended
Suicide Prevention
• Domestic Violence Signs
and Basic Interventions
• Trauma Informed Care
• Training must be completed within six
(6) months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The two tables below show the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 76
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization, the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Respite - Planned
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Planned Respite -
Individual
(up to 6 hours)
8023
S5150
HA
15 minutes
24/day
Planned Respite -
Individual per
diem
(over 6 up to 12
hours)
8024
S5151
HA
Per Diem
1/day
Planned Respite –
Individual per
diem
(over 12 up to 24
hours)
8025
S5151
HA, HK
Per diem
1/day
Planned Respite -
Group per diem
(over 6 up to 12
hours)
8026
S5150
HA, HK,
HQ
Per diem
1/day
Planned Respite -
Group
(up to 6 hours)
8027
S5150
HA, HQ
15 minutes
24/day
Respite - Crisis
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Crisis Respite –
(up to 6 hours)
8028
S5150
HA, ET
15 minutes
24/day
Crisis Respite -
8029
S5151
HA, ET
Per Diem
1/day

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 77
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
(over 6 up to 12
hours)
Crisis Respite -
Individual
(over 12 up to 24
hours)
8030
S5151
HA, ET,
HK
Per Diem
1/day
Annual units for Planned and Crisis Respite are limited to 14 days (full per diems)
during the calendar year or 1,344 15-minute units annually. The cumulative total hours
of all Planned and Crisis Respite services received may not exceed the 14 day/1,344
15- minute unit annual amount without medical necessity documented in the child’s
case record. If the child is enrolled in a MMCP, approval from the MMCP must also be
documented in the child’s case record.
The following are examples of permissible Respite billing combinations (total 1,344 15-
minute units OR 14 per diems during the calendar year):
• 48 15-minute units/week for 28 weeks
• One 24-hour per diem units and 22 15-minute units/week for 52 weeks with 104
additional 15-minute units to be used throughout the year
• 24 hours for 14 days
Guidance on Per Diem Billing
It is permissible to provide and bill for another HCBS while overnight Respite is also
provided at the full per diem rate during the same day, provided that the child/youth is in
the care of the Respite provider for at least 12 cumulative hours. For example, a
provider can bill for the per diem Crisis Respite rate while the child/youth attends a
necessary and/or regularly scheduled medical appointment, provided that the
child/youth is in the care of the Crisis Respite provider for at least 12 cumulative hours
outside of the time the child/youth spent at the medical appointment. If the child/youth is
in the direct care of the Respite provider for less than 12 cumulative hours while
receiving other services (e.g., medical services/appointments), then the 6 – 12 hour or
up to 6 hour rate should be billed. Providers must properly document why the break in
service was needed and necessary during the provision of overnight respite.
As indicated in the Respite limit guidance noted above, the total Planned and Crisis
Respite claims cannot total more than 336 hours within the calendar year.
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 78
Prevocational Services
Definition
Prevocational Services are individually designed to prepare a youth (age 14 or older) to
engage in paid work, volunteer work, or career exploration. Prevocational Services are
not job-specific, but rather are geared toward facilitating success in any work
environment for youth whose disabilities do not permit them access to other
prevocational services. The service will be reflected in youth’s POC and must be
directed to teaching skills rather than explicit employment objectives. In addition,
Prevocational Services assist with facilitating appropriate work habits, acceptable job
behaviors, and learning job production requirements.
Service Components
Prevocational Services may include volunteer work, such as learning and training
activities that prepare a person for entry into the paid workforce. Prevocational Services
should enable each participant to attain the highest level of work in the most integrated
setting and with the job matched to the participant’s interests, strengths, priorities,
abilities, and capabilities, while following applicable federal wage guidelines from the
U.S. Department of Labor. Services are intended to develop and teach general skills.
Examples include, but are not limited to:
• Ability to communicate effectively with supervisors, co-workers, and customers
• Generally accepted community workplace conducts and dress
• Ability to follow directions
• Ability to attend to and complete tasks
• Punctuality and attendance
• Appropriate behaviors in and outside the workplace
• Workplace problem solving skills and strategies
• Mobility training
• Career planning
• Proper use of job-related equipment and general workplace safety
Prevocational Services include activities that are not primarily directed at teaching skills
to perform a particular job, but at underlying habilitative goals (e.g., attention span,
motor skills, interpersonal relations with co-workers and supervisors) that are associated
with building skills necessary to perform work and optimally to perform competitive,
integrated employment.
• Resume writing, interview techniques, role play, and job application completion
• Exploring career options, facilitating appropriate work habits, acceptable job
behaviors, and learning job production requirements
• Assisting in identifying community service opportunities that could lead to paid
employment
• Helping youth to connect their educational plans to future career/vocational goals
• Helping youth to complete college, technical school, or other applications to
continue formal education/training

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 79
• Helping youth to apply for financial aid or scholarship opportunities
Documentation is maintained that the service is not available under a program funded
under Section 110 of the Rehabilitation Act of 1973 or the IDEA (20 U.S.C. 1401 et
seq.).
Modality
This service may be delivered in a one-to-one session or in a group setting of two or
three participants.
Setting
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community-based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network, family is broadly
defined, and can include families created through birth, foster care, adoption, or a self -
created unit.
Limitations/Exclusions
Documentation is maintained that the service is not available under a program funded
under Section 110 of the Rehabilitation Act of 1973 or the IDEA (20 U.S.C. 1401 et
seq.).
Prevocational services will not be provided to an HCBS participant if:
• Special education and related services are otherwise available to the individual
through a local educational agency, under the provisions of the Individuals with
Disabilities Education Act (IDEA), and the provision of HCBS Prevocational
services would be duplicative of such services.
• Vocational rehabilitation services are otherwise available to the individual
through a program funded under section 110 of the Rehabilitation Act of 1973
(Access VR), and the provision of HCBS Prevocational services would be
duplicative of such services.
• Vocational services are provided in facility-based work settings that are
not integrated settings in the general community workforce.
Certification/Provider Qualifications
Provider Agency Qualifications
Practitioners must operate in agencies that have been designated through the NYS
Children’s Provider Designation Review Team. This requires agencies have appropriate
license, certification and/or approval in accordance with State designation requirements.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 80
• Provider agencies and practitioners must adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and statutes
• Provider agencies must adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency must ensure that staff receive Mandated Reporting training
prior to service delivery
• The provider agency must ensure that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law if
applicable
• The provider agency must ensure that any insurance required by the designating
state agency is obtained and maintained
• The provider agency must ensure that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Qualifications
• Minimum Qualifications: An individual with an associate’s degree and one year
of human service experience
• Preferred Qualifications: Bachelor’s degree with one year of experience in
human services working with children/youth
Supervisor Qualifications
• Minimum Qualifications: An individual with a bachelor's degree and three
years of experience in human services
• Preferred Qualifications: Master’s degree with one year of experience in human
services working with children/youth
Training Requirements
Service Type
Trainings Required
Requirement Completion Timeframe
Prevocational
Services
• Mandated Reporter
• Prior to Service Delivery
• Personal Safety/
Safety in the
Community
• Training must be completed within
six (6) months of hire date.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 81
Service Type
Trainings Required
Requirement Completion Timeframe
• Strength Based
Approaches
• Suicide Prevention
• Domestic Violence
Signs and Basic
Interventions
• Trauma Informed
Care
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The table below shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Prevocational Services
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Prevocational
Services -
Individual
8006
T2015
HA
15 Minutes
8/day

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 82
Prevocational
Services - Group
of 2
8007
T2015
HA, UN
15 Minutes
8/day
Prevocational
Services - Group
of 3
8008
T2015
HA, UP
15 Minutes
8/day
Supported Employment
Definition
Supported Employment services are individually designed to prepare youth with
disabilities (age 14 or older) to engage in paid work. Supported Employment services
provide assistance to participants with disabilities as they perform in a work setting.
Supported Employment provides ongoing supports to participants who, because of their
disabilities, need intensive on-going support to obtain and maintain an individual job in
competitive or customized employment, or self-employment, in an integrated work
setting in the general workforce for which an individual is compensated at or above the
minimum wage, but not less than the customary wage and level of benefits paid by the
employer for the same or similar work performed by individuals without disabilities. The
outcome of this service is sustained paid employment at or above the minimum wage in
an integrated setting in the general workforce, in a job that meets personal and career
goals.
Supported Employment services are individualized and may include any combination of
the following services: vocational/job-related discovery or assessment, person-centered
employment planning, job placement, job development, negotiation with prospective
employers, job analysis, job carving, training and systematic instruction, job coaching,
benefits support, training and planning, transportation, career advancement services,
and other workplace support services including services not specifically related to job
skill training that enable the participant to successfully integrate into the job setting.
Supported Employment services may also include services and supports that assist the
participant in achieving self-employment through the operation of a business including
home-based self-employment. However, Medicaid funds are not used to defray the
expenses associated with starting up or operating a business.
In addition to the need for an appropriate job match that meets the individual’s skills and
interests, individuals may also need long term employment support to successfully
maintain a job due to the ongoing nature of the HCBS participant’s support needs,
changes in life situations, or evolving and changing job responsibilities.
Service Components
Supported employment services may be provided in a variety of settings, particularly
work sites. Supported employment services include the following:

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 83
• Supervision and training that are not job-related
• Intensive ongoing support
• Transportation to and from the job site
• Interface with employers regarding the individual’s disability(ies) and needs
related to healthcare issue(s)
• Other activities needed to sustain paid work (e.g., employment assessment, job
placement, and/or adaptive/assistive equipment and/or technology necessary for
employment)
• Job finding and development training in work behaviors
• Assessing the interest and fit of an individual for particular job opportunities,
staff work with employers and job sites preparing them to be able to make
necessary and reasonable accommodations
• On-site support for the individual as they learn specific job tasks
• Monitoring through on-site observation and through c ommunication with job
supervisors and employers
Modality
• Individual in-person intervention
Setting
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community-based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network, family is broadly
defined, and can include families created through birth, foster care, adoption, or a self -
created unit.
Limitations/Exclusions
Medicaid funds may not be used to defray the expenses associated with starting up or
operating a business.
Supported Employment service will not be provided to an HCBS participant if:
• Special education and related services are otherwise available to the individual
through a local educational agency, under the provisions of the Individuals with
Disabilities Education Act (IDEA), and the provision of Supported Employment
would be duplicative of such services.
• Vocational rehabilitation services are otherwise available to the individual through
a program funded under section 110 of the Rehabilitation Act of 1973, and the
provision of Supported Employment would be duplicative of such services.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 84
• Supported employment does not include facility based, or other similar types of
vocational services furnished in specialized facilities that are not a part of the
general workplace.
• Supported employment does not include payment for supervision, training,
support, and/or adaptations typically available to other workers without
disabilities filling similar positions in the business.
• Supported employment does not include volunteer work. Such volunteer learning
and un-paid training activities that prepare a person for entry into the paid
workforce are addressed through Prevocational services.
Medicaid funding cannot be claimed for incentive payments, subsidies, or unrelated
vocational training expenses such as the following:
• Incentive payments made to an employer to encourage or subsidize the
employer’s participation in Supported Employment
• Payments that are passed through to users of Supported Employment services
Supported Employment is limited to three hours per day.
Certification/Provider Qualifications
Provider Agency Qualifications
Practitioners must operate in agencies that have been designated through the NYS
Children’s Provider Designation Review Team. This requires agencies have appropriate
license, certification, and/or approval in accordance with State designation
requirements.
• Provider agencies and practitioners must adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and statutes
• Provider agencies must adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency must ensure that staff receive Mandated Reporting training
prior to service delivery
• The provider agency must ensure that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law, if
applicable
• The provider agency must ensure that any insurance required by the designating
State agency is obtained and maintained
• The provider agency must ensure that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 85
Individual Qualifications
• Minimum Qualifications: An individual with an Associate’s degree and one
year of human service experience
• Preferred Qualifications: Bachelor’s degree with one year of experience in
human services working with children/youth
Supervisor Qualifications
• Minimum Qualifications: An individual with a Bachelor’s degree and three years
of experience in human services
• Preferred Qualifications: Master’s degree with one year of experience in human
services working with children/youth
Training Requirements
Service Type
Trainings Required
Requirement Completion Timeframe
Supported
Employment
• Mandated Report
• Prior to Service Delivery
• Personal Safety/ Safety in
the Community
• Strength Based
Approaches
• OMH-recommended
Suicide Prevention
• Domestic Violence Signs
and Basic Interventions
• Trauma Informed Care
• Training must be completed within six (6)
months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The table below shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 86
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Supported Employment is billed as one service and can be delivered with or without the
child/youth present.
Supported Employment
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Supported
Employment
8015
H2023
HA
15 minutes
12/day
Palliative Care – Expressive Therapy
Definition
Palliative Care is specialized medical care focused on providing relief from the
symptoms and stress of a chronic medical, physical, or developmental condition or life-
threatening illness. The goal of Palliative Care services is to improve quality of life for
both the child/youth and the family. Palliative Care is provided by a specially trained
team of doctors, nurses, social workers, and other specialists who work together with a
child/youth’s doctors to provide an extra layer of support. It is appropriate at any stage
of a chronic medical, physical, or developmental condition or life-threatening illness and
can be provided along with curative treatment.
Children/youth must meet LOC functional criteria and suffer from the symptoms and
stress of a chronic medical, physical, or developmental condition or life-threatening
illness.
The HHCM or C-YES will assist the family with obtaining a doctor’s written order
including justification for Expressive Therapy from a Physician, Physician Assistant,
Nurse Practitioner, Occupational Therapist, Physical Therapist or Psychiatrist. This
written order is to be included with the child/youth’s POC and made available to the
MMCP as needed.
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 87
Expressive Therapy (art, music, and play) helps children/youth better understand and
express their reactions through creative and kinesthetic treatment.
Expressive therapy helps children/youth to feel empowered in their own creativity,
control, and aid in their communication of their feelings when their life and body may be
rapidly changing during the stressful time of undergoing a chronic condition and/or life-
threatening illness and the trauma that often comes with its treatment. Whether through
music, art, and/or play therapy, the child/youth may find an outlet that allows them to
express their emotions safely and have a medium where they have complete control to
play and explore with abandon. The family can participate as well, whether in the form
of memories shared together or by tangible objects made by the child/youth they can
hold onto - scrapbooks, paintings, or sculpture - mementos that tell their child/youth’s
life from their perspective and aid in their family’s own journey of grief and loss.
Service Components
Expressive Therapy (art, music and play) helps children/youth better understand and
express their feelings, emotions, behaviors, etc. through creative and kinesthetic
treatment.
Modality
• Expressive Therapy (art, music and play) – 1:1
Setting
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community-based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network, family is broadly
defined, and can include families created through birth, foster care, adoption, or a self -
created unit.
Limitations/Exclusions
Palliative Care Expressive Therapy benefits may not duplicate Hospice or other State
Plan benefits accessible to participants.
Limited to the lesser of four appointments per month or 48 units per calendar year. This
limit can be exceeded when medically necessary.
Certification/Provider Qualifications
Provider Agency Qualifications
Certified Home Health Agency (CHHA), Hospice Organization, Article 28 Clinic, and/or
designated through the NYS Children’s Provider Designation Review Team.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 88
This requires agencies have appropriate license, certification, and/or approval in
accordance with State designation requirements.
• Provider agencies and practitioners adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and
statutes
• Provider agencies adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency ensures that staff receive Mandated Reporting training
prior to service delivery
• The provider agency ensures that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law if
applicable
• The provider agency ensures that any insurance required by the designating
State agency is obtained and maintained
• The provider agency ensures that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Staff Qualifications
• Minimum Qualifications:
o An individual with a minimum of one year working with the medically
fragile population and at least one year of clinical experience with pediatric
population, preferably involving end of life care
o Child Life Specialist with certification through the Child Life Council;
Creative Arts Therapist licensed by the State of New York; Music
Therapist with a Bachelor’s Degree from a program recognized by the
NYS Education Department; Play Therapist with a Master’s Degree from a
program recognized by the New York State Education Department;
current Play Therapist Registration conferred by the Association for Play
Therapy (Expressive Therapy (Art, Music, and Play))
o Direct service workers must have background checks
o Student interns practicing within the scope of the New York State
Education law and supervised by a licensed practitioner in that profession
can deliver HCBS; student interns and limited permittees can treat
Medicaid enrollees under the supervision of a licensed practitioners in that
profession who must be enrolled as a Medicaid provider
Practitioners must operate in agencies which have been designated through the NYS
Children’s Provider Designation Review Team.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 89
Training Requirements
Service Type
Trainings Required
Requirement Completion Timeframe
Palliative
Care
• Mandated Reporter
• Prior to Service Delivery
• Personal Safety/ Safety in
the Community
• Strength Based
Approaches
• Suicide Prevention
• Domestic Violence Signs
and Basic Interventions
• Trauma Informed Care
• Training must be completed within six (6)
months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The table below shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Palliative Care – Expressive Therapy

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 90
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Palliative Care -
Expressive
Therapy
8019
96159
TJ
15 minutes
48/year
PALLIAT IVE CARE – MASSAGE T HERAPY
Definition
Palliative Care is specialized medical care focused on providing relief from the
symptoms and stress of a chronic medical, physical, or developmental condition or life-
threatening illness. The goal of Palliative Care services is to improve quality of life for
both the child/youth and the family. Palliative Care is provided by a specially trained
team of doctors, nurses, social workers, and other specialists who work together with a
child/youth’s doctors to provide an extra layer of support. It is appropriate at any stage
of a chronic medical, physical, or developmental condition or life-threatening illness and
can be provided along with curative treatment.
Children/youth must meet LOC functional criteria and suffer from the symptoms and
stress of a chronic medical, physical, or developmental condition or life-threatening
illness.
The HHCM or C-YES will assist the family with obtaining a doctor’s written order
including justification for Massage Therapy from a Physician, Physician Assistant, Nurse
Practitioner, Occupational Therapist, Physical Therapist or Psychiatrist. The written
order is to be included with the child/youth’s POC and made available to the MMCP as
needed.
Massage Therapy: To improve muscle tone, circulation, range of motion, and address
physical symptoms related to illness as well as provide physical and emotional comfort,
pain management, and restore the idea of healthy touch for children/youth who are
dealing with treatments that may involve painful interventions and ongoing and/or past
trauma.
Service Components
Massage Therapy – To improve muscle tone, circulation, range of motion and address
physical symptoms related to their chronic medical, physical, or developmental
condition or life-threatening illness.
Modality
• Massage Therapy – 1:1

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 91
Setting
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community-based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network, family is broadly
defined, and can include families created through birth, foster care, adoption, or a self -
created unit.
Limitations/Exclusions
Palliative Care Massage Therapy benefits may not duplicate Hospice or other State
Plan benefits accessible to participants.
Limited to no more than 12 appointments per calendar year. This limit can be exceeded
when medically necessary.
Certification/Provider Qualifications
Provider Agency Qualifications
Certified Home Health Agency (CHHA), Hospice Organization, Article 28 Clinic, and/or
designated through the NYS Children’s Provider Designation Review Team.
This requires agencies to have appropriate license, certification, and/or approval in
accordance with State designation requirements.
• Provider agencies and practitioners adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and
statutes
• Provider agencies adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency ensures that staff receive Mandated Reporting training
prior to service delivery
• The provider agency ensures that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law if
applicable
• The provider agency ensures that any insurance required by the designating
State agency is obtained and maintained
• The provider agency ensures that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 92
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Staff Qualifications
• Minimum Qualifications:
o Massage therapist currently licensed by the State of New York
o An individual with a minimum of three years working with the medically
fragile population and at least one year of clinical experience with pediatric
population, preferably involving end of life care
Practitioners must operate in agencies which have been designated through the NYS
Children’s Provider Designation Review Team.
Training Requirements
Service Type
Trainings Required
Requirement Completion Timeframe
Palliative
Care
• Mandated Reporter
• Prior to Service Delivery
• Personal Safety/ Safety in
the Community
• Strength Based
Approaches
• Suicide Prevention
• Domestic Violence Signs
and Basic Interventions
• Trauma Informed Care
Training must be completed within six (6)
months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The table below shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 93
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers must maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Palliative Care – Massage Therapy
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Palliative Care -
Massage Therapy
8018
97124
TJ
15 minutes
72 units/year
Palliative Care – Counseling and Support Services
Definition
Palliative Care is specialized medical care focused on providing relief from the
symptoms and stress of a chronic medical, physical, or developmental condition or life-
threatening illness. The goal of Palliative Care services is to improve quality of life for
both the child/youth and the family. Palliative Care is provided by a specially trained
team of doctors, nurses, social workers, and other specialists who work together with a
child/youth’s doctors to provide an extra layer of support. It is appropriate at any stage
of a chronic medical, physical, or developmental condition or life-threatening illness and
can be provided along with curative treatment.
Children/youth must meet LOC functional criteria and suffer from the symptoms and
stress of a chronic medical, physical, or developmental condition or life-threatening
illness.
Palliative Care Counseling and Support Services can be delivered:
1. To the participant with a chronic medical, physical, or developmental condition or
life-threatening illness and the participant’s identified family members prior to the
passing of the participant,
AND/OR

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 94
2. To the participant’s identified family after the passing of participant, if the HCBS
provider’s Service Plan and the care manager’s plan of care (POC) denotes the
service as outlined below.
The HHCM or C-YES will assist the family with obtaining a doctor’s written order
including justification for Counseling and Support Services from a Physician, Physician
Assistant, Nurse Practitioner, Occupational Therapist, Physical Therapist or
Psychiatrist. The written order is to be included with the child/youth’s POC and made
available to the MMCP as needed.
The Palliative Care Counseling and Support Services provider must conduct an initial
review to determine the needs of the participant and their family. This review should be
incorporated into the provider’s Service Plan that outlines the frequency, scope, and
duration of counseling to be provided and that service plan should be incorporated into
the HCBS care management POC. For families to receive six (6) months of Counseling
and Support Services after the passing of their child/youth the service must be included
in the POC prior to the participant’s passing. The family can also receive one (1)
additional month of Health Home care management, and these needs should be
incorporated in the POC.
Counseling and Support Services: Provide help for participants and their families to
cope with grief related to the participant’s chronic medical, physical, or developmental
condition or life-threatening illness. Children/youth with a chronic medical, physical, or
developmental condition or life-threatening illness and their families cope with grief and
loss in a variety of ways and may need various kinds of support over time, including
counseling, support groups, and other services. Counseling and Support Services can
be provided to participants who are receiving services with a hospice care provider, if
the services are not duplicative.
Further information regarding Counseling and Support Services, including the additional
month of care management and post-mortem counseling and support can be found in
the Palliative Care – Bereavement Services and Health Home Care Management
policy.
Note: These services can be offered at any point after a Children’s Waiver participant is
diagnosed with a chronic medical, physical, or developmental condition or life-
threatening illness.
Service Components

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 95
Counseling and Support Services – Help for participants and their families to cope
with the participant’s chronic medical, physical, or developmental condition or life-
threatening illness and with grief / loss related to the participant’s passing.
Modality
Counseling and Support Services 1:1; family eligible to participate
Setting
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community-based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network, family is broadly
defined, and can include families created through birth, foster care, adoption, or a self -
created unit.
Limitations/Exclusions
Palliative Care Counseling and Support Services benefits may not duplicate Hospice or
other State Plan benefits accessible to participants.
Limited to the lesser of five appointments per month or 60 hours per calendar year.
Certification/Provider Qualifications
Provider Agency Qualifications
CHHA, Hospice Organization, Article 28 Clinic, and/or designated through the NYS
Children’s Provider Designation Review Team. This requires that agencies have
appropriate license, certification, and/or approval in accordance with State designation
requirements.
• Provider agencies and practitioners adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and
statutes
• Provider agencies adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency ensures that staff receive Mandated Reporting prior to
service delivery
• The provider agency ensures that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law if
applicable

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 96
• The provider agency ensures that any insurance required by the designating
State agency is obtained and maintained
• The provider agency ensures that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Staff Qualifications
• Minimum Qualifications:
o An individual with a minimum of three years working with the medically
fragile population and at least one year of clinical experience with pediatric
population, preferably involving end of life care
o Licensed Clinical Social Worker (LCSW), Licensed Master Social Worker
(LMSW), Licensed Psychologist, Licensed Mental Health Counselor
(LMHC), or Licensed Creative Arts Therapist (LCAT) that meet current
NYS licensing guidelines
o Student interns practicing within the scope of the New York State
Education law and supervised by a licensed practitioner in that profession
can deliver HCBS; student interns and limited permittees can treat
Medicaid enrollees under the supervision of a licensed practitioners in that
profession who must be enrolled as a Medicaid provider
Practitioners must operate in agencies which have been designated through the NYS
Children’s Provider Designation Review Team.
Training Requirements
Service Type
Trainings Required
Requirement Completion Timeframe
Palliative
Care
• Mandated Reporter
• Prior to Service Delivery
• Personal Safety/ Safety in
the Community
• Strength Based
Approaches
• Suicide Prevention
• Domestic Violence Signs
and Basic Interventions
• Trauma Informed Care
• Training must be completed within six (6)
months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 97
The tables below shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Note: “Palliative Care - Counseling and Support Services” in the first table are provided
by HCBS providers, and “Palliative Care – Bereavement Counseling Services” are
provided by Health Homes, as outlined in the Palliative Care – Bereavement Services
and Health Home Care Management policy.
Palliative Care – Counseling and Support Services
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Palliative Care –
Counseling and
Support Services
8017
90832
TJ
30 minutes
Limited to the
lesser of 10
units per
month or 120
units per
calendar year
Palliative Care - Bereavement Counseling Services
Service
Rate
Code
Procedure
Code
Modifier
Unit Measure
Unit Limit

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 98
Upstate Codes
Bereavement Services -
HH Low Acuity
7946
96156
Per
assessment
1
unit/calendar
year
Bereavement Services
HH Medium Acuity
7947
96156
Per
assessment
1
unit/calendar
year
Bereavement Services -
HH High Acuity
7948
96156
Per
assessment
1
unit/calendar
year
Downstate Codes
Bereavement Services -
HH Low Acuity
7949
96156
Per
assessment
1
unit/calendar
year
Bereavement Services -
HH Low Acuity
7950
96156
Per
assessment
1
unit/calendar
year
Bereavement Services -
HH Low Acuity
7951
96156
Per
assessment
1
unit/calendar
year
Bereavement Assessment/Counseling
Bereavement -
Assessment/Counseling
7952
96156
Bereavement
Risk
Assessment
and up to six
(6) months of
Bereavement
counseling
1 unit/
calendar
year per
member
Palliative Care – Pain and Symptom Management
Definition
Palliative Care is specialized medical care focused on providing relief from the
symptoms and stress of a chronic medical, physical, or developmental condition or life-
threatening illness. The goal of Palliative Care services is to improve quality of life for
both the child/youth and the family. Palliative Care is provided by a specially trained
team of doctors, nurses, social workers, and other specialists who work together with a
child/youth’s doctors to provide an extra layer of support. It is appropriate at any stage
of a chronic medical, physical, or developmental condition and can be provided along
with curative treatment.
Children/youth must meet LOC functional criteria and suffer from the symptoms and
stress of chronic medical, physical, or developmental conditions.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 99
The HHCM or C-YES will assist the family with obtaining a written order including
justification for Pain and Symptom Management from a Physician. The written order is
to be included with the child/youth’s POC and made available to the MMCP as needed.
Pain and Symptom Management: Relief and/or control of the child/youth’s suffering
related to their chronic medical, physical, or developmental condition.
Pain and Symptom Management is an important part of aiding in providing relief from
pain and symptoms and/or controlling pain, symptoms, and side effects related to
chronic medical, physical, or developmental conditions or life-threatening illness a
child/youth is enduring. This management is not only an important part of humanely
caring for the child/youth’s pain and suffering but helping the child/youth and family
cope and preserve their quality of life at a difficult time.
Service Components
Pain and Symptom Management – Relief and/or control of the child/youth’s suffering
related to their chronic medical, physical, or developmental condition.
Modality
• Pain and Symptom Management – 1:1
Setting
Allowable settings in compliance with Medicaid regulations and the Home and
Community Based Settings Final Rule (§441.301(c)(4) and §441.710) (see Appendix B)
will exhibit characteristics and qualities most often articulated by the individual
child/youth and family/caregiver as key determinants of independence and community
integration. Services should be offered in the setting least restrictive for desired
outcomes, including the most integrated home or other community-based settings
where the beneficiary lives, works, engages in services, and/or socializes. While
remaining inclusive of those in the family and caregiver network, family is broadly
defined, and can include families created through birth, foster care, adoption, or a self -
created unit.
Limitations/Exclusions
Palliative Care Pain and Symptom Management benefits may not duplicate Hospice or
other State Plan benefits accessible to participants.
Certification/Provider Qualifications
Provider Agency Qualifications
Certified Home Health Agency (CHHA), Hospice Organization, or Article 28 Clinic and
designated through the NYS Children’s Provider Designation Review Team.
Practitioners must operate in agencies which have been designated through the NYS
Children’s Provider Designation Review Team. This requires agencies have appropriate

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 100
license, certification, and/or approval in accordance with State designation
requirements.
• Provider agencies and practitioners adhere to all Medicaid requirements in
this Manual and in other applicable provider manuals, regulations, and
statutes
• Provider agencies adhere to cultural competency guidelines
• Provider agencies must be knowledgeable and have experience in trauma-
informed care and working with individuals from the cultural groups of those
being served
• The provider agency ensures that staff receive Mandated Reporting training
prior to service delivery
• The provider agency ensures that practitioners maintain the licensure
necessary to provide services under their scope of practice under State law if
applicable
• The provider agency ensures that any insurance required by the designating
State agency is obtained and maintained
• The provider agency ensures that any safety precautions needed to protect
the child population served are taken as necessary and required by the
designating State agency
Additional information and application for Children’s HCBS can be found on the DOH
website.
Individual Staff Qualifications
• Minimum Qualifications:
o An individual with a minimum of three years working with the medically
fragile population and at least one year of clinical experience with pediatric
population, preferably involving end of life care
o Pediatrician or Family Medicine Physician board certified in Pediatrics or
Family Medicine licensed by the State of New York; Nurse Practitioner
licensed by the State of New York (Pain and Symptom Management); or
Registered Nurse licensed by the State of New York under the direct
supervision of a pediatrician or medical physician, board certified in
Pediatrics.
Practitioners must operate in agencies which have been designated through the NYS
Children’s Provider Designation Review Team.
Training Requirements
Service Type
Trainings Required
Requirement Completion Timeframe
Palliative
Care
• Mandated Reporter
• Prior to Service Delivery

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 101
Service Type
Trainings Required
Requirement Completion Timeframe
• Personal Safety/ Safety in
the Community
• Strength Based
Approaches
• Suicide Prevention
• Domestic Violence Signs
and Basic Interventions
• Trauma Informed Care
• Training must be completed within six (6)
months of hire date.
Additional information regarding training requirements can be found in Appendix E.
Service Billing Details
Rate Code Description
The below table shows the show the rate code, CPT code, and modifier code
combinations that will be required under Medicaid Managed Care. Providers will use
these coding combinations to indicate to the MMCP that the claim is for a
children/youth’s service and is to be paid at the government rate. The procedure and
modifier code combinations must be adhered to by both provider and MMCP to ensure
appropriate rate payment.
In acknowledgement of the need for checks against fraud and abuse, but to ensure a
child/youth’s access to services, service utilization in excess of the "soft" unit (i.e.,
annual, daily, dollar amount) limits must be based on medical necessity. Documentation
of the medical necessity for extended durations must be kept on file in the child/youth’s
record. HCBS should be initially authorized for no more than six months at a time and
based on each participant’s unique needs. To exceed billing limits for children/youth
enrolled in managed care, providers must contact the MMCP to receive guidance
regarding the Plan’s specific documentation requirements in these instances ; for
children/youth enrolled in FFS, HCBS providers muat maintain documentation from a
licensed professional that outlines the need to exceed the service limit (e.g., copy of an
assessment from a licensed professional; letter from a licensed professional that clearly
describes the need for additional units of service, etc.).
In addition to requiring concurrent utilization review and authorization, the MMCP may
conduct post-payment administrative reviews to ensure services were provided
appropriately.
Palliative Care – Pain and Symptom Management
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Palliative Care -
Pain and
Symptom
Management
8016
99347
TJ
15 minutes
No limit, as
required by
child/youth’s

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 102
physician
order
Adaptive and Assistive T echnology
Definition
Adaptive and Assistive Technology (AT) provides technological aids and devices
identified within the child/youth’s POC which enable the accomplishment of daily living
tasks that are necessary to support the health, welfare, and safety of the child/youth.
Service Components
Adaptive and Assistive Technology includes but is not limited to:
• Positioning devices
• Mobility devices
• Augmentative Communication devices
• Computer Accessibility devices
• Assistive Demotics/Home Automation devices
• Standing boards/frames and therapeutic equipment for the purpose of
maintaining or improving the participant's strength, mobility, or flexibility to
perform activities of daily living
• Adaptive switches/devices
• Meal preparation and eating aids/devices/appliances
• Specially adapted locks
• Motorized wheelchairs
• Guide dogs, hearing dogs, service dogs (as defined in New York Civil Rights Law
Article 47-b(4)) (for additional guidance regarding service dogs, please refer to
Appendix F)
• Electronic, wireless, solar-powered, or other energy powered devices that
demonstrate to the satisfaction of the commissioner, or designee, that the
device(s) will significantly enable the participant to live, work, or meaningfully
participate in the community with less reliance on paid staff supervision or
assistance
o Such devices may include computers, observation cameras, sensors,
telecommunication screens, and/or telephones and/or other telecare
support services/systems that enable the participant to interact with
remote staff to ensure health and safety
o Such devices cannot be used for surveillance, but to support the person to
live with greater independence including devices to assist with medication
administration, including tele-care devices that prompt, teach, or otherwise
assist the participant to independently self-administer medication routinely,
portable generators necessary to support equipment, or devices needed
for the health or safety of the person including stretcher stations

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 103
Adaptive and Assistive Technology Services include:
• Evaluation of the adaptive and assistive technology needs of a participant,
including a functional evaluation of the impact of the provision of appropriate
adaptive and assistive technology and appropriate services to the participant in
the customary environment of the participant
• Services consisting of purchasing, leasing, or otherwise providing for the
acquisition of adaptive and assistive technology devices for the participant
• Services consisting of selecting, designing, fitting, customizing, adapting,
applying, maintaining, repairing, or replacing adaptive and assistive technology
devices
• Training or technical assistance for the participant, or, where appropriate, the
family members, guardians, advocates, or authorized representatives of the
participant
• Training or technical assistance for professionals or other individuals who provide
services to, employ, or are otherwise substantially involved in the major life
functions of the participant
Modality
The HHCM/C-YES will coordinate requests for AT with the LDSS in conjunction with
DOH for children/youth enrolled in Fee-for-Service Medicaid. The HHCM/C-YES will
coordinate requests for AT with the Medicaid Managed Care Plan for children/youth
enrolled in a MMCP.
Limitations/Exclusions
The Adaptive and Assistive Technology available through the HCBS authorities cannot
duplicate equipment and/or technology otherwise available through the Medicaid State
Plan under 1905(a) of the Social Security Act or other federal/state funding streams.
Equipment must be beyond the scope of Durable Medical Equipment (DME). DME is a
SPA service and needs to be pursued first, if the need meets the DME requirements.
Care Managers can consult with NYS DOH prior to submitting the request for DME.
Refer to the DME Manual (under ‘Fee Schedule’) for further information.
Adaptive and assistive devices are expected to be a one-time only purchase.
Replacements, repairs, upgrades, and/or enhancements made to existing equipment
will be paid if documented as a necessity and approved by the State or its designee.
Ongoing monitoring associated with telecare support services or other approved
systems authorized under this definition may be provided, if necessary, for health and
safety and documented to the satisfaction of the State or designee. The HHCM, C-YES,
or MMCP will ensure, that where appropriate, justification from physicians or other
specialists or clinicians has been obtained.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 104
Warranties, repairs, and/or maintenance on adaptive and assistive technology only
when most cost effective and efficient means to meet the need and are not available
through the Medicaid State Plan 1905(a) or third-party resources.
Cost Limits
All Adaptive and Assistive Technology costs require prior approval from the LDSS in
conjunction with DOH or the MMCP. Adaptive and Assistive Technology is subject to a
$15,000 per calendar year soft cap. The State or its designee may consider exceptions
when medically necessary, including but not limited to a significant change in the child’s
needs or capabilities.
Certification/ Provider Qualifications
For Adaptive and Assistive Technology, the LDSS (for FFS enrollees) or MMCP (for
managed care enrollees) is the provider of record for billing purposes using the
standard bidding process.
The HHCM/C-YES will assist in determining the need for the service, identifying the
expected benefit to the child/youth, obtaining a physician’s order, obtaining the clinical
justification and/or scope of the work, securing bids, and facilitating the completion of
the Final Cost Form.
The LDSS or MMCP secures a vendor qualified to complete the required work.
For FFS enrollees, standard provisions of the NYS Finance Law and procurement
policies must be followed to ensure that vendors are qualified, and that State-required
bidding procedures have been followed. MMCPs are not required to obtain bids for
Adaptive and Assistive Technology projects. Final payment to vendors is provided once
project is verified as complete and in compliance with approved project scope.
LDSS or MMCP staff verify the qualifications of the Adaptive and Assistive Technology
vendor:
• Must be familiar with the Adaptive and Assistive Technology policies permitted in
the waiver program as described in this Manual; the LDSS or MMCP should
supply the evaluator with a copy of both prior to initiation of the evaluation
• Must be able to communicate well with all parties involved with the purchase of
the equipment and any training needed (e.g., consumers, contractors, and local
government officials)
• Must be able to clearly describe in writing, and by design, the proposed purchase
• Must have knowledge of assistive technology and specific adaptive equipment
appropriate for the child/youth’s needs
LDSS, in conjunction with DOH or the MMCP will determine the most cost-effective
service that will meet the child/youth’s needs.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 105
For further information regarding assessing need, service authorization, service
delivery, and payment, including process flows refer to the following Adaptive and
Assistive Technology Resources and Forms:
Service Billing Details
FFS Billing
Some providers of AT will require partial payment to purchase materials, technology,
and/or equipment. In addition, the evaluator/assessor invoice may have to be paid prior
to completion of the modification/adaptation request. To address these potential
barriers, the NYS DOH has established a Special Project Voucher (SPV) Fund and a
process that will eliminate the need for the LDSS to front funds to non-Medicaid enrolled
providers in advance of receiving Medicaid reimbursement for LDSS-authorized
services.
When the LDSS requires upfront funds for an AT service, the LDSS must submit the
Pre-project Evaluation Payment Request Form and/or the Description and Cost
Projection Form, as appropriate, with all supporting documents to the NYS DOH. NYS
DOH’s Children’s Waiver staff will process the request for SPV funds, including
requesting that a check be issued to the County Treasurer at the LDSS. Please note,
the check will be issued from the Office of Temporary and Disability Assistance (OTDA).
If the request is not approved, the LDSS will be so notified. If additional information is
needed, the disbursement may be delayed pending submission of the additional
information.
MMCP Billing
Adaptive and Assistive Technology will be billed using 837P by the Plan when
submitting the encounter to DOH.
The table below shows the rate code, CPT code, and modifier code combination that
will be required under Medicaid Managed Care. The procedure and modifier code
combinations must be adhered to by the MMCP to ensure appropriate rate payment.
Adaptive and Assistive Technology
• Parent Info Sheet- Adaptive and Assistive Technology
• Guidelines for Authorizing Adaptive and Assistive Technology
• Pre-project Evaluation Payment Request Form
• Description and Cost Projection Form
• Notice of Decision to Authorize or Deny Adaptive and Assistive
Technology
• Final Cost Form

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 106
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Adaptive and
Assistive
Technology
8037
T2028
HA
$1.00
$15,000 per
calendar year
Adaptive and
Assistive
Technology
8038
T2028
HA, V1
$10.00
$15,000 per
calendar year
Adaptive and
Assistive
Technology
8039
T2028
HA, V2
$100.00
$15,000 per
calendar year
Adaptive and
Assistive
Technology
8040
T2028
HA, V3
$1,000.00
$15,000 per
calendar year
Vehicle Modifications
Definition
Vehicle Modifications (VMods) provide physical adaptations to the primary vehicle of the
enrolled child/youth which, per the child/youth’s POC, are identified as necessary to
support the health, welfare, and safety of the child/youth or that enable the child/youth
to function with greater independence.
Service Components
Modifications include but are not limited to:
• Portable electric/hydraulic and manual lift
• Ramps
• Foot controls
• Wheelchair lock downs/wheelchair floor
• Deep dish steering wheel
• Spinner knobs
• Hand controls
• Parking brake extension
• Replacement of roof with fiberglass top
• Floor cut outs
• Extension of steering wheel column
• Raised door
• Repositioning of seats
• Dashboard adaptations
• Other ancillary equipment or modifications necessary to guarantee full access to,
and safety in, a motor vehicle
The LDSS (for FFS enrollees) or MMCP (for managed care enrollees) secures a
contractor and/or evaluator qualified to complete the required work. In the case of

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 107
Vehicle Modifications, the evaluators and modifiers are approved by the National
Mobility Equipment Dealers Association (NMEDA). Activities include but are not limited
to; determining the need for the service, the safety of the proposed modification, its
expected benefit to the child/youth, and the most cost-effective approach to fulfill the
child/youth’s need.
In FFS, the work is done by a contractor who is selected by the LDSS in conjunction
with DOH through a standard bid process, following the rules established by the Office
of the State Comptroller. Standard provisions of the NYS Finance Law and procurement
policies must be followed to ensure that contractors are qualified and that State-required
bidding procedures have been followed. Final payment to vendors is provided once
project is verified as complete and in compliance with approved project scope.
In managed care, the Plan is the payer and may contract with an approved network
provider for the service. MMCPs are not required to obtain bids for vehicle modification
projects. Services are only billed to the MMCP once the contract work is verified as
complete and the amount billed is equal to the contract value of the approved scope.
Note: This service does not duplicate other services available through the New York
Medicaid State Plan. All services require prior authorization by the MMCP or the LDSS
in conjunction with DOH.
Modality
The HHCM/C-YES will coordinate requests for VMods with the LDSS in conjunction with
DOH for children/youth enrolled in Fee-for-Service Medicaid. The HHCM/C-YES will
coordinate requests for VMods with the Medicaid Managed Care Plan for
children/youth enrolled in a MMCP.
Limitations/Exclusions
Other exclusions include the purchase, installation, and/or maintenance of items such
as cellular phones, global positioning/tracking devices, or other mobile communication
devices; repair or replacement of modified equipment damaged or destroyed in an
accident; alarm systems; auto loan payments; insurance coverage; costs related to
obtaining a driver’s license, title/registration, license plates, emergency road service, or
rental vehicles when a vehicle modification is in process.
Repair & Replacement of Modification
In most instances a specific type of Vehicle Modification is a one-time benefit to motor
vehicles used by the child/youth. However, in reasonable circumstances determined
and approved by the State, a second modification may be considered for funding if the
current modifications are in need of repair, worn-out, or unsafe. Replacements, repairs,
upgrades, or enhancements made to existing equipment will be paid if documented as a
necessity. In addition, when the modification must be replaced or repaired, a
depreciation schedule will be used to determine the limit of the amount to be applied to
the cost.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 108
Vehicle Modifications are limited to the primary means of transportation for the
child/youth. The vehicle may be owned by the child/youth or by a family member or non-
relative who provides primary, consistent, and ongoing transportation for the child/youth.
All equipment and technology used for entertainment is prohibited.
Modification Limits
Only those services not reimbursable under the Medicaid State Plan under 1905(a) of
the Social Security Act, or other federal/state funding streams will be reimbursable
under the HCBS Waiver.
Contracts for Vehicle Modifications may not exceed $25,000 per calendar year without
prior approval from DOH or the MMCP. The State may consider exceptions when
medically necessary, including but not limited to a significant change in the child’s
needs or capabilities.
Certification/Provider Qualifications
Modification Contractor/Craftsman with licensure appropriate to the trade.
LDSS or MMCP staff verify the qualifications of vehicle modification providers who must
present the following knowledge and skills:
• Must be familiar with the Vehicle Modification policies permitted in the waiver
program as described in State guidance; the LDSS/HRA/MMCP should supply
the evaluator with a copy of both prior to initiation of the evaluation
• Must be able to communicate well with all parties involved with the development
of Vehicle Modifications (e.g., consumers, contractors, and local government
officials)
• Must be able to clearly describe in writing, and by design, the proposed vehicle
modification
• Must know and be able to apply the New York State Building Code, Current
Accessibility Standards, and the Federal Accessibility Guidelines found in the
Fair Housing Amendment Act (as relevant to any vehicle modification)
• Must have knowledge of assistive technology and specific adaptive equipment
appropriate for the child/youth’s needs
• Must have skill in design/drafting in order to clearly describe the proposed
modification
• Must be able to complete all components of an On-Site Evaluation
Contractors performing any adaptation for a child/youth in the waiver program is
required to:
• Be bonded
• Maintain adequate and appropriate licensure
• Maintain vehicle modification provider certification from NMEDA

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 109
Provider qualifications are verified at the beginning of the Vehicle Modification project by
the LDSS/MMCP.
Vehicle Modification Resources and Forms:
Service Billing Details
FFS Billing
Most providers of VMods will require partial payment to purchase materials,
technology, and/or equipment. In addition, the evaluator/assessor invoice may have to
be paid prior to completion of the modification. To address these potential barriers, the
NYS DOH has established a Special Project Voucher (SPV) Fund and a process that
will eliminate the need for the LDSS to front funds to non-Medicaid enrolled providers in
advance of receiving Medicaid reimbursement for LDSS-authorized services.
When the LDSS requires upfront funds for a VMod service, the LDSS must submit the
Pre-project Evaluation Payment Request Form and/or the Description and Cost
Projection Form, as appropriate, with all supporting documents to the NYS DOH. NYS
DOH’s Children’s Waiver staff will process the request for SPV funds, including
requesting that a check be issued to the County Treasurer at the LDSS. Please note,
the check will be issued from the Office of Temporary and Disability Assistance (OTDA).
If the request is not approved, the LDSS will be so notified. If additional information is
needed, the disbursement may be delayed pending submission of the additional
information.
MMCP Billing
Plans will use 837I encounter format when billing DOH for VMod services.
The table below shows the rate code, CPT code, and modifier code combinations that
will be required under Medicaid Managed Care. The procedure and modifier code
combinations must be adhered to by the MMCP to ensure appropriate rate payment.
Vehicle Modifications
• Parent Info Sheet- Vehicle Modifications
• Guidelines for Authorizing Vehicle Modifications
• Pre-project Evaluation Payment Request Form
• Description and Cost Projection Form
• Notice of Decision to Authorize or Deny Vehicle Modifications
• Final Cost Form

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 110
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Vehicle
Modifications
8041
T2039
HA
$1.00
$25,000 per
calendar year
Vehicle
Modifications
8042
T2039
HA, V1
$10.00
$25,000 per
calendar year
Vehicle
Modifications
8043
T2039
HA, V2
$100.00
$25,000 per
calendar year
Vehicle
Modifications
8044
T2039
HA, V3
$1,000.00
$25,000 per
calendar year
Environmental Modifications
Definition
Environmental Modifications (EMods) provide internal and external physical adaptations
to the primary residence of the enrolled child/youth which, per the child/youth’s POC,
are identified as necessary to support the health, welfare, and safety of the child/youth
or that enable the child/youth to function with greater independence in the home and
without which the child/youth would require and institutional and/or more restrictive
living setting.
Service Components
Modifications include but are not limited to:
• Installation of ramps, handrails, and grab-bars
• Widening of doorways (but not hallways)
• Modifications of bathroom facilities
• Installation of specialized electric and plumbing systems that are necessary to
accommodate the medical equipment and supplies needed for the welfare of the
recipient
• Lifts and related equipment
• Elevators when no feasible alternative is available
• Automatic or manual door openers/bells
• Modifications of the kitchen necessary for the participant to function more
independently in his/her home
• Medically necessary air conditioning
• Braille identification systems
• Tactile orientation systems
• Bed shaker alarm devices
• Strobe light smoke detection and alarm devices
• Small area driveway paving for wheel-chair entrance/egress from van to home
Safe environment modifications for behaviorally challenged participants require the prior
review of a behavioral specialist and include window protections, reinforcement of walls,

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 111
durable wall finishes, open-door signal devices, fencing, video monitoring systems, and
shatter-proof shower doors. These may also include future technology devices that
allow the participant to live more safely and independently to avoid possible institutional
placement or placement in a more restrictive living environment, which are available at
a reasonable cost in comparison to living in a more restrictive residential setting.
The scope of Environmental Modifications will also include necessary assessments to
determine the types of modifications needed.
Note: This service does not duplicate other services available through the New York
Medicaid State Plan. All services require prior authorization by the LDSS in conjunction
with DOH if exceeding established limits or MMCP.
Modality
The HHCM/C-YES will coordinate requests for EMods with the LDSS in conjunction with
DOH for children/youth enrolled in Fee-for-Service Medicaid. The HHCM/C-YES will
coordinate requests for EMods with the Medicaid Managed Care Plan for children/youth
enrolled in a MMCP.
Limitations/Exclusions
Excluded are those adaptations or improvements to the home that are of general utility
and are not of direct medical or remedial benefit to the child/youth. Adaptations that add
to the total square footage of the home's footprint are excluded from this benefit except
when necessary to complete an adaptation (e.g. in order to improve entrance/egress to
a residence or to configure a bathroom to accommodate a wheelchair). Also excluded
are pools and hot tubs and associated modifications for entering or exiting the pool or
hot tub.
Repair & Replacement of Modification
In most instances, a specific type of Environmental Modification is a one-time benefit.
However, in reasonable circumstances determined and approved by the State, a
second modification may be considered for funding as follows: if a person moves to
another home; if the current modifications are in need of repair, worn-out, or unsafe; or
if a participant wishes to spend considerable time with a non-cohabitating parent in their
home and such modifications are required to ensure health and safety during these
periods.
State policy places certain limitations on environmental modifications requested when
the home/apartment is a leased space, including property owner sign-off on the
modification and limitations on federal/state liability for the cost of
removal/replacement/repair of items in public spaces of rental properties.
Modification Limits

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 112
Only those services not reimbursable under the Medicaid State Plan under 1905(a) of
the Social Security Act, or other federal/state funding streams will be reimbursable
under the HCBS Waiver.
All Environmental Modifications require prior approval from the LDSS in conjunction with
DOH or the MMCP. For Environmental Modifications, the LDSS or MMCP is the
provider of record for billing purposes. Environmental Modifications have a $25,000 per
calendar year soft cap. The State may consider exceptions when medically necessary,
including but not limited to a significant change in the child/youth’s needs or capabilities.
Note: This service does not duplicate other services available through the New York
Medicaid State Plan. All services require prior authorization by the LDSS in conjunction
with DOH if exceeding established limits or MMCP.
Certification/Provider Qualifications
Environmental Modification Contractor/Craftsman with licensure appropriate to trade.
LDSS or MMCP staff verify the qualifications of home modification providers present the
following knowledge and skills:
• Must be familiar with the home adaptation policies permitted in the waiver
program as described in state guidance; the LDSS/HRA/MMCP should supply
the evaluator with a copy of both prior to initiation of the evaluation
• Must be able to communicate well with all parties involved with the development
of home adaptations (e.g., consumers, contractors, and local government
officials)
• Must be able to clearly describe in writing, and by design, the proposed home
adaptation
• Must know and be able to apply the New York State Building Code, Current
Accessibility Standards, and the Federal Accessibility Guidelines found in the
Fair Housing Amendment Act (as applicable to the home modification)
• Must have knowledge of assistive technology and specific adaptive equipment
appropriate for the child/youth’s needs
• Must have skill in design/drafting in order to clearly describe the proposed
modification
• Must be able to complete all components of an on-site evaluation
Contractors performing any adaptation for a child/youth in the waiver program are
required to:
• Be bonded
• Maintain adequate and appropriate licensure
• Obtain any and all permits required by state and local municipality codes for the
modification
• Agree that before final payment is made the contractor must show that the local
municipal branch of government that issued the initial permit has inspected the
work

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 113
Provider qualifications are verified at the beginning of the Environmental Modification
contract by the LDSS/MMCP.
Environmental Modification Resources and Forms:
Service Billing Details
FFS Billing
Most providers of EModswill require partial payment to purchase materials, technology,
and/or equipment. In addition, the evaluator/assessor invoice may have to be paid prior
to completion of the modification. To address these potential barriers, the NYS DOH
has established a Special Project Voucher (SPV) Fund and a process that will eliminate
the need for the LDSS to front funds to non-Medicaid enrolled providers in advance of
receiving Medicaid reimbursement for LDSS-authorized services.
When the LDSS requires upfront funds for an EMod service, the LDSS must submit the
Pre-project Evaluation Payment Request Form and/or the Description and Cost
Projection Form with all supporting documents to the NYS DOH. NYS DOH’s Children’s
Waiver staff will process the request for SPV funds, including requesting that a check be
issued to the County Treasurer at the LDSS. Please note, the check will be issued from
the Office of Temporary and Disability Assistance (OTDA). If the request is not
approved, the LDSS will be so notified. If additional information is needed, the
disbursement may be delayed pending submission of the additional information.
MMCP Billing
Plans will use 837I encounter format when billing DOH for EMod services.
The table below shows the rate code, CPT code, and modifier code combinations that
will be required under Medicaid Managed Care. The procedure and modifier code
combinations must be adhered to by the MMCP to ensure appropriate rate payment.
Environmental Modifications
• Parent Info Sheet- Environmental Modifications
• Guidelines for Authorizing Environmental Modifications
• Guidance on Environmental Modifications to Support Behaviorally
Health Challenged Members
• Pre-project Evaluation Payment Request Form
• Description and Cost Projection Form
• Notice of Decision to Authorize or Deny Environmental Modifications
• Final Cost Form

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 114
Service
Rate Code
Procedure
Code
Modifier
Unit Measure
Unit Limit
Environmental
Modifications
8032
S5165
HA
$1.00
$25,000 per
calendar year
Environmental
Modifications
8034
S5165
HA, V1
$10.00
$25,000 per
calendar year
Environmental
Modifications
8035
S5165
HA, V2
$100.00
$25,000 per
calendar year
Environmental
Modifications
8036
S5165
HA, V3
$1,000.00
$25,000 per
year calendar
Non-Medical T ransportation
Definition
Non-Medical Transportation services are offered, in addition to any medical
transportation furnished under the 42 CFR 440.17(a) in the State Plan. Non-Medical
Transportation services are available for individuals to access authorized HCBS and
destinations that are related to a goal included on the child/youth’s POC.
Service Components
Examples where this service may be requested include transportation to: HCBS that a
child/youth was determined eligible to receive, a job interview, college fair, a wellness
seminar, a GED preparatory class, etc. This service will be provided to meet the
child/youth’s needs as determined by an assessment performed in accordance with the
State’s requirements and as outlined in the child/youth’s POC.
The care manager must document a need for transportation to support an individual’s
identified goals. The HHCM will include justification for this service within the Person-
Centered POC. For individuals not enrolled in a HH, the Independent Entity or MMCP
will be responsible for completing documentation of which goals in an individual’s POC
to which the trips will be tied. For each participant utilizing Non-Medical Transportation,
the Transportation Manager will provide a monthly report of authorized trips to the State.
Limitations/Exclusions
Generally, the same rules used to determine reimbursement of trips to medical
appointments should be followed when considering reimbursement of non-medical trips
for eligible participants. Only those services not reimbursable under the CFCO State
Medicaid Plan will be reimbursable under the HCBS Waiver.
The following guidelines apply to Non-Medical Transportation:
• Transportation must be tied to a goal in the POC
• Transportation is available for a specified duration

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 115
• Individuals receiving residential services are ineligible for Non-Medical
Transportation
• Use transportation available free of charge
• Use the medically appropriate mode of transportation
• Travel within the common marketing area
• When possible, trips should be combined
• Justify need for travel outside the common marketing area
Vouchers submitted for personal vehicle mileage reimbursement must be submitted
within 90 days of the date of service. Only when there are extenuating circumstances,
will DOH allow payment for trips that are submitted after the 90-day time period. These
requests will be considered on a case-by-case basis provided valid justification is given.
Reimbursement for travel can be denied when the destination does not support the
participant’s integration into the community.
A participant’s POC outlines the general parameters of the child/youth’s Non-Medical
Transportation needs. However, these needs can change or be amended based upon
the participant’s stated goals and/or successful ongoing integration into the community.
Certification/Provider Qualifications
Agencies interested in providing Non-Medical Transportation must be enrolled in the
FFS program as a current Medicaid Transportation Provider.
Please see the following links on information on Medicaid Transportation:
• Transportation Provider Manuals
• Transportation Provider Enrollment Application
Roles Related to a Participant’s Access to Non-Medical Transportation
The following roles and guidelines serve to inform the HHCM, MMCP, and the
Transportation Manager of the procedures and rules surrounding an eligible
participant’s access to the Non-Medical Transportation benefit.
HHCM Roles
HHCMs are responsible for conducting and developing the Person-Centered POC. If
the care manager determines there is a need for transportation to support an
individual’s identified goals, the HHCM will include justification for this service within the
Person-Centered POC. The HHCMs will complete the DOH POC Grid for Non-Medical
Transportation for Children’s HCBS (Grid) with all known information. It is possible that
the complete trip destination details may not be known (e.g. exact appointment time and
date). This information can be provided by the enrollee to the Transportation Manager
upon request of transportation.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 116
The CMA should at a minimum list the goal from the POC; specific activity, support, or
task; provider of services (if applicable); start and end date. After completing the POC
and the Grid, the HHCM will send it to the MMCP. If the child/youth is not yet enrolled in
a plan, the HHCM will send the Grid directly to Department of Health’s Medicaid
Transportation Manager for review.
Medicaid Managed Care Plan Roles
The MMCP is responsible for approving the Person-Centered POC and for forwarding
the completed Grid to DOH’s Medicaid Transportation Manager.
For individuals not enrolled in a HH, the MMCP will be responsible for completing the
Grid based on the individual’s POC and forwarding to the Transportation Manager. The
Grid will include documentation for Non-Medical Transportation including documentation
of which goals in an individual’s POC the trips will be tied to.
The DOH POC Grid for Non-Medical Transportation for Children’s HCBS is
completed by the MMCP based on the participant’s POC and includes the following
information:
• Participant information
• HCBS provider information
• Non-Medical Transportation service requested
• Supporting information includes:
o Goal from the POC
o HCBS or specific activity/support/task
o Mode of transportation service needed
o Trip destination/location
o Start date/end date
o Frequency
The MMCP will forward the completed Grid to the Transportation Manager any time
there are changes to the Grid.
Transportation Manager Roles
The Transportation Manager is responsible for authorizing transportation services in
accordance with Medicaid policy, by approved Medicaid Transportation providers, and
as supported on the MMCP-provided Grid. Once the Grid is received from the MMCP,
the Transportation Manager should assume that the MMCP has reviewed and approved
the Non-Medical Transportation included in the individual’s POC and that trips included
in the Grid are appropriate. The Transportation Manager is responsible for ensuring
adherence to the guidelines below for Non-Medical Transportation, which include
assigning the most medically appropriate, cost-effective mode of transportation.
Enrollees have freedom of choice regarding the transportation provider within the
assigned mode (e.g. ambulette, taxi, public transportation, etc.).
Contact Information for Transportation Managers

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 117
NYC & Upstate: Medical Answering Services (MAS)
• Website
• Forms & Resources for Enrollees
• Physician Attestation for Mileage Reimbursement Individual Appointments
Fax number for submitting all forms: (315) 299-2786
Secure email: Harp-info@medanswering.com
(When sending completed Grids: “Attn: Non-Medical Transportation for
Children’s Home and Community Based Services (HCBS)”)
Long Island: LogistiCare Solutions, LLC
• Website
• Medicaid Transformation Information on Website
Fax number for submitting mileage reimbursement forms: (866) 528-0462
(When sending completed Grids: Attn: Non-Medical Transportation for Children’s
Home and Community Based Services (HCBS)”)
Additional Contact Information:
NYS Department of Health Transportation Unit: medtrans@health.ny.gov
NYS Office of Mental Health: omh.sm.co.HCBS-Application@omh.ny.gov
Service Billing Details
Non-Medical Transportation will be paid fee-for-service for eligible children/youth,
regardless of whether the child/youth is enrolled in Medicaid Managed Care. Please
refer to the Medicaid Transportation Guidelines for more details.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 118
APPENDICES
Appendix A: Glossary of Key Terms
Care Team or Multi-disciplinary Team: Are the providers, identified family supports,
family members, managed care plan and other individuals or entities that the child/youth
or family identified to be involved in the care coordination and service provision
development.
Child/Youth: Throughout this document, the term “child/youth” or “children/youth” refers
to a child/youth under age 21.
Children and Youth Evaluation Service (C-YES): C-YES is the State-designated
Independent Entity which conducts HCBS/LOC eligibility determinations and provides
Medicaid application assistance for children who are eligible for HCBS and not yet
enrolled in Medicaid. C-YES also develops an HCBS POC, refers eligible children for
HCBS, and monitors access to care for children who opt out of HH care management.
Collateral Contact: Family members, caregivers, and other stakeholders identified on
the child/youth’s Plan of Care.
Cultural Competency: Defined as attributes of a behavioral healthcare organization
that describe the set of congruent behaviors, attitudes, skills, policies, and procedures
that are promoted and endorsed to enable caregivers at all levels of the organization to
work effectively and efficiently with persons and communities of all cultural
backgrounds. An important element of cultural competence is the capacity to overcome
structural barriers in healthcare delivery that sustain health and healthcare disparities
across cultural groups.
Developmental Disability: Section 1.03(22) of the New York State Mental Hygiene
Law is the legal base for eligibility determination and defines Developmental Disability
as: A disability of a person that: (a)(1) Is attributable to an intellectual disability cerebral
palsy, epilepsy, neurological impairment, familial dysautonomia, Prader-Willi syndrome
or autism; (2) Is attributable to any other condition of a person found to be closely
related to an intellectual disability because such condition results in similar impairment
of general intellectual functioning or adaptive behavior to that of intellectually disabled
persons or requires treatment and services similar to those required for such persons;
or (3) Is attributable to dyslexia resulting from a disability described in (1) or (2); (b)
Originates before such person attains age twenty-two; (c) Has continued or can be
expected to continue indefinitely; and (d) Constitutes a substantial handicap to such
person's ability to function normally in society.
Discharge: Describes when a participant will no longer receive HCBS. In some cases,
a child/youth may be released from specific HCBS that no longer meets the
child/youth’s goals but may remain in receipt of additional HCBS.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 119
Disenrollment: Describes when a participant is being released from the Children’s
Waiver.
Duration: Describes how long the service will be delivered to the child/youth and/or
family. The duration of the service should correspond to the abilities of the child/family
and be reflective of the billing unit identified by service.
Evidence-Based: Services must utilize evidence-based practices where appropriate and
provide or enable continuing education activities to promote uptake of these practices.
Family: Family is defined as the primary caregiving unit and is inclusive of the wide
diversity of primary caregiving units in our culture. Family is a birth, foster, adoptive, or
self-created unit of people residing together, with significant attachment to the
child/youth, consisting of adult(s) and/or child(ren), with adult(s) performing duties of
parenthood/caregiving for the child(ren) even if the individual is living outside of the
home.
“Family of One”: A commonly used phrase to describe a child/youth that becomes
eligible for Medicaid through use of institutional eligibility rules for certain medically
needy individuals. These rules allow a budgeting methodology for children/youth to
meet Medicaid financial eligibility criteria as a “family of one,” using the child/youth’s
own income and disregarding parental income.
Frequency: Outlines how often the service will be offered to the child/youth and/or
family. Services may be delivered on a weekly, biweekly or monthly basis, according to
the needs of the child/youth and family.
HCBS/LOC Eligibility Determination: A tiered assessment where multiple factors
must be met for child/youth’s HCBS/LOC eligibility to be determined. To access
Children’s HCBS, a child/youth must meet target population, risk factors, and functional
criteria as described in the Children’s Waiver. The HCBS/LOC Eligibility Determination
is housed within the Uniform Assessment System (UAS).
Health Home Serving Children (HHSC): A State-designated program that provides
comprehensive care management, care coordination and health promotion,
comprehensive transitional care, patient and family support, referral to community
supports, and the use of Health Information Technology (HIT) to link services for
children/youth who meet HH eligibility criteria (i.e. 1) must be enrolled in Medicaid; 2)
must have two or more chronic conditions or one single qualifying chronic condition of
HIV/AIDS, Serious Mental Illness, Serious Emotional Disturbance, or Complex Trauma).
Home or Community Setting: Home setting or community setting means the setting in
which children/youth primarily reside or spend time, as long as it is not a hospital
nursing facility, Intermediate Care Facility (ICF), or psychiatric nursing facility. Note: this
is distinguished from a Home and Community based setting.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 120
Licensed Practitioner of the Healing Arts: An individual professional who is a
Licensed psychoanalyst, Licensed psychologist, Licensed Clinical Social Worker, Nurse
Practitioner, Physician, Physician Assistant or Psychologist and practicing within the
scope of their State license. LPHAs who sign off on the HCBS Attestation form must be
able to diagnose within their scope of practice.
4
a. Licensed Psychologist is an individual who is currently licensed and currently
registered as a psychologist by the New York State Education Department from
the New York State Education Department and who possesses a doctoral degree
in psychology.
b. Licensed Clinical Social Worker (LCSW) is an individual who is currently
licensed and registered as a Clinical Social Worker by the New York State
Education Department.
c. Nurse Practitioner is an individual who is currently certified as a nurse
practitioner by the New York State Education Department.
d. Physician is an individual who is licensed and currently registered as a physician
by the New York State Education Department.
e. Physician Assistant is an individual who is currently registered as a physician
assistant by the New York State Education Department.
f. Psychiatrist is an individual who is licensed and currently registered to practice
medicine in New York State, who (i) is a diplomat of the American Board of
Psychiatry and Neurology or is eligible to be certified by that Board, or (ii) is
certified by the American Osteopathic Board of Neurology and Psychiatry or is
eligible to be certified by that Board.
The following Licensed Practitioners, if under the supervision of an LPHA (as defined
above) are also eligible to complete the HCBS LPHA Attestation form:
a. Licensed Psychoanalyst is an individual who is currently licensed and currently
registered as a psychoanalyst by the New York State Education Department.
b. Licensed Marriage & Family Therapist (LMFT) is an individual who is licensed
and currently registered as a marriage and family therapist by the New York
State Education Department.
4
The LPHA Attestation form is no longer required for the Target Populations of Medically Fragile (MF) or
Developmental Disability who are Medically Fragile (DD/MF).

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 121
c. Licensed Mental Health Counselor (LMHC) is an individual who is licensed and
currently registered as a mental health counselor by the New York State
Education Department.
d. Licensed Creative Arts Therapist (LCAT) is an individual who is licensed and
currently registered as a Creative Arts Therapist by the New York State
Education Department possesses a creative arts therapist permit from the New
York State Education Department.
e. Registered Professional Nurse is an individual who is licensed and currently
registered as a registered professional nurse by the New York State Education
Department.
g. Licensed Master Social Worker (LMSW) is an individual who is either currently
registered as a Licensed Master Social Worker (LMSW) by the New York State
Education Department.
Institutionalization: Admission to a hospital (medical or psychiatric), RTF, ICF/IID or
nursing facility.
Integrated: Success for children/youth requires both integrated and effective treatment.
Initial and on-going collaboration between providers and natural supports is fundamental
to enhancing resiliency, meeting the imperatives of developmental stages, and promoting
wellness for each child/youth and their family.
Licensed Occupational Therapist: An individual who is licensed and currently
registered as an Occupational Therapist by the New York State Education Department
that assists people across the lifespan to do the things they want and need to do
through the therapeutic use of daily activities (occupations). Common occupational
therapy interventions include helping children with disabilities to participate fully in
school and social situations, helping people recovering from injury to regain skills, and
provide customized interventions to improve the person’s ability to perform daily
activities and reach their goals.
Medicaid Eligible Child: Any child/youth in New York State who is eligible for
Medicaid, whether eligible via income consideration, medically needy definitions, or
categorical eligibility (e.g., foster care).
Medicaid Managed Care Plan: The mainstream Medicaid Managed Care Plan or HIV
Special Needs Plan in which the child/youth is enrolled on the date of service, or which
the child/youth has selected for enrollment and has provided written consent to share
protected health information with prior to enrollment.
Medically Fragile: For the purposes of this Manual and Children’s HCBS a “medically
fragile child” is defined as an individual who is under 21 years of age whose target

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 122
population, risk factors, and functional criteria align with the Medically Fragile or
Medically Fragile and DD LOC criteria.
Multisystem involved: Two or more child systems including child welfare, juvenile
justice, Department of Homeless Services and/or other homeless services, OASAS
clinics or residential treatment facilities or institutions, OMH clinics or residential facilities
or institutions, OPWDD services or residential facilities or institutions, or having an
established IEP through the school district.
Natural Supports: Individuals and informal resources that a family/caregiver can
access, independent of formal services. These supports are a significant source of
culturally relevant emotional support and caring friendships for children/youth and
families. Natural supports can be short-term or long-term and are usually sustainable
and available to the child/youth and family/caregiver after formal services have ended.
Out of Home Placement: Residential Rehabilitation Services for Youth (RRSY),
Residential Treatment Facility (RTF), Residential Treatment Center (RTC), or other
congregate care setting, such as SUD residential treatment facilities, group residencies,
institutions in the OCFS system, or hospitalization.
Parent, guardian, or legally authorized representative: The individuals who have
custody/guardianship of the child/youth and who are able to consent to the child/youth’s
services, when the child/youth is not of age to self-consent or does not have the mental
capacity to self-consent to services. (Youth who are 18 years or older or under the age
of 18 years old who are pregnant, married, or a parent can self-consent for the HH, C-
YES, and HCBS).
5
Note: When developing the POC, foster parents are encouraged to provide input.
The final signature for the POC needs to be signed by the
child/parent/guardian/legally authorized representative.
Person-Centered Care: Services should reflect a child/youth and family’s goals and
personal desired outcomes, and emphasize shared decision-making approaches that
empower families, provide choice, and minimize stigma. Services should be designed to
optimally treat illness, improve clinical and psychosocial outcomes, and emphasize
wellness and attention to the family’s overall well-being and the child/youth’s full
community inclusion. To be person-centered, services must be culturally appropriate,
child/youth guided, and relevant.
Physical Disability: “Disability" under Social Security is based on one’s inability to
work. A person is considered disabled under Social Security rules if they cannot do
work that s/he did before, SSA decides that s/he cannot adjust to other work because of
5
This guidance does not change or modify the applicability of any law, regulation, or court order
regarding custody, guardianship, right to consent to health care, or right to protected health information.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 123
his/her medical condition(s), and his/her disability has lasted or is expected to last for at
least one year or to result in death.
Recovery-Oriented: Services should be provided based on the principle that all
individuals have the capacity to recover from mental illness and/or substance use
disorders. Specifically, services should support the acquisition of living, vocational, and
social skills and be offered in home and community-based settings that promote hope
and encourage each person to establish an individual path towards recovery.
Restoration: Returning to a previous level of functioning.
School Setting: The place in which a child/youth attends school.
Scope: The service components and interventions being provided and utilized to
address the identified needs of the child/youth.
Serious Emotional Disturbance (SED): A designated mental illness diagnosis
according to the most current edition of the Diagnostic and Statistical Manual of Mental
Disorders (DSM) for a child/youth who has experienced functional limitations due to
emotional disturbance over the past 12 months on a continuous or intermittent basis.
The functional limitations must be moderate in at least two of the following areas or
severe in at least one of the following areas:
• Ability to care for self (e.g. personal hygiene; obtaining and eating food;
dressing; avoiding injuries)
• Family life (e.g. capacity to live in a family or family like environment;
relationships with parents or substitute parents, siblings and other relatives;
behavior in family setting)
• Social relationships (e.g. establishing and maintaining friendships;
interpersonal interactions with peers, neighbors and other adults; social skills;
compliance with social norms; play and appropriate use of leisure time)
• Self-direction/self-control (e.g. ability to sustain focused attention for a long
enough period of time to permit completion of age-appropriate tasks;
behavioral self-control; appropriate judgment and value systems; decision-
making ability)
• Ability to learn (e.g. school achievement and attendance; receptive and
expressive language; relationships with teachers; behavior in school)
Service Goal: A general statement of outcome relating to the identified need for the
specific intervention provided.
Service Provider: Individuals/organizations that provide and are paid to provide
services to the child/youth and family/caregiver.
Substance Use Disorder (SUD): A diagnosis of a substance use disorder is based on
a pathological pattern of behaviors related to the use of the substance. The diagnosis of

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 124
a substance use disorder is based on criteria defined in the current Diagnostic and
Statistical Manual of Mental Disorders (DSM) and can be applied to all ten classes of
drugs (i.e. alcohol; cannabis; hallucinogens; inhalants; opioids; sedatives; hypnotics;
anxiolytics; stimulants; tobacco; and other (or unknown) substances).
Trauma-Informed: Trauma-informed services are based on an understanding of the
vulnerabilities or triggers experienced by trauma survivors that may be exacerbated
through traditional service delivery approaches so that these services and programs can
be modified to be more supportive and avoid re-traumatization. All programs should
engage all individuals with the assumption that trauma has occurred within their lives
(SAMHSA, 2014).
Youth: Individuals generally 14 years of age and older.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 125
Appendix B: CMS Final Rule on HCBS Settings
According to CMS requirements, any residential or non-residential setting where
children/youth receive HCBS must have the following qualities:
1. The setting is integrated in and supports full access of individuals receiving
Medicaid HCBS to the greater community, including opportunities to seek
employment and work in competitive integrated settings, engage in community
life, control personal resources, and receive services in the community, to the
same degree of access as individuals not receiving Medicaid HCBS.
2. The setting is selected by the individual from among setting options including
non-disability specific settings and an option for a private unit in a residential
setting. The setting options are identified and documented in the person-
centered service plan and are based on the individual's needs, preferences,
and, for residential settings, resources available for room and board.
3. Ensures an individual's rights of privacy, dignity and respect, and freedom
from coercion and restraint.
4. Optimizes, but does not regiment, individual initiative, autonomy, and
independence in making life choices, including but not limited to, daily
activities, physical environment, and with whom to interact.
5. Facilitates individual choice regarding services and supports, and who provides
them.
In a provider-owned or controlled residential setting, in additional to the qualities
specified above, the following conditions must be met:
6. The unit or dwelling is a specific physical place that can be owned, rented, or
occupied under a legally enforceable agreement by the individual receiving
services, and the individual has, at a minimum, the same responsibilities and
protections from eviction that tenants have under the landlord/tenant law of the
State, county, city, or other designated entity. For settings in which landlord
tenant laws do not apply, the State must ensure that a lease, residency
agreement or other form of written agreement will be in place for each HCBS
participant, and that the document provides protections that address eviction
processes and appeals comparable to those provided under the jurisdiction's
landlord tenant law.
7. Each individual has privacy in their sleeping or living unit:
o Units have entrance doors lockable by the individual, with only appropriate
staff having keys to doors.
o Individuals sharing units have a choice of roommates in that setting.
Individuals have the freedom to furnish and decorate their sleeping or
living units within the lease or other agreement.
8. Individuals have the freedom and support to control their own schedules and
activities, and have access to food at any time.
9. Individuals are able to have visitors of their choosing at any time.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 126
10. The setting is physically accessible to the individual.
o Any modification of the additional conditions specified in items 1 through 4
above, must be supported by a specific assessed need and justified in the
person-centered service plan. The following requirements must be
documented in the person-centered service plan:
o Identify a specific and individualized assessed need.
o Document the positive interventions and supports used prior to any
modifications to the person-centered service plan.
o Document less intrusive methods of meeting the need that have been tried
but did not work.
Provider-owned and controlled standards 6-10 are the only standards that are
modifiable, under certain conditions.
Include a clear description of the condition that is directly proportionate to the specific
assessed need.
o Include regular collection and review of data to measure the ongoing
effectiveness of the modification.
o Include established time limits for periodic reviews to determine if the
modification is still necessary or can be terminated.
o Include the informed consent of the individual.
o Include an assurance that interventions and supports will cause no harm
to the individual.
Provider-owned and controlled standards 6-10 are the only standards that are
modifiable, under certain conditions.
For standards 6-10, there cannot be restrictive rules that apply to all Children’s Waiver
recipients. Examples of restrictive rules include, set visitor hours in a residential setting,
and only one time slot food/snacks are available. Standards 6-10 may be modified on a
case-by case basis for a specific individual if it is done:
• When there is a specific need that has been identified that a participant requires
staff support with (i.e., a diagnosis is not enough information to support modifying
a standard)
• On a time-limited basis (reassessing periodically to see if the modification is still
needed)
• After less restrictive and more positive approaches were tried and failed
Modification example: Jane requires assistance with managing her access to
food/snacks due to her tendency to eat frequently, which raises her blood sugar levels.
Staff tried counseling her but were not successful. With her (or her
guardian/representative’s) informed consent, staff will support her with accessing the
snack cabinet for at least six months, documenting this in her plan.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 127
The CMS Final Rule (§441.301(c)(4) and §441.710) defines the qualities that all home
and community-based settings must possess in order to be in compliance with the rule.
In the final rule, CMS also clarifies which settings do NOT qualify as home and
community-based settings.
According to CMS, settings that DO NOT MEET the definition of being home and
community based are:
• A nursing facility;
• An institution for mental diseases;
• An intermediate care facility for individuals with intellectual disabilities;
• A hospital; or
• Any other locations that have qualities of an institutional setting, as determined
by the Secretary.
In addition, the final rule 441.301(c)(5)(v) specifies that the following settings are
presumed to have the qualities of an institution (and therefore likely do not meet the
HCBS standard without documentation to support otherwise):
• Any setting that is located in a building that is also a publicly or privately operated
facility that provides inpatient institutional treatment,
• Any setting that is located in a building on the grounds of, or immediately
adjacent to, a public institution, or
• Any other setting that has the effect of isolating individuals receiving Medicaid
HCBS from the broader community of individuals not receiving Medicaid HCBS.
Any modifications of these additional conditions must be supported by a specific
assessed need and justified in the person-centered service plan.
The federal HCBS regulations also require that the Person-Centered Service Planning
(PCSP) process must be met as outlined in the following requirements:
• Reflect
that the setting in which the individual resides is chosen by the individual.
o The PCSP must ensure that the setting chosen by the individual is
integrated in and supports full access of individuals receiving Medicaid
HCBS to the greater community
• Be timely and occur at least annually at times and locations of the individual’s
convenience
• Assist the person in achieving outcomes they define for themselves, and in the
most integrated community setting(s) they desire
• Ensure delivery of services in a manner that reflects personal preferences and
choices

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 128
• Help promote the health and welfare of those receiving services
• Take into consideration the culture of the person served
• Include strategies for solving disagreement(s)
• Offer choices regarding the services and supports the person receives, and from
whom
• Reflect the individual’s strengths, preferences, needs (both clinical and support),
and desired outcomes
• Provide necessary information and support to the individual to ensure that they
can direct their planning process as much as possible
• Include people chosen by the individual
• Reflect services and supports (paid and unpaid) that will assist the individual to
achieve identified goals, and the providers of those services and supports,
including natural supports (unpaid supports that are provided voluntarily to the
individual in lieu of 1915(c) HCBS waiver services and supports).
• Be understandable to the individual receiving services and supports, and the
individuals important in supporting him or her. At a minimum, the plan must be
written in plain language and in a manner that is accessible to individuals with
disabilities and person who are limited English proficient.
• Identify the individual and/or entity responsible for monitoring the plan.
o Indicate what entity or person will monitor the primary or main person-
centered plan
• Be distributed to the child/youth and other people involved in the plan.
• Include those services, the purpose or control of which the individual elects to
self-direct and prevent the provision of unnecessary or inappropriate services
and supports.
o Provide a method for the individual to request updates to their plan
• Document that any modification of the additional conditions, under 42 CFR
441.301(c)(4)(vi)(C) and (D), must be supported by a specific assessed need and
justified in the PCSP. Any deviation from the standards at 42 CFR
441.301(c)(4)(vi)(C) and (D) will be justified and documented in the care plan
with updated frequency, scope, and duration, and will be updated no less
frequently than every 6 months.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 129
APPENDIX C: PRIOR/CONCURRENT AUTHORIZATION GRID
HCBS
Prior
Authorization
Concurrent
Authorization
Additional Guidance
Caregiver/Family
Advocacy and
Support Services
No
Yes
Eligibility determination and plan of care
(POC) are the only required elements for
initial authorization. MMCPs will reimburse
for initial authorization of 96 units or a total
of 24 hours of service for a period of 60 days
from the time that the MMCP receives
notification from the HCBS provider.
Community
Habilitation
No
Yes
Eligibility determination and POC are the
only required elements for initial
authorization. MMCPs will reimburse for
initial authorization of 96 units or a total of 24
hours of service for a period of 60 days from
the time that the MMCP receives notification
from the HCBS provider.
Day Habilitation
No
Yes
Eligibility determination and POC are the
only required elements for initial
authorization. MMCPs will reimburse for
initial authorization of 96 units or a total of 24
hours of service for a period of 60 days from
the time that the MMCP receives notification
from the HCBS provider.
Prevocational
Services
No
Yes
Eligibility determination and POC are the
only required elements for initial
authorization. MMCPs will reimburse for
initial authorization of 96 units or a total of 24
hours of service for a period of 60 days from
the time that the MMCP receives notification
from the HCBS provider.
Supported
Employment
No
Yes
Eligibility determination and POC are the
only required elements for initial
authorization. MMCPs will reimburse for
initial authorization of 96 units or a total of 24
hours of service for a period of 60 days from
the time that the MMCP receives notification
from the HCBS provider.
Environmental
Modifications
Yes
Yes
$25,000 annual calendar year limit;
addressed in separate guidance
Vehicle Modifications
Yes
Yes
$25,000 annual calendar year limit;
addressed in separate guidance

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 130
HCBS
Prior
Authorization
Concurrent
Authorization
Additional Guidance
Adaptive and
Assistive Technology
Yes
Yes
$15,000 annual calendar year limit;
addressed in separate guidance
Palliative Care
(Counseling and
Support Services,
Pain and Symptom
Management,
Expressive Therapy,
Massage Therapy)
Yes
Yes
Palliative care benefits may not duplicate
Hospice or other State Plan benefits
accessible to participants.
Expressive therapy limited to the lesser of
four appointments per month or 48 units per
calendar year.
Massage therapy limited to no more than 12
appointments per calendar year.
Counseling and Support limited to the lesser
of five appointments per month or 60 hours
per calendar year.
Limits can be exceeded when medically
necessary.
Planned Respite
No
Yes
Eligibility determination and POC are the
only required elements for initial
authorization. MMCPs will reimburse for
initial authorization of 96 units or a total of 24
hours of service for a period of 60 days from
the time that the MMCP receives notification
from the HCBS provider. Billing for Respite
must be based on in-person interactions with
the Waiver child.
Respite billing is limited to six (6) hours (24
units) per child per day.
For Individual Respite the maximum of six
(6) hours (24 units) is equivalent to a daily
individual per diem rate.
Group Respite billing is limited to six (6)
hours (24 units) per child per day.
Planned Respite will be authorized for
utilization for no more than 7 consecutive
days per calendar year. Anything beyond
this utilization will require concurrent review.
Crisis Respite
No
Yes
No prior authorization is needed; MMCP
may require a notification of care and require
concurrent review if utilization exceeds 72
hour stay.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 131
APPENDIX D: UTILIZAT ION MANAGEMENT/MEDICAL NECESSIT Y
GUIDELINES FOR CHILDREN ’S ALIGNED HOME AND COMMUNIT Y
BASED SERVICES
Admissions Criteria
Continued Stay Criteria
Discharge Criteria
6
All of the following criteria must
be met:
1. The child/youth must meet
Level of Care (LOC) Eligibility
Determination criteria to be
eligible for HCBS.
2. The child/youth must meet
risk and functional criteria as
evidenced by the completion
and affirmative outcome of the
HCBS Eligibility Determination
tool or the ICF-IDD Level of
Care determination.
3. The HCBS supports the
child/youth’s efforts to maintain
the child in the home,
community, and school and is
reflected in the Plan of Care
(POC).
4. The child/youth must be
willing to receive HCBS.
5. There is no alternative level of
care or cooccurring service that
would better address the
child/youth’s clinical and
functional needs.
6. The child/youth must live in
an appropriate setting in
accordance with Federal and
State guidance.
All of the following criteria must
be met:
1. Child/youth continues to meet
admission criteria and an
alternative service would not
better serve the child/youth.
2. A POC has been developed,
informed and signed by the
child/youth, Health Home care
manager or Independent Entity,
and others responsible for
implementation.
3. Interventions are timely,
needbased and consistent with
evidence based/best practice
and provided by a designated
HCBS provider.
4. Child/youth is making
measurable progress towards a
set of clearly defined goals Or
There is evidence that the POC
and/or provider treatment plan
are modified to address the
barriers in treatment progression
Or Continuation of services is
necessary to maintain progress
already achieved and/or prevent
deterioration.
5. Family/guardian/caregiver is
participating in treatment, where
appropriate.
Criteria #1, 2, 3, 4, 5 or 6 are
suitable; criteria #7 is
recommended, but optional:
1. Child/youth no longer meets
admission criteria and/or meets
criteria for another, more
appropriate service, either more
or less intensive.
2. Child/youth or
parent/guardian withdraws
consent for treatment.
3. Child/youth is not participating
in the POC development and/or
utilizing referred services.
4. Child/youth’s needs have
changed and current services
are not meeting these needs.
5. Child/youth’s goals would be
better served with an alternate
service and/or service level.
6. Child/youth’s POC goals have
been met.
7. Child/youth’s support system
is in agreement with the
aftercare service plan.
6
As described in the NYS 1115 MRT Waiver, each child will receive the beneficiary protections granted
under Medicaid including notices of denials and the right to file appeals when denied HCBS enro llment or
receiving a denial or limitation for a requested service.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 132
APPENDIX E: TABLE OF RESPONSIBILITIES FOR HCBS WORKFLOW
Milestone Event
Responsible Entity
Enrolled in MMCP
FFS Medicaid
Enrolled
in HH
Opt-out
of HH,
Served
by C-YES
Enro
lled
in
HH
Opt-out
of HH,
Served
by C-
YES
HCBS Provider referral
HHCM
C-YES
HHC
M
C-YES
Notifies MMCP and HHCM of
First Appointment
HCBS
Provider
HCBS
Provider
N/A
N/A
On-going POC updates
HHCM
MMCP
HHC
M
C-YES
Request Authorization for Services
HCBS
Provider
HCBS
Provider
N/A
N/A
Major life event requiring POC
update
HHCM
MMCP
HHC
M
C-YES
Monitoring access to care
MMCP
MMCP
HHC
M
C-YES
Annual reassessment
HHCM
C-YES
HHC
M
C-YES

Appendix F: T raining Grid
HCBS providers must have the following in place:
• Written policies and procedures that describe staff orientation
• Mandatory training and other offered trainings for staff
• Staff have the required training to provide care that is trauma informed, culturally
competent, and appropriate to the developmental level of the population served
• Maintain documentation of staff completion of required trainings in accordance
with the Children’s HCBS Provider Manual and be able to provide training
records to the State upon request to review. Additional information on State
reviews will follow.
Mandatory training components can be delivered in one training or a series of trainings.
The HCBS provider will need to maintain training records and training curriculum as
evidence of meeting the requirements. Providers can seek community training available
to them, partner with another agency, and/or develop a training within their organization
to address the required training components. Mandated Reporter training must be
completed prior to service delivery, and all other trainings must be completed within six
months of hire date.
Training Required
Training Components Required
Mandated Reporter
Staff members are required to completed Mandated Reporter training prior to
delivering HCBS.
Personal Safety/
Safety in the
Community
• Safety awareness/office and community safety
• Prevention/risk assessment for the field visits
• Use of safety technology (e.g. use of mobile phones)
• Transporting children/youth/families
• Safety training/self-protection strategies
• De-escalation techniques
• Emergency protocols and resources (includes agency policies that
address emergency procedures while delivering HCBS in the
community and resources available to staff in the event of an
emergency e.g. 911, on-call supervision)
• Post incident reporting and response (includes agency policies that
address incident reporting and procedures for staff providing HCBS in
the community)
• To ensure safety and protection of child/ youth, trainings will address
professional boundaries, relationship boundaries, trauma, and a code
of ethics for staff working with children/ youth.
Strength Based
Approaches
• What are strength-based approaches?
• Person-centered planning
• Strength based information gathering
• Collaboration with child/youth/family and community (e.g. family-
guided, youth-driven, etc.)
• Identifying strengths, protective factors and assets
• Cultural and linguistic competence
Suicide Prevention
• Myths and misconceptions of suicide
• Risk factors

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 134
Training Required
Training Components Required
• High risk populations
• Warning signs
• How to help (assess for risk of suicide and harm, encourage
appropriate professional help)
• Action/safety planning identify resources in the community (i.e.,
emergency services and mental health professionals))
Domestic Violence
Signs and Basic
Interventions
• What is domestic violence?
• Prevalence
• Types of abuse
• Cycle of violence/pattern of abuse
• Domestic violence effects on children
• How to help
• Action/safety planning
Trauma Informed Care
• What is trauma?
• Prevalence/findings (e.g. ACES)
• Impact of trauma
• Trauma informed care approach (i.e., strength-based, person and
family centered, culturally aware, meeting language needs,
performing collaborative and coordinated care, etc.).

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 135
Appendix G: Service Animal Guidance
The NYS Children’s Waiver recognizes the importance of service animals in the lives of
individuals with various disabilities such as those that substantially limit one or more
major life activities. Service animals are more than pets, and more than companions;
they are a working animal and the important work they do enhances independence for
children/youth with physical, cognitive, and developmental disabilities. Service animals
perform some of the functions and tasks that the individual with a disability cannot
perform for him or herself.
Service animal is defined by the Americans with Disabilities Act (ADA) Title II (State and
local government services) and Title III (public accommodations and commercial
facilities) as, “any dog that is individually trained to do work or perform tasks for the
benefit of an individual with a disability, including a physical, sensory, psychiatric,
intellectual, or other mental disability.” The work or tasks performed by a service animal
must be directly related to the individual's disability. These tasks may include, but are
not limited to:
• assisting individuals who are blind or have low vision with navigation and other
tasks,
• alerting individuals who are deaf or hard of hearing to the presence of people or
sounds,
• providing non-violent protection or rescue work,
• calming a person with Post Traumatic Stress Disorder during an anxiety attack,
• pulling a wheelchair,
• protecting a person who is experiencing a seizure,
• alerting individuals to the presence of allergens,
• retrieving items such as a telephone or medicine or reminding someone to take
prescription medications,
• providing physical support and assistance with balance and stability to individuals
with mobility disabilities, and,
• helping persons with psychiatric and neurological disabilities by preventing or
interrupting impulsive or destructive behaviors.
Additional guidance on the ADA’s service animal provisions can be found in the
following publications:
• Title III Regulation Supplement - Current as of January 17, 2017
Nondiscrimination on the Basis of Disability by Public Accommodations and in
Commercial Facilities
• Frequently Asked Questions about Service Animals and the ADA
• Public Access Test Checklist for Service Animals

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 136
Dogs whose sole function is to provide comfort or emotional support do not qualify as
service animals under the ADA.
This definition does not affect or limit the broader definition of “assistance animal” under
the Fair Housing Act or the broader definition of “service animal” under the Air Carrier
Access Act.
• U.S. Department of Housing and Urban Development: Service Animals and
Assistance Animals for People with Disabilities in Housing and HUD-Funded
Programs, FHEO-2013-01 (April 25, 2013)
• 49 U.S.C. § 41705; see “Nondiscrimination on the Basis of Disability in Air
Travel,” 14 C.F.R. Part 382 (United States Department of Transportation 2014)
Nondiscrimination on the basis of disability in air travel
The ADA requires that service animals be under the control of the handler at all times
and be harnessed, leashed, or tethered, unless these devices interfere with the service
animal's work or the individual's disability prevents him from using these devices.
Individuals who cannot use such devices must maintain control of the animal through
voice, signal, or other effective controls.
Policy
This policy provides guidance on the use and funding of service animals by New York
Children’s Waiver participants. Service animals funded by the New York Children’s
Waiver must meet the following criteria.
• The request for funding must following the Guidelines for Authorizing Assistive
Technology including:
o Documenting the need for assistance in the individual’s POC
o A physician’s order stating the need for assistance
o Clinical justification from the appropriate clinician and/or service specialist
to assess the individual’s need for the request service animal and to
indicate how the service animal meets the needs of the individual in the
most cost effective manner; the clinical justification must include a home
environment assessment to determine if there are any obstacles to the
use of the service animal in the home
o Submitting the Description and Cost Project Form to the Managed Care
Organization (MCO) or LDSS as appropriate
• A licensed veterinarian shall be engaged to certify the following:
o The service animal is trained to perform the activities needed by the
individual as identified in the POC and clinical justification. See Appendix
1 for ADA requirements regarding training.
o The service animal must pass obedience level 3 and/or the national public
access test, be registered and licensed as required by local ordinance,

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 137
and current on all vaccinations. See Appendix 2 for a National Public
Access checklist for basic obedience requirements.
o Assistance teams are tested initially and verified every 24 months to
ensure they continue to work well together and accomplish the identified
tasks. Additional training may be conducted if medical necessity is
determined based on the changing needs of the individual.
Services include:
A. Evaluation of the assistive technology/service animal needs of a participant,
including a functional evaluation of the impact of the provision of appropriate
assistive technology and appropriate services to the participant in the
customary environment of the participant
B. Services consisting of purchasing assistive technology devices/service animal
for the participant
C. Services consisting of selecting, designing, fitting, customizing, adapting,
applying, maintaining, repairing, or replacing assistive technology devices for
the participant
D. Training or technical assistance for the participant, or, where appropriate, the
family members, guardians, advocates, or authorized representatives of the
participant
E. Training or technical assistance for professionals or other individuals who
provide services to, employ, or are otherwise substantially involved in the
major life functions of participant
Service animals are expected to be a one-time only purchase. Replacements
will be paid if documented as a necessity and approved by the State or its
designee. Maintenance will only be approved when it is the most cost effective
and efficient means to meet the need, and other options are not available
through the 1905(a) Medicaid State Plan or third-party resources.
• Refresher training for the service animal every 24 months is an
allowable expense. Additional training for the service animal would
be paid for if warranted by a change in the participant’s condition
and the appropriate documentation is provided.
• Services available through the Children’s Wavier cannot duplicate
services otherwise available through the 1915(a) Medicaid State
Plan or other federal/state funding streams. Equipment must be
beyond the scope of Durable Medical Equipment (DME).
Vocational Rehabilitation funding must be sought prior to Medicaid
funding.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 138
• All service animal costs require prior approval from the LDSS in
conjunction with DOH or the MCO. As a type of Adaptive and
Assistive Technology, service animal requests are subject to a
$15,000 per calendar year soft limit. The State may consider
exceptions when medically necessary, including but not limited to a
significant change in the participant’s needs or capabilities.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 139
Appendix H: Medicaid Eligibility Guidance
Medicaid Eligibility Status Impact on HCBS Eligible Children
This guidance is to provide clarification regarding Medicaid eligibility related to the
Children’s Waiver and changes due to the approved 1115 Waiver. This guidance
explains how the receipt of services are related to waiver and Medicaid eligibility for
“Family of One” children. Specifically, the guidance explains when either Care
Management or HCBS are required for children to obtain eligibility for the Children’s
Waiver and Medicaid eligibility.
Together, the 1915(c) Children’s Waiver and the 1115 MRT waiver authorities provide
Medicaid eligibility for children meeting the HCBS eligibility criteria under the Children’s
Waiver. The 1915(c) Children’s Waiver was implemented on April 1, 2019 and
consolidated six children’s HCBS waivers into one comprehensive waiver. The
children’s 1115 MRT waiver amendment was approved on August 2, 2019 to allow
“Family of One” to children meeting the 1915(c) Children’s Waiver criteria, who only
receive HH Care Management services, to retain their Waiver eligibility status. This
allows the child to have Medicaid eligibility determined under a “Family of One” budget if
not otherwise eligible under community budgeting. The two authorities allow all children
and youth eligible for the Waiver to have:
• Greater ease of enrollment into Children’s Waiver
• Access to all HCBS (Home and Community Based Services) as needed
• Greater flexibility for HCBS to be delivered in natural environments for better
outcomes
• Retain eligibility for Medicaid if “Family of One” and eligible for the Children’s
Waiver
HCBS Care Management
All children/youth enrolled in the Children’s Waiver need care coordination services. HH
comprehensive care management provides the care coordination service required
under the Children’s Waiver. If a child/youth is eligible for the Children’s Waiver, they
automatically receive HH care management and a separate HH eligibility determination
is not needed. As HH is an optional benefit, a child/family can opt-out of HH services.
For a child/youth who opts-out of HH services, their care coordination will be provided
by the Independent Entity of C-YES and, if enrolled in MMCP, by the MMCP care
manager. A child/youth who needs HCBS, but is not enrolled in Medicaid, will be
referred to C-YES who will determine HCBS/LOC Eligibility and assist with establishing
Medicaid eligibility. Once the child/youth is HCBS and Medicaid eligible, the child/family
can choose who they would like to provide care coordination, HH or C-YES.
“Family of One” Medicaid Eligibility
“Family of One” is a phrase used to describe a child that becomes eligible for Medicaid
through the use of institutional eligibility rules. If a child is not otherwise eligible for
Medicaid when counting parental income (and/or resources, if applicable), these rules
allow for the child to have Medicaid eligibility determined as a “Family of One”, using

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 140
only the child’s own income (and resources, if applicable). If a child/youth is not
currently receiving Medicaid due to parental income (and/or resources, if applicable)
and the child/youth is in need of waiver services, when the child/youth is found
HCBS/LOC eligible and able to obtain a capacity slot, then based upon waiver eligibility,
the child will have Medicaid eligibility determined as a “Family of One”.
Note: There is a hierarchy that must be used in determining a child/youth’s Medicaid
eligibility. This hierarchy requires that parental income information be included in the
child’s Medicaid application, even if the income is not ultimately used under a “Family of
One” budget. If the child is in a medically fragile diagnostic group or certified disabled,
parental resource information and any income of non-waiver siblings under age 18 will
also need to be included on the Medicaid application. In addition, as part of the
Medicaid eligibility determination, children/youth in a medically fragile diagnostic group
will have a disability determination made by the State Disability Review Team, if
disability status has not already been established by the Social Security Administration.
Pending the disability determination, Medicaid coverage will be authorized for such
children under an ADC-related “Family of One” budget, but the child/family will be
required to comply with the disability determination.
Once a child/youth obtains Medicaid under “Family of One” they must be
continually enrolled and receiving HCBS or HH care management services (as
noted below) to continue their “Family of One” eligibility for the Medicaid. Any
“Family of One” child/youth can also receive other Medicaid services (i.e. State Plan
services) such as Private Duty Nursing, CFTSS, pharmacy, hospital, physician, etc.
Once a child/youth with “Family of One” Medicaid is no longer eligible for the Children’s
Waiver and/or doesn’t receive HCBS or HH care management, they may lose their
Medicaid eligibility altogether or they may have to meet a large spenddown each month
in order to access Medicaid services.
“Community Eligible Medicaid” is when a child/youth is determined eligible for Medicaid
based on a budget that includes family income (and resources when applicable) in the
budget calculation (MAGI, ADC-related or SSI-related community budget) and is not
tied to Children’s Waiver eligibility.
“Family of One” and Care Management
Children/youth who meet HCBS/LOC eligibility (target, risk and functional) and obtain a
capacity slot, must be connected and in receipt of at least one HCBS on a monthly
basis. Under the new Children’s Waiver/1115 Waiver authorities, any “Family of One”
(with a KK code) child/youth meeting the eligibility criteria for the 1915(c) Children’s
Waiver must receive HH care management services or HCBS.
For all children/youth whether Community Eligible or “Family of One” Medicaid, a
determination of services necessary must be supported by an assessment of needs and
strengths with the child/family and their identified care team as developed in the person-
centered POC. The Children’s Waiver offers an expanded array of service options for

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 141
children and families. Based on the needs and priorities of the family, the HHCM can
link the family with the appropriate services to best support their needs, including
Private Duty Nursing under the Medicaid State Plan. HCBS found necessary to maintain
the child/youth in their home should be supportive and appropriate for the child/youth’s
needs. The child/youth’s care record must reflect the needs and necessary services
through appropriate documentation.
If an HCBS/LOC eligible child/youth has no need for an HCB Service, and is only
eligible for Medicaid under a “Family of One” budget, then similar to the previous HCBS
Waivers, if the child/youth receives HH Care Management in order to be maintained in
the home, the child/youth qualifies for the Children’s Waiver. HH care management may
be the sole service for a “Family of One” child/youth to continue waiver eligibility and
have access to other needed Medicaid services. In these cases, only HH
comprehensive care management with monthly in-person monitoring, regardless of
acuity level, is allowable. C-YES/MMCP care coordination will not meet this
requirement; this restriction must be explained to the child/family. In contrast, a
community Medicaid eligible child must receive an HCBS waiver service monthly to
continue waiver eligibility.
See Children’s Waiver - HCBS Waiver Eligibility Service Requirements and Children’s
Waiver - Medicaid Eligibility Status Impact on HCBS Eligible Children for more details
regarding this policy.
HH care management for an HCBS/LOC and “Family of One” eligible child/youth, in
absence of any other HCBS waiver service, requires that the POC outline frequency,
scope and duration for the HH care management services.
Figure 1: “Family of One” children may obtain waiver and Medicaid eligibility in two
ways:
As noted in the figure above, children and youth meeting the Children’s Waiver eligibility
criteria, assigned to a capacity slot, and receiving HCBS, may receive care
management either through HH or C-YES/MMCP based upon child/family choice. The
difference between HH comprehensive care management and C-YES HCBS care
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 142
coordination, with MMCP care management as applicable. must be explained to the
child/family so an informed choice can be made.
Disenrollment from Waiver
A child/youth who does not meet the Children’s Waiver eligibility criteria and who has no
need for HCBS or HH care management, should be disenrolled from the Children’s
Waiver. In addition, once a child/youth has been successful in reaching the goal of the
HCBS (i.e. Environmental Modification) and no other HCBS is needed, possible
discharge from the waiver authorities should be reviewed and determined if other HCBS
goals are not appropriate.
Figure 2: Disenrollment from Waiver if child/youth does not meet Children’s Waiver
criteria or need HCBS/HH services.
“Family of One” children/youth (with a KK code) who do not require at least one HCBS
monthly but continues to meet the eligibility criteria for the Children’s Waiver must
receive HH Care Management and have HCBS in their plan of care for health and
welfare monitoring to maintain their Medicaid eligibility.
If a child/youth has community Medicaid (without a KK code) and does not need HCBS
monthly but needs State Plan services or other supports to be safe and supported at
home and in their community, will be disenrolled from the Children’s Waiver. The
child/youth will retain Medicaid eligibility to receive all other medically necessary
Medicaid services.
Receipt of HCBS or HH Care Management Services
If State Plan Services such as CFTSS or Community First Choice Options (CFCO) can
meet a child/youth’s needs, then these services must be accessed prior to HCBS
Services. This does not prohibit a child/youth from receiving both State Plan services
and HCBS at the same time, as long as it is reflective of the child/youth’s needs in the
person-centered POC and does not result in duplicative services. The child/youth’s
needs should be continually monitored and reviewed with the family and treating service
providers. If it is determined that the child/youth’s needs are met via non-HCBS
programs and/or services, HCBS discharge should be explored.
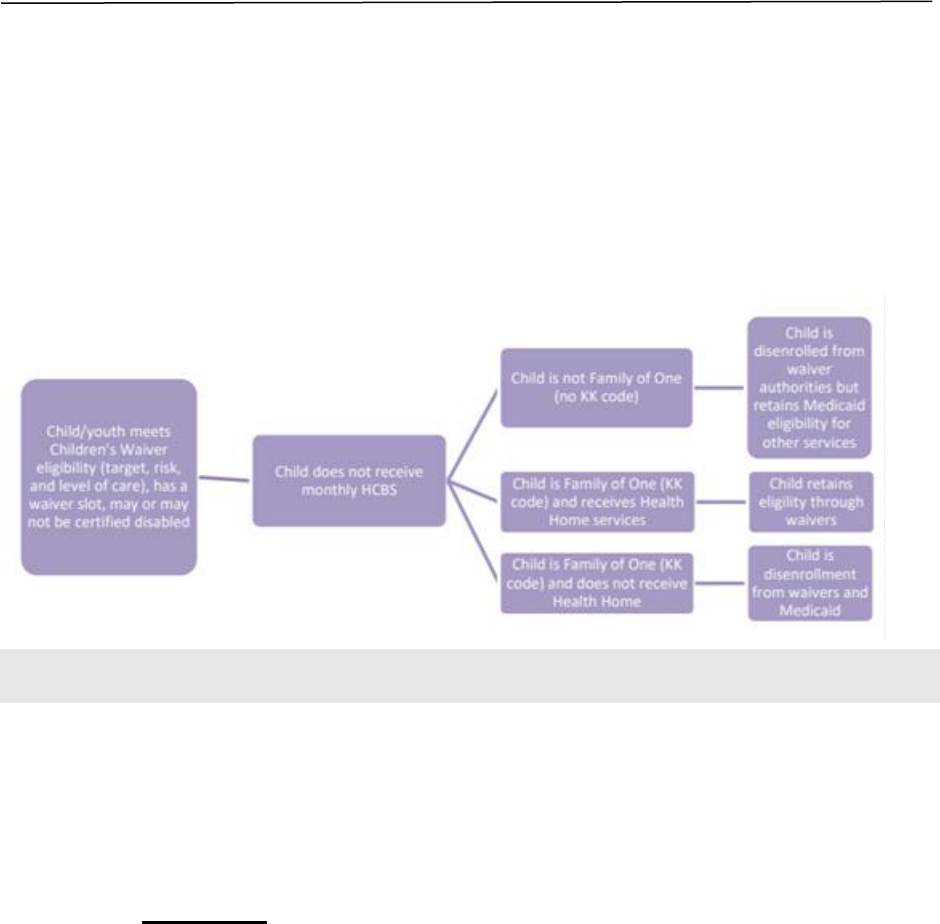
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 143
If State Plan or CFCO services alone meet the needs of the child/youth, then the
child/youth should not be enrolled in the Children's Waiver unless the child/youth is
only eligible for Medicaid under “Family of One” (KK code). A “Family of One”
child/youth who meets the Children’s Waiver eligibility criteria and receives HCBS
and/or HH Care Management, can access other State Plan services such as Private
Duty Nursing, and will continue to meet waiver and Medicaid eligibility requirements.
Figure 3: Disenrollment from waiver if child/youth doesn’t receive monthly HCBS but
continues to meet Children’s Waiver criteria.
Process for Renewing and Establishing Medicaid for Children’s Waiver
Participants
Background – Enrollment in the Children’s Waiver
In preparation for the implementation of the Children’s Waiver on April 1, 2019, a
streamlined process was developed to determine Medicaid eligibility, Children’s Waiver
Home and Community Based Services (HCBS) eligibility, and subsequent entering of
Children’s Waiver Recipient Restriction Exception (RRE) codes (K-codes) for wavier
enrolled children/youth.
Child/Youth with Active Medicaid
When a child/youth has active Medicaid, their HCBS eligibility determination is
performed by the HH CMA’s accessor/care manager, unless the child/youth has opted-
out of HH, in which case the HCBS eligibility determination would be conducted by C-
YES. DOH Capacity Management Team (CMT) receives a report of all completed
HCBS/LOC eligibility determinations. The CMT will review the report for new eligible
children/youth, notify the HHCM/C-YES accessor of slot availability, and enter the
appropriate K-codes into eMedNY to indicate HCBS/LOC eligibility and target population.
The K-code of K1 in eMedNY, indicates to MMCP, the LDSS, HCBS providers, and
others, that the child/youth is eligible and enrolled in the HCBS Children’s Waiver.
Children/youth who are enrolled in HH and want/need HCBS, the HHCM can complete
and determine HCBS/LOC eligibility. If the child’s/youth’s Medicaid recertification is

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 144
upcoming, if there is a concern that the child’s/youth’s Medicaid may lapse, or there is a
need for “Family of One” (KK code) Medicaid budgeting, the HHCM can determine
HCBS/LOC eligibility and work with the LDSS/HRA. The HHCM should not refer an
enrolled HH child/youth to C-YES for HCBS/LOC eligibility. It is imperative that
children/youth are not passed back and forth between HH and C-YES.
Child/Youth without Active Medicaid
When a child/youth who is not enrolled in a HH and does not have active Medicaid
seeks HCBS eligibility, their HCBS eligibility determination must be performed by C-
YES. The CMT receives a report of all completed HCBS/LOC eligibility determinations.
The CMT will review the report for new eligible children/youth and will notify the C-YES
accessor of slot availability. The LDSS is responsible for entering the appropriate K-
codes after the child/youth is determined Medicaid eligible as outlined by Administrative
Directive Memorandum.
Monitoring Active Medicaid Status – Children Enrolled in Children’s Waiver
According to the HH Standards and Requirements of HH, Care Management
Agencies, and Managed Care Organizations, the HHCM must verify an individual’s
Medicaid eligibility/status on a regular basis and prior to billing for services. The HHCM
should be aware of the member’s Medicaid recertification date and should assist the
member/family with Medicaid recertification whenever possible.
More information on the requirements can be found in the Consolidated Children’s
Waiver and Medicaid Case Processing Requirements document.
For children/youth enrolled in the HCBS Children’s Waiver, it is imperative that
HCBS providers verify the child/youth’s Medicaid eligibility plus HCBS enrollment
(through eMedNY), prior to providing services and billing. HCBS providers may not
bill while the child/youth does not have active Medicaid. If the HCBS provider
continues to deliver services while the child/youth’s Medicaid enrollment is not
active, the provider is at risk of not recovering those costs.
Loss of Active Medicaid – Children Enrolled in Children’s Waiver
If an HCBS enrolled child/youth loses their Medicaid, the HHCM or C-YES should
reach out to the LDSS to understand the reason for the loss of Medicaid and to share
with the LDSS that the child/youth is enrolled in the HCBS Children’s Waiver and has
active K- codes. If the family’s financial situation has changed so that they are no
longer eligible for community Medicaid, the LDSS should conduct the “Family of One”
(KK code) Medicaid budgeting to determine Medicaid eligibility for the child/youth,
which, if found eligible, would allow the child/youth to remain in HCBS.
HCBS enrolled children/youth receiving HH care management who lose their Medicaid
should not be referred to C-YES for assistance with Medicaid. It is the responsibility of
the HHCM to assist in restoring active Medicaid status, if possible.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 145
When a member’s Medicaid is no longer active, the HHCM can continue to work with
the member and the LDSS for up to 90 days to assist with the re-establishment of
Medicaid. The HHCM may continue to work with the member but may not bill for
services while the member’s Medicaid is inactive. The HH may retroactively bill for
care management services provided during this 90-day period prior to the date
Medicaid is re-established, if the member is later deemed eligible, enrolled in Medicaid,
and the Medicaid date is effective for this time period. If the HHCM learns that the
member/family’s Medicaid cannot be restored, the HHCM must initiate the HH
disenrollment planning process.
For children/youth receiving HCBS care coordination through C-YES, C-YES may
work with the member/family and/or LDSS to assist with re-establishing Medicaid
eligibility.
For further information, refer to the Children’s Wavier Medicaid Eligibility Status
Impact on HCBS Eligible Children guidance document.
For any questions, please reach out to your lead HH for assistance. DOH Children’s
Transformation contact information: BH.transition@health.ny.gov or
HHSC@health.ny.gov
Medicaid Excess/Surplus Income (Spenddown) Program Guidance for Children’s
Care Management and HCBS
The following information outlines the Medicaid “Spenddown” program and its impact on
Children’s HH care management and/or Children’s Waiver enrollment of HCBS.
What is the Spenddown Program?
The Spenddown program is a way for individuals with income over the Medicaid level
(excess/surplus income) to receive Medicaid coverage. The individual must submit paid
or incurred medically necessary bills equal to or greater than the monthly excess
income amount. The individual may also pay the amount of their monthly excess to the
local district (for upstate residents, the County LDSS, or, for NYC residents, the HRA).
This is called Pay-In.
How Does an Individual Satisfy or Meet Their Monthly Spenddown Amount?
When an individual has a monthly spenddown, it means the individual’s income is
above the Medicaid income limit and must “spenddown” to the Medicaid limit by
submitting paid or unpaid medically necessary expenses, such as out-of-pocket medical
costs (co-pays for doctor appointments and/or pharmacy). The individual can also
choose to pay their monthly spenddown by cash/check/money order directly to their
LDSS/HRA.
• Medically necessary costs and Waiver Services can be utilized for the monthly
spenddown. The family and providers should work with the LDSS/HRA to
understand which service costs can be utilized for spenddown.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 146
• HH care management services cost cannot be utilized for spenddown.
• The individual can pay their spenddown monthly or pay months in advance.
Please note: When a child/youth has Family of One Medicaid budgeting, parental
medical expenses cannot be applied toward a child’s/youth’s spenddown.
When an individual is determined Medicaid eligible with a monthly spenddown, the
individual does not have Medicaid coverage until the monthly spenddown is met.
• Once the individual meets their monthly spenddown, s/he is eligible for Fee-for-
Service (FFS) or regular Medicaid coverage only.
• Individuals participating in the spenddown program are not eligible to join a
MMCP.
What Occurs if an Individual Does Not Satisfy Their Monthly Spenddown
Amount?
If the individual does not meet their monthly spenddown, then services rendered such
as HH care management and other Medicaid services cannot be billed. HHCMs, HCBS
providers, and other Medicaid service providers should work with the family to assist in
meeting their spenddown so services can be delivered. Providers should verify monthly
that the family’s monthly spenddown is met to provide services and be able to bill for
those services.
• If an individual does not meet their spenddown for 90 days or longer, the
LDSS/HRA may close the individual’s Medicaid case, resulting in loss of
Medicaid, Waiver Services, and HH care management services; therefore, care
managers and providers should assist individuals not meeting their spenddown
to avoid disenrollment.
• If an individual loses coverage, the LDSS/HRA, the care manager, and providers
should work to connect the individual to other non-Medicaid services.
Children’s Waiver Participant and Spenddown:
When a child/youth is eligible for the Children’s Waiver and their Medicaid eligibility is
being determined, if they are found Community Medicaid eligible with a spenddown,
then the LDSS/HRA will complete Family of One budgeting. In many cases, the
child/youth found to be eligible for Medicaid through Family of One budgeting won’t
have a spenddown, therefore the required monthly Waiver Services can be delivered
without concern for meeting a spenddown. In some cases, Family of One Waiver-
eligible children/youth will have a spenddown that would have to be met prior to Waiver
Services being provided.
How to Identify an individual Participating in the Spenddown Program:
To systematically identify an individual who has spenddown coverage in ePACES, upon
entering the individual’s Client Identification Number (CIN), the following messages will
come up:
❖ “No Coverage-Excess Income” until the monthly spenddown is met

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 147
Once the individual meets their monthly spenddown, ePACES will reflect the following
message:
❖ “Outpatient Coverage” or
❖ “Outpatient Coverage with Community-Based Long-Term Care”
Outpatient care is sometimes referred to as ambulatory care. It is medical care or
treatment that does not require an inpatient stay in a hospital or medical facility. Some
examples of outpatient services are:
• Treatment and Preventative Health and Dental Care (Doctor, Dentist)
• Eye Exams, Eyeglasses
• Prescription Drugs
• Laboratory and X-Rays
• Medical Supplies
• Care in a Hospital that does not Result in the Individual Being Formally Admitted
to the Hospital for an Inpatient Stay (Emergency Room/Observation)
• Transportation to and from Necessary Medical Services
If the individual meets their monthly spenddown for a six-month period, ePACES will
reflect the following message:
❖ “Full Coverage” or “Community Coverage with Community Based Long-
Term Care (CC with CBLTC)”
Any questions or for further explanation concerning how to meet a monthly spenddown
should be directed to the Medicaid case worker at the individual’s LDSS/HRA. Upstate
and NYC individuals can also contact the Medicaid Help Line at 1-800-541-2831 for
assistance.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 148
Appendix I: HCBS LOC Eligibility Guidance
Care Management Requirements for HCBS Eligible Children
This guidance is to provide clarification regarding Home and Community Based
Services (HCBS) requirements for care managers to ensure HCBS eligible
children/youth obtain the services as required for the child/youth to maintain Waiver
eligible. The 1915(c) Children’s Waiver was implemented on April 1, 2019 and
consolidated the six children’s HCBS waivers into one comprehensive waiver. Each
waiver had nuance differences and different HCB Services. Additionally, with the
consolidated Children’s Waiver now directly connected to HHSC’s program, there are
an increased number of care managers coordinating care for HCBS eligible children,
when previously they had not done so. As such, the following is to clarify the
requirements for services of HCBS eligible children within the Children’s Waiver.
HCBS Level of Care (LOC) Determination:
The new consolidated 1915(c) Children’s Waiver for HCBS requires an annual (365
days) HCBS Level of Care (LOC) Eligibility Re-determination to be completed for the
child/youth to remain in the Waiver and continue receiving Waiver services.
The HHCM or C-YES staff are required to complete this eligibility determination prior to
its annual expiration. The annual re-determination should begin 2 months prior to the
expiration of the current HCBS/LOC determination. It is the HHCM’s or C-YES staff’s
responsibility to know and understand the requirements and necessary paperwork
needed to make an HCBS/LOC eligibility determination. For the target populations of
Developmental Disability in Foster Care and Developmental Disability Medically Fragile,
it is imperative that the HHCM or C-YES staff work with the OPWDD DDROs to
establish timely HCBS redeterminations.
If a child/youth experiences a significant life event, as defined as a significant
impact/change to the child’s or caregiver’s functioning and their daily living situation, a
new HCBS eligibility determination will be needed. With all new HCBS/LOC Eligibility
Determinations, the annual determination timeline resets with the completion of a new
assessment outcome.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 149
If a child/youth enrolled in the Children’s Waiver is hospitalized or placed in an HCBS
restricted setting, then the child/youth can remain enrolled in the Children’s Waiver in
such setting for up to 90 days.
During the 90 days stay:
• For children/youth in a HH, the MAPP segment would be “pended”, and no billing
would occur while the child was in the restricted setting. (Please refer to the HH
Continuity of Care Policy)
• The HH, C-YES or MMCP care manager, as applicable, should notify all care
team members of the child’s/youth’s placement.
• The HH, C-YES or MMCP care manager, as applicable, will stay in contact with
the hospital or HCBS restricted setting and request to be notified 30 days or as
soon as possible, for shorter lengths of stay, prior to discharge.
Length of Stay – 90 days or shorter:
• The HH, C-YES or MMCP care manager, as applicable, will request to be
notified when the child/youth will be discharged.
• Whenever possible, the HH or C-YES staff will conduct a new HCBS/LOC
Eligibility Determination prior to discharge to ensure continuous waiver
eligibility, will update the plan of care, as needed, and link the child/youth to
service upon discharge.
Length of Stay – longer than 90 days:
• Once the child/youth’s length of stay is beyond 90 days, the HH or C-YES staff
will disenroll the child/youth from the Children’s Waiver providing proper
notification to the child/family of the notice of decision, as well as notifying DOH
Capacity Management. (Those with “Family of One” Medicaid based upon waiver
eligibility may lose their Medicaid)
• The HH or C-YES staff will ask the hospital or HCBS restricted setting to notify
when the child/youth is being discharged, if the child/youth will need and want
HCBS upon discharge. An HCBS/LOC Eligibility Determination can be conducted
to determine if the child/youth can be re-enrolled in the Children’s Waiver.
Monthly HCBS Required
Children/youth who meet HCBS/LOC eligibility (target, risk (when needed), and
functional) and obtain a capacity slot, must be connected and in receipt of HCBS on a
monthly basis. The determination of services necessary must be supported by an
assessment of needs and strengths with the child/family and their identified care team
to develop a person-centered POC. The Children’s Waiver offers an expanded array of
service options for children and families. Based on the needs and priorities of the family,
the care manager will link the family with the appropriate services to best support their
needs (including other Medicaid needed services). HCBS found necessary to maintain
the child/youth in their home should be supportive and appropriate for the child/youth’s

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 150
needs. The child/youth’s care record must reflect the needs and necessary services
through appropriate documentation.
If a child/youth has been determined eligible for HCBS and the child/family consents to
receive HCBS, then at least one HCBS must be received monthly to maintain eligibility
for the Children’s Waiver. If the child/youth is not connected to an HCBS upon eligibility
being determined or misses monthly HCBS, then the HH, C-YES or MMCP care
manager, as applicable, must document efforts made to ensure access in the case
record. If there is a concern regarding the child/family’s interest in continuing HCBS and
issues occur regularly, then the HH, C-YES, or MMCP care manager, as applicable,
should review quarterly (three months) HCBS with the child/family and care team to
determine if HCBS should be continued, terminated, or changed and/or if a referral to a
different provider/service is needed.
Monthly HCBS Requirement and Accessibility
Children/youth enrolled in the waiver who need at least one HCBS monthly to safely live
in their home and community must receive the HCBS needed for health, safety, and
welfare. Due to their high needs, children/youth with a Children’s Waiver plan of care
requiring HCBS cannot be placed on HCBS provider’s waitlist for all their identified and
referred HCBS.
If a child/youth has been assessed as needing HCBS to be maintained in the
community, HHCM, C-YES or MMCP must ensure the child/youth has access to the
HCBS outlined on the plan of care. If the child/youth does not have access to monthly
HCBS, then the HHCM, C-YES or MMCP, as applicable, must document efforts made
to ensure access in the case record.
HHCMs, C-YES, or MMCP, as applicable, must make every effort to find available
HCBS and HCBS providers that meet the identified needs of the child/youth. The
child/youth must be referred to another HCBS provider in their service area with the
capacity to serve the child/youth instead of being waitlisted. If the child/family does not
want another provider, the child/youth must receive at least one service monthly or be
in jeopardy of losing their HCBS.
If the HHCM or C-YES staff cannot find available HCBS, then they should contact the
child/youth’s MMCP, if applicable. The HH CMA must contact the lead HH for
assistance to ensure the health and welfare of the child. The lead HH should alert DOH
or the MMCP of the access issue and work with the care manager to provide necessary
services to enrolled children.
If access issues occur regularly, then the HH, C-YES, or MMCP, as applicable, should
review quarterly (three months) HCBS with the child/family and care team to determine
if HCBS should be continued, terminated, or changed. HHCMs and care management
agencies should contact their lead HH with questions or contact the DOH
HHSC@health.ny.gov.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 151
Matching Services to Need
Due to the transformations staggered implementation timeline, children/youth may be
receiving and or referred to multiple services of both the Children’s Waiver and the new
State Plan Services of CFTSS. It is important to ensure that through a person-centered
POC development and service review, that children/youth’s needs are matched with
specific services that they can obtain and regularly receive. This does not prohibit a
child/youth from receiving both State Plan services and HCBS at the same time, as long
as it is reflective of the child/youth’s needs in the person-centered POC and does not
result in duplicative services.
Specifically, community Medicaid eligible children/youth who have all of their needs met
through only State Plan Services of CFTSS or Community First Choice Options (CFCO)
services, should be disenrolled from the Children’s Waiver. In addition, once a
child/youth has been successful in reaching the goal of the HCBS (i.e. Environmental
Modification) and no other HCBS are needed for the child to be maintained in the
community, possible disenrollment from the Children’s Waiver should be reviewed and
determined if other HCBS goals are not appropriate.
Requirements Regarding the Children’s Waiver HCBS Participants Placed in a
Restricted Setting
When a child/youth enrolled in the Children’s Waiver is hospitalized or placed in an
HCBS restricted setting, the child/youth may remain in such setting for up to 90
consecutive calendar days while maintaining enrollment in the Children’s Waiver. If the
waiver child/youth is also enrolled in the HH program when entering an HCBS restricted
setting, the HHCM must “pend” the enrollment segment in the MAPP tracking system.
The HH and HCBS providers are not able to bill while the child/youth is in a restricted
setting, unless otherwise noted below.
When the child/youth remains in a hospital or restricted setting for more than 90
consecutive calendar days, the child/youth must be disenrolled from the Children’s
Waiver. The family/child will be issued a NOD explaining the reason for the
disenrollment from the Children’s Waiver. The HHCM or C-YES will notify the DOH CMT
through the HCS regarding the Children’s Waiver disenrollment following information
outlined in the Communication with DOH Capacity Management for the Children's
Waiver guidance document. The CMT, upon receipt of the notification, will end date the
K-codes on the child’s/youth’s case based upon the date given by the HHCM or C-YES.
In keeping with the Continuity of Care and Re-Engagement for Enrolled Health Home
Members policy, in the 30 days prior to the member’s discharge from the restricted
setting, the care manager must participate in active discharge planning activities to re-
engage the member, the member’s enrollment segment must be changed to ‘active’
status in the MAPP tracking system, and the care management agency may bill for
services provided during the 30-day period. The HHCM must also conduct the
HCBS/LOC Eligibility Assessment 30 days prior to discharge from the restricted setting,

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 152
if possible, or within 30-days after discharge to determine HCBS re-eligibility (if
previously disenrolled from HCBS) and to ensure an updated POC and necessary
services are in place to assist the child/youth in transitioning back to their home and/or
community.
For any questions, please reach out to your lead HH for assistance, DOH Children’s
Transformation contact at BH.transition@health.ny.gov or HHSC@health.ny.gov.
HCBS Determination for Children Discharging from OMH Residential Treatment
Facility or Psychiatric Center
This guidance describes procedures for making 1915(c) Children’s Waiver Home and
Community Based Services (HCBS) referrals for children prior to or after being
discharged from OMH Licensed Residential Treatment Facilities (RTFs) or OMH State
Operated Psychiatric Centers Serving Children (State PCs).
When a child/youth enters an RTF or State PC, the DOH, in conjunction with OMH, is
responsible for (re)determining Medicaid eligibility for the child/youth. When Medicaid
eligibility is established, the child/youth is enrolled in Medicaid under District 97. This
eligibility continues while the child/youth is in the RTF or State PC and continues for the
month of discharge and one month after the month of discharge. This extension is
to prevent a gap in coverage and allow time for the LDSS, NYC HRA to determine
continued Medicaid eligibility.
For children/youth who have Medicaid coverage under OMH District 97, upon return to
their county of residence post discharge, the LDSS will extend Medicaid coverage
beyond the month after discharge, if necessary, to complete a redetermination of
Medicaid eligibility. If the child/youth is not otherwise eligible for Medicaid based on
household income and/or assets, but is eligible for HCBS, Family of One budgeting will
be used to determine Medicaid eligibility. A new Medicaid application is not required
upon RTF/PC discharge in these situations; however, the local district may require
additional information in order to determine the continued eligibility of the child/youth.
Note: Children with SSI Medicaid have uninterrupted Medicaid through a separate
automated process. OMH extends SSI Medicaid for 10 days beyond the OMH Medicaid
district 97 case closing transaction date, and the SSI Medicaid coverage is transitioned
automatically to the discharge District of Fiscal Responsibility (DFR).
When a child/youth enters an RTF or State PC, the OMH Patient Resource Office
(PRO) will complete a Medicaid eligibility determination. There are 3 scenarios to
consider when referring for HCBS and Medicaid Eligibility:
1. Child/youth enters the RTF or State PC with Medicaid
2. Child/youth enters the RTF or State PC without Medicaid and the OMH PRO
determines Medicaid eligibility prior to discharge

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 153
3. Child/youth enters the RTF or State PC without Medicaid and is discharged
before the OMH PRO determines Medicaid eligibility
The following outlines the process for connecting children/youth who are being
discharged to a HH or C-YES for purposes of an HCBS Eligibility Determination and
access to HCBS in each of the three scenarios listed above when an identified need is
established.
Scenario 1: Child/youth enters the RTF or State PC with Medicaid
Children/youth who are enrolled in Medicaid prior to admission to an RTF or State PC
and have an identified need for high level services will be referred to a HH for care
management services and an HCBS Eligibility Determination before being discharged,
when possible. The referral can be made up to 30 days prior to discharge.
• If the child/youth is already connected to HH care management agency and or
HCBS, a new referral is not needed if the child/youth has been inpatient for 90
days or less. Contact with the current HH provider is needed.
HHCMs are permitted to serve a child/youth 30 days prior to discharge to assist with
discharge planning, to secure services, and to establish HCBS eligibility. If a child/youth
in an RTF or State PC needs HCBS in order to be safely discharged to their home and
community, then the HCBS/LOC Eligibility Determination must be completed before
discharge. Coordination between the RTF or State PC and the HH is necessary to
ensure children/youth are safely discharged.
In circumstances when the child/youth is referred to a HH after discharge, such as when
the child’s length of stay is less than 30 days, or when there is a change in the
child/youth’s discharge plan, the child should be enrolled in a HH immediately. The HH
must complete an HCBS eligibility determination within 30 days of the referral.
Scenario 2: Child/youth enters the RTF or State PC without Medicaid and the OMH
Patient Resource Office (PRO) determines Medicaid Eligibility before discharge
Children/youth who are enrolled in Medicaid prior to discharge will be referred to a HH
for care management services and an HCBS eligibility determination. Once Medicaid
eligibility is established by OMH, the referral can be made up to 30 days prior to
discharge.
Once Medicaid is established by OMH, HHCMs are permitted to serve a child/youth
immediately to assist with discharge planning, to secure services, and to establish
HCBS eligibility. If the RTF/State PC unable to make a referral to the HH 30 days prior
to discharge, the referral should be made immediately with the information regarding the
discharge date. Once the referral to HH is made (which may occur at the time of
discharge), the HH will need to work with the child/youth/family and the RTF or State PC
to ensure proper documentation and information is obtained to complete the HCBS/LOC
Eligibility Determination.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 154
It is imperative that the HHCM remembers that the Medicaid eligibility established by
PRO under District 97 continues only for the month of discharge and one month after
the month of discharge. The HHCM will need to ensure that HCBS/LOC eligibility is
completed prior to Medicaid eligibility ending and the DOH Capacity Management is
notified to enter the proper Recipient Restriction K-codes to ensure that if the Local
District needs to conduct Family of One budgeting, they will be aware of the HCBS
eligibility.
Scenario 3: Child/youth enters the RTF or State PC without Medicaid and the OMH
Patient Resource Office (PRO) cannot determine Medicaid Eligibility before
discharged
Up to 30 days prior to discharge, but no later than the date of discharge, the RTF or
State PC will refer children/youth who are not already enrolled in Medicaid or cannot be
determined Medicaid eligible under District 97 to C-YES for an HCBS Eligibility
Determination and assistance with the Medicaid eligibility application.
Responsibilities of Each Party Involved
To ensure adequate services are available upon discharge and uninterrupted Medicaid
coverage for children who may not be otherwise eligible for Medicaid, coordination is
essential and the sharing of information critical for a successful transition.
RTFs/State PCs
1. Determine when a child/youth will be ready for discharge.
2. As soon as possible, up to 30 days prior to discharge, work with the
family/caregiver to identify their preferred HH or HH CMA and make a direct
referral. If Medicaid will not be established prior to discharge, then make a
referral to C-YES.
3. At time of referral, indicate Medicaid eligibility status and potential discharge
date.
4. When a HH/C-YES care manager is assigned, ensure all necessary
documentation is provided and forms are complete to facilitate completion of an
HCBS Eligibility Determination (i.e. Diagnosis, Disability, LPHA form, etc.).
5. Continue to work collaboratively with the HH/C-YES care manager to ensure a
seamless transition to the community and access to needed services.
6. Please note: For children who are being discharged from an RTF or State PC
and are in foster care, it is expected that there is enhanced collaboration with the
LDSS and the Voluntary Foster Care Agency, if applicable, to ensure access to
needed Medicaid services and to promote a safe and stable discharge. For
children in foster care, the LDSS will enroll them in Medicaid using the foster care
Medicaid rules.
OMH Patient Resource Office (PRO) and LDSS
1. For children/youth who have been determined Medicaid eligible by the OMH
PRO, OMH PRO will transition the OMH Medicaid (District 97) case to the LDSS
District of Fiscal Responsibility.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 155
a. For SSI Medicaid eligible children/youth, PRO will transfer the OMH
Medicaid coverage to the new district through the Auto-State Data
Exchange (SDX) process.
b. For all other children/youth:
i. PRO will initiate the closing of the child/youth’s OMH Medicaid
case.
ii. PRO will change the child/youth’s residence address to their
discharge address, and a closing notice will be sent to this the
discharge address. The notice will advise that the coverage will be
transferred to the new district and will identify the effective date that
the OMH Medicaid case will end.
iii. PRO will mail a Relocation Referral Form and pertinent case
information to the Medicaid Director in the new district of residence.
iv. The Relocation Referral Form sent by the PRO will indicate
whether the child is enrolled in Waiver services or that a referral
has been made.
2. Upon receipt of the Relocation Referral Form, the LDSS District of Fiscal
Responsibility (DFR) will establish uninterrupted coverage for the case,
transitioning the Medicaid coverage from OMH Medicaid to the county.
3. LDSS District of Fiscal Responsibility (DFR) will issue the appropriate opening
notice.
4. DOH will notify the LDSS of the approval for HCBS eligibility and enter the
appropriate Recipient Restriction K-code on eMedNY to indicate participation in
the Children’s Waiver. This will provide necessary information to the LDSS for
purposes of redetermining Medicaid eligibility for the child/youth; including the
authorization to use Family of One budgeting, if necessary.
C-YES
1. The RTF or State PC will refer children/youth to C-YES who are not already
enrolled in Medicaid or cannot be determined Medicaid eligible under District 97
for an HCBS Eligibility Determination and assistance with the Medicaid eligibility.
a. The assigned C-YES family support worker will contact the RTF/State PC
48 hours after they are assigned to notify the referring RTF/State PC of
the assignment.
b. C-YES will gather the necessary information to follow up with the family
prior to the discharge of the child/youth, whenever possible.
c. C-YES will stay in contact with the RTF/State PC staff who can assist with
necessary information and the LPHA form to conduct the HCBS/LOC
Eligibility Determination.
d. C-YES must also notify the RTF/State PC assigned OMH Patient
Resource Office (PRO) when a child is determined eligible for HCBS.
e. When developing the person-centered POC and referring to HCBS, C-
YES will notify HCBS providers that the child/youth was discharged from
the RTC/State PC.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 156
f. C-YES must follow their established processes in addition to the steps
outlined above.
Health Home
2. The RTF or State PC will refer children/youth to HH who have Medicaid eligibility
prior to entering care or if PROs established OMH District 97 Medicaid eligibility
prior to or at discharge for an HCBS Eligibility Determination.
a. After verifying Medicaid eligibility, the assigned HHCM will contact the
RTF/State PC 48 hours after they are assigned to notify the referring
RTF/State PC of the assignment.
b. HHCM will gather the necessary information to follow up with the family
prior to the discharge of the child/youth, whenever possible.
c. The HHCM will schedule an appointment to meet with the child/youth,
family, and RTF/State PC staff to gather the necessary information to
conduct the HCBS/LOC Eligibility Determination and complete appropriate
consents.
d. If the child/youth is determined HCBS eligible, the HHCM will follow the
HCBS process to obtain a slot with Capacity Management and issue the
appropriate Notice of Decision.
e. The HHCM must also notify the RTF/State PC assigned OMH Patient
Resource Office (PRO) when a child is determined eligible for HCBS. This
notification will be made prior to the child’s discharge, wherever possible,
and no later than 30 days from the date of the referral.
f. When developing the person-centered POC and referring to HCBS, the
HHCM will notify HCBS providers that the child/youth is being discharged
from the RTC/State PC to ensure the first appointment and services are in
place after discharge, whenever possible.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 157
APPENDIX J: HEALT H HOME SERVING CHILDREN POLICY
INFORMAT ION
Health Home Policy Document
Description
Comprehensive Assessment Policy
Establishes standards and guidance regarding the
Health Home comprehensive assessment that is
required for all Health Home enrollees
Health Home Quality Management Policy
Describes the scope and required procedures for
continuous quality improvement, monitoring, and
oversight within the Health Home network
Health Home Notices of Determination and
Fair Hearing Policy
Outlines the policies and procedures for issuing Notices
of Determination for Health Home enrollment and the
steps for requesting and attending a Fair Hearing
Health Home Monitoring: Reportable
Incidents Policies and Procedures
Defines the requirements for Health Homes to identify,
receive, investigate, resolve and record Reportable
Incidents, including a continuous quality improvement
process to track and identify trends to reduce risk and
minimize the potential for future occurrence of the same
or related incidents
Health Home Plan of Care Policy
Outlines standards and guidance for Plans of Care
(POCs) completed by Health Home Care Managers
Access to/Sharing of Personal Health
Information (PHI) and the Use of Health
Home Consents
Lists the various Health Home consents requirements
and policies/procedures related to PHI protections
Health Home Care Management Activities
and Billing Protocols for Managing Newly
Referred Individuals from Excluded Settings
Addresses steps that must be taken to manage new
referrals from excluded settings of potentially eligible
Health Home and/or HCBS children/youth
Conflict Free Case Management Policy
Outlines the federally guided principles of Conflict Free
Case Management (CFCM) and implementation
strategies for each

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 158
Appendix K: Waiver Performance Measures
The following table lists performance measures as identified in the 1915(c) Children’s
HCBS Waiver that are pertinent to HH/C-YES Care Managers and HCBS Providers.
The performance measures noted in this appendix section are not inclusive of all
performance measures and quality metrics required by the Waiver and monitored by
DOH. For a full list of all required reporting measures and metrics,
please see the Waiver.
Performance Measure
Relevant Party
Waiver
Appendix
An evaluation for LOC is provided to all applicants for whom
there is a reasonable indication that services may be needed
in the future. The percent of children that met initial LOC
requirements prior to receiving services.
HH/C-YES Care
Managers & HCBS
Providers
B
The processes and instruments described in the approved
waiver are applied appropriately and according to the
approved description to determine participant LOC. The
percent of annual LOC forms/instruments completed as
required in the approved waiver.
HH/C-YES Care
Managers
B
Performance Measure: The processes and instruments
described in the approved waiver are applied appropriately
and according to the approved description to determine
participant LOC. The percent of LOC forms/instruments
completed as required in the approved waiver.
HH/C-YES Care
Managers
B
Percent of waiver providers providing waiver services who
meet designation, licensure, and certification requirements
continuously.
HCBS Providers
C
Percent of waiver providers providing waiver services who
meet designation, licensure, and certification requirements
prior to furnishing waiver services initially.
HCBS Providers
C
Percent of waiver providers providing waiver services who
have an active agreement with the State to provide Medicaid
services if they are FFS, or an active agreement with the State
to provide Medicaid services and an active agreement with the
MCO if they are MC.
HCBS Providers
C
Percent of providers of waiver services who meet training
requirements during the Children’s Waiver re/designation
process (Non-Certified/Non-Licensed).
HCBS Providers
C
Percent of providers of waiver services who meet training
requirements during the Children’s Waiver re/designation
process (Certified/Licensed).
HCBS Providers
C
Percent of participants reviewed with a POC that contains
interventions/strategies that were adequate and appropriate to
their needs and goals (including health goals) as indicated in
the assessment(s).
HH/C-YES Care
Managers
D

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 159
Performance Measure
Relevant Party
Waiver
Appendix
Percent of participants reviewed with a POC that has
adequate and appropriate strategies to address their health
and safety risks as indicated in the assessment(s).
HH/C-YES Care
Managers
D
Percent of participants reviewed with a POC that addressed
the participant’s goals/needs as indicated in the
assessment(s).
HH/C-YES Care
Managers
D
The percent of POC forms/processes completed as required
in the waiver.
HH/C-YES Care
Managers
D
Percent of participants whose POC was updated within 365
days of the last POC evaluation.
HH/C-YES Care
Managers
D
Percent of participants whose POC was updated as warranted
by changes in the participant’s needs.
HH/C-YES Care
Managers
D
Percent of new participants receiving services according to
their POC within 45 days of approval of their POC.
HH/C-YES Care
Managers
D
Percent of participants who received services in the type,
amount, duration, and frequency specified in the POC.
HH/C-YES Care
Managers & HCBS
Providers
D
Percent of participant records reviewed with a completed
signed freedom of choice (FOC) form that specifies choice
was offered among waiver services and providers.
HH/C-YES Care
Managers
D
Percent of participant records reviewed with a POC that
includes the participant’s and/or guardian/caregiver’s
signature as consistent with State and Federal guidelines.
HH/C-YES Care
Managers
D
Number and percent of substantiated cases of abuse, neglect,
exploitation, and unexplained death where recommended
actions to protect the participants health and welfare were
implemented.
HH/CYES Care
Managers & HCBS
Providers
G
Percent of reports related to abuse, neglect, exploitation, and
unexplained death of participants where an initial action to
protect the health and welfare of the child or an investigation
was initiated within the established timelines.
HH/C-YES Care
Managers & HCBS
Providers
G
Percent of waiver participants enrolled who have contact with
their care manager consistent with the waiver guidelines.
HH/C-YES Care
Managers & HCBS
Providers
G
Percent of appeals and state fair hearings filed by participants
that were resolved according to approved waiver and State
guidelines.
HH/CYES Care
Managers & HCBS
Providers
G
Percent of participants who received information on how to
report suspected abuse, neglect, exploitation, or unexplained
death according to policy.
HH/C-YES Care
Managers & HCBS
Providers
G
Number and percent of participant incidents that were
reported, reviewed, and submitted to DOH within required
timeframes, as specified in the approved waiver.
HH/C-YES Care
Managers & HCBS
Providers
G
Number and percent of unauthorized uses of restrictive
interventions, including restraints and seclusion, that were
appropriately and timely reported per guidance.
HH/C-YES Care
Managers & HCBS
Providers
G

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 160
Performance Measure
Relevant Party
Waiver
Appendix
Number and percent of Children’s Waiver participants who
received annual physical exams or a wellness exam per
guidelines.
HH/C-YES Care
Managers
G
Percent of FFS claims paid using FFS rates that follow the
rate methodology in the approved waiver application.
HCBS Providers
I
Percent of claims paid only for services rendered when
participants were enrolled in the waiver and eligible for such
services, and when the services were provided by a qualified
provider.
HCBS Providers
I
Percent of MC Children’s Waiver payments paid consistent
with the payment and rate methodologies in the approved
waiver.
MCO/ HCBS Providers
I
Percent of FFS claims and MC encounters paid in accordance
with the waiver’s approved rates and methodologies.
MCO/ HCBS Providers
I
Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 161
Appendix L: K-Codes RR/E for the Children’s Waiver
Members enrolled in the HCBS Children’s Waiver will have Recipient
Restriction/Exemption (RR/E) codes, identified as “K-codes” to indicate which
children/youth are enrolled in waiver services and their specific population category.
RR/E
Code
R/RE Code Description
K1
HCBS LOC
K3
HCBS Serious Emotional Disturbance (SED)
K4
HCBS Medically Fragile (MF)
K5
HCBS Developmentally Disabled and Foster Care (DD & FC)
K6
HCBS Developmentally Disabled and Medically Fragile (DD & MF)
K9
Foster Care
KK
Family of One
A1
Children’s Health Home: indicates the member is in outreach or enrolled with a
Care Management Agency
A2
Children’s Health Home: indicated the member is in outreach or enrolled with a
Health Home
If an MMCP receives an HCBS claim for a child/youth whose RR/E K-code cannot be
verified, the MMCP should deny the claim for lack of verification of Children’s Waiver
eligibility, enrollment, and approved service. Children’s HCBS providers and MMCPs
should coordinate with the child/youth’s care manager to ensure that the appropriate K-
code is on the child/youth’s file and enrollment in the 1915(c) Children’s Waiver is
confirmed. HCBS providers should also be mindful of timely filing timeframes when
submitting claims to MMCPs.
If a member’s RR/E K-codes are missing or incorrect, the HCBS provider contacts the
HHCM or C-YES. The HHCM or C-YES is responsible for ensuring proper Children’s
Waiver K-codes and will communicate any K-code issues to the DOH Capacity
Management.

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 162
Appendix M: Billing and Claiming Resources
The following lists resources that HCBS providers, HHCMs, and Medicaid Managed
Care Plans may find useful.
Resource
Description
NPI Number Webinar
Guides agencies through the application process for
an NPI number and explains a general overview of the
significance and utility of the NPI number
Medicaid Provider Enrollment for New
Children's SPA and HCBS Providers
Walks through the steps providers need to take to
enroll as a Medicaid provider to bill and be reimbursed
by Medicaid
Understanding Paper Claims
Submissions
Reviews the steps for submitting paper claims and
walks through each component of the UB-04 claim
form
Principles of Revenue Cycle
Management and Utilization Management
Provides background information, definitions,
tips/tools related to revenue cycle management and
utilization management
Billing Tool
An interactive UB-04 form that walks through the
components required to submit a clean claim

Children’s Home and Community Based Services (HCBS) Manual
Appendix N: Allowable Billing Combinations
NYS Allowable Billing Combinations of Children’s Behavioral Health, Children and Family Treatment and Support Services and HCBS
HCBS
OMH
Clinic
OASAS
Clinic
OASAS
Opioid
Treatment
Program
OMH
Youth
ACT*
OMH
PROS**
OMH
CDT**
OMH
Partial
Hospital
OASAS
Outpatien t
Rehab
CPST/
OLP
PSR
FPSS
YPST
Day Habilitation
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Community
Habilitation
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Caregiver/Famil
y Advocacy and
Support
Services
Yes
Yes
Yes
No
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Respite
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Prevocational
Services
Yes
Yes
Yes
No
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Supported
Employment
Yes
Yes
Yes
No
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Palliative Care Pain
& Symptom
Management
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Palliative Care
Counseling and
Support Services
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Palliative Care
Massage Therapy
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Palliative Care
Expressive Therapy
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Adaptive and
Assistive Technology
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes

Children’s Home and Community Based Services (HCBS) Manual
VERSION 2023-1 MARCH 2023 PAGE | 164
* Youth ACT has care management built in and is considered an all-inclusive program for Mental Health. As such, on-going co-enrollment with
HCBS is not allowable because of the care coordination of both services except for 30 days prior to discharge from Youth ACT.
**These services are available to youth aged 18 and older

